Introduction
The coronavirus disease 2019 (COVID-19) pandemic is a public health emergency of international concern. Understanding the trajectory of severe acute respiratory syndrome 2 (SARS-CoV-2) and the duration of infectivity has a critical importance in controlling the pandemic.1) There is substantial uncertainty regarding virological levels (i.e. detection and viral load) in patients and how this relates to infectivity and disease severity. Information regarding SARS-CoV-2 detection and viral load at different time points of an infection will aid clinical interpretation of real-time reverse transcriptase polymerase chain reaction (rRT-PCR) test results. Furthermore, information pertaining to the duration of infectivity will help to create and update public health protocols for quarantine, isolation and contact tracing.2 Besides, it will allow a better reallocation of resources and it will prevent situations like the one we will report. In this article, we present a case of unlikely SARS-CoV-2 reinfection with devastating consequences for the patient, and we discuss the latest evidence about interpretation of PCR results. This knowledge should be reinforced to prevent poor test decisions and avoid other concerns.
Case Report
In June, a 40-year-old woman was admitted to hospital with fever and cough. She had been in usual state of health until four days before admission, when a dry cough developed. She was referred to our emergency department by her hemodialysis clinic, because fever was detected before beginning regular treatment session.
The patient had a history of Joubert syndrome, a disorder with a wide range of features. In our patient case, it caused a chronic renal disease. For this reason, she initiated hemodialysis about three years ago in an extra-hospitalar clinic and was registered on renal transplantation waiting list.
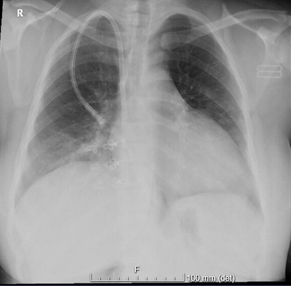
On examination, the temperature was 37.1ºC, the heart rate was 94 beats per minute, the blood pressure 133/91 mmHg, the respiratory rate 16 breaths per minute, and the oxygen saturation 99% while the patient was breathing ambient air. The patient appeared to be well and in no distress. Laboratory test results are shown in Table 1. Rapid nucleic acid testing of a nasopharyngeal swab was positive for SARS-CoV-2. A chest radiograph showed clear lungs, without evidence of focal airspace consolidation or pulmonary edema (Fig. 1).
Table 1: Laboratory data.
| Variable | On admission | Reference range |
|---|---|---|
| Hemoglobin (g/dL) | 10,9 | 12-15 |
| White cells (per μl) | 5000 | 4500-11500 |
| Neutrophiles (per μl) | 3800 | 2000-7500 |
| Lymphocytes (per μl) | 800 | 1500-4000 |
| Monocytes (per μl) | 400 | 200-1000 |
| Eosinophiles (per μl) | 100 | 100-600 |
| Platelet count (per μl) | 137.000 | 150.000-450.000 |
| Sodium (mmol/L) | 139 | 135-145 |
| Potassium (mmol/L) | 4.0 | 3.5-5.0 |
| Lactate dehydrogenase (U/L) | 388 | 120-246 |
| C-Reactive Protein (mg/dL) | 14.87 | <0.5 |
The patient was admitted to a dedicated COVID-19 hospitalization area, since there was no other place out of hospital capable to provide dialysis under isolation measures. During the stay, she maintained fever for six days, but no other symptom appeared. On hospital day 11, new nucleic acid testing of nasopharyngeal swab was negative. In order to accomplish cure, another swab test was made after 24 hours with the same result. Despite that, her husband remained positive. Because the lack of capacity to undertake domiciliary isolation, she stayed in hospital. This option was made to protect patients of extra-hospitalar hemodialysis clinic. After 4 weeks, her husband finally tested negative. Excessive caution motived another swab test before discharged, which was negative. Finally, she came back to community.
Four weeks later, she was going to receive a kidney transplant from a deceased donor at a reference center for kidney transplantation, but, at admission, she was tested again for SARS-CoV-2 and the result came out positive. At that time, there was no evidence of acute infection. Patient was asymptomatic and C-reactive protein levels remained low. After that, surgery was cancelled, and she was transferred back to her local hospital to undergo dialysis in isolation.
Discussion
It is known that PCR tests positivity range as time since exposure. Namely, over the 4 days of infection before the typical time of symptom onset (day 5), the probability of a false-negative result in an infected person decreased from 100% on day 1 to 68% on day 4. On the day of symptom onset, the median false-negative rate is 38%. This then decreases to 20% on day 8 (3 days after symptom onset) beginning to increase again, from 21% on day 9 to 66% on day 21.3 Overall, PCR tests sensitivity is about 70%, while specificity is 100%, so, while positive tests for COVID-19 are clinically useful, negative tests need to be interpreted with caution, taking into account the pre-test probability of disease.4 Pre-test probability must take in account days since symptoms onset, as previous mention. On the other hand, there are a lot of reports of cases that continues to be positive several weeks after infectious. It was documented a case that remained positive for 83 days.5 Although, there are several international papers which support the notion that early reinfection does not occur and patients who test positive again for SARS-CoV-2 are not infectious. This was first reported by Korean researchers. They had identified 447 patients who again tested positive on real-time reverse transcriptase-polymerase chain reaction testing for viral RNA. To help determine whether a positive result on a second test is associated with infectivity, the Korean researchers investigated 790 contacts of 285 patients who tested positive a second time. Among the contacts, the researchers identified three new cases. However, for all three patients, other sources of infection were possible. Furthermore, the researchers tried to culture virus from 108 patients who tested positive a second time, but all cultures were negative. Authors concluded that there was no evidence of infectivity of re-positive cases.6) In an even more relevant way, Germans researchers found that the virus collected from patients after 8 days of illness did not grow in culture or yield subgenomic mRNA which is only present when a virus is replicating.7) Another study suggest that transmission may even be limited to five days after symptom onset. The authors traced 2716 close contacts of COVID-19 patients, and they did not find any case among 852 contacts who were exposed later of 5 days of symptom onset.8) Indeed, it is set that infectious potential belong between day 3 before symptomatic onset and 5 days after that.2
So, in our opinion, the case we reported do not represent a true reinfection and patient was not contagious. Thus, she should not have been tested. The rules in vigour at that time, concretely rule number 13 from Portuguese Directorate-General of Health (DGS),9 says that all asymptomatic patients with a history of past SARS-CoV-2 infection who had cure criteria set out in DGS rule number 4/202010 are dismissed from carrying out another laboratory test. Once again, the patient was contacted by the public health unit, and it was not possible to ascertain any new source of infection. Furthermore, she would test negative again 4 days after. Despite that, there was reports about cases of true reinfection. Genomic, epidemiological, clinical and serological analyses confirmed that the patients had re-infection instead of persistent viral shedding.11,12
Currently, there is a Portuguese rule about testing national strategy that clarifies this issue and it is according with evidence. So, patients with history of infection by SARS-CoV-2 laboratory confirmed in the past 180 days should not undertake another test unless they are immunosuppressed, or they have concomitantly symptoms, high risk contact with COVID-19 patient and there is not another diagnosis that can explain the clinical case.13
Today, another point of discuss is about cured patients with needing of immunosuppressing treatment for cancers or transplants, such as our patient. There is a fear of viral reactivation in these patients. A research followed 39 patients with positive antibodies anti-SARS-CoV-2 and PCR test negative. After chemotherapy, all patients remained negative for SARS-CoV-2, without suspicious changes on chest computed tomography.14 Nevertheless, it was related a possible reinfection in a patient who was undergoing treatment to B cell acute lymphloblastic leukemia. The authors think that given the short time frame from leukemia treatment to PCR positivity and the low case rate in mid‐June in New York City, reinfection appears to have been unlikely and SARS‐CoV‐2 reactivation is a possible explanation. They believe it illustrates the risks of treating recently recovered COVID‐19 patients with immunosuppressive therapy, particularly lymphocyte and antibody‐depleting therapy.15 Despite that, it is important to note that there was not viral genomic analysis supporting their conclusion. Taking in account that there was not any another similar case related and there is a lot of studies showing that the virus does not replicate even in an appropriately microbiological culture after 8 days, we think that reinfection is more likely.
Conclusion
In conclusion, we think that clear recommendations should be established and reinforced worldwide. Moreover, we believe that patients who need immunosuppression for any reason must do it about 1 week after symptoms onset. We base our opinion in studies that shows the virus is not viable a few days after symptoms onset. Besides, until 180 days past infection we think there is no need to do any test. Albeit there are some fears which are acceptable taking in account the lack of evidence, we believe the benefits outweigh the risks for most patients. On the other hand, ethical issues arise since there is a duty to transplant the person who will benefit the most from it.