Introduction
In recent years, average life expectancy has increased in OECD countries.1 Concomitantly, regional inequalities in health outcomes have begun to emerge in these countries. In general, they proved to be lower in what concerns population living in a rural environment.2 In addition, there are also differences motivated by intrinsic regional factors, such as diet.3
This issue has also been raised in Portugal. In fact, in 1996, a pioneering study demonstrated that the increase in distance negatively influences the use of hospital services.4 More recently, the same author concluded that regional disparities continued to occur, mainly between urban coastal areas and the rural interior.5 In this segment, an article stands out, showing that distance to hospital has a significant impact on access to emergency services, contrary to the increase in user fees.6
The impact of geographic and sociodemographic factors
A study carried out in North Carolina showed that the possession of a driving license and the distance travelled to the health provider had an impact on the use of regular medical care.7 Another one showed that distance also has an impact on the use of emergency services.8 On the other hand, a study in the state of Ohio did not find a significant correlation between distance and mortality from heart disease. Still, poverty rate and rurality were significantly associated with mortality.9
The aforementioned articles end up capturing cases of low severity, even if the focus is on the emergency service, because their misuse is an internationally disseminated problem.10 In order to circumvent this problem, some studies have focused their analysis on time responses from pre-hospital facilities. They conclude that a longer response time is associated with higher mortality rates, particularly in rural areas.11 It is relevant to note that there are other social factors that motivate the delay in providing care such as gender, age and race.12 Similarly, researchers from Pennsylvania found a significant difference in mortality from cardiorespiratory arrest, as it occurred in rural areas (91%) and urban areas (77%)13 Another study analyzed the lethality rate for road accidents in all Italian municipalities between 2000 and 2012 and it was concluded that the increase in the distance by 1 km increases the probability of death by 0.18%14 Another publication showed that a 1-minute increase in driving time arrival at the emergency department a 17% increase in 90 days-mortality.15
In this way, investigations observed that closing hospitals improves overall efficiency, in spite of admitting that it can lead to increased mortality in urgent situations.16,17 However, a study carried out in California found no difference in mortality related to the increase in distance resulting from the closure of services.18 A recent work carried out in Sweden on the closure of 16 emergency services showed a decreased likelihood of survival from a myocardial infarction, but only during the first year after closure of a particular service.19
Objective
This study has two main goals: assessing the impact of distance to the polyvalent emergency service and the contribution of less differentiated services (medical and surgical or basic) to the mortality of critically ill patients.20
The relevance of this study is related to the inexistence in Portugal, at least to our knowledge, of a scientific basis for the planning of emergency services. This organization results mainly from historical roots, related to hospital localization and experts’ opinions. In fact, the most extensive document on this issue is the National Urgency and Emergency Network's Reevaluation Report, prepared by a commission appointed by the Ministry of Health.21 This encompasses a relevant evaluation of the network, but does not present new scientific research. Furthermore, this report appoints that in the last fifteen years there was an intense debate about Urgency and Emergency network and after that lists twenty-two significant published documents. However, it should be pointed that none of those represents a classic scientific work with clear investigation question, data and hypothesis tests.
In order to understand our analysis, it should be noted that Portuguese emergency services are divided into three essential levels, hereby presented in decreasing order of differentiation: Polyvalent Emergency Service (PES), Medical and Surgical Emergency Service (MSES) and Basic Emergency Service (BES).22 These different levels of responsibility run in a network. In order to streamline the referral process, green pathway systems have been created for pathologies in which time is crucial for therapeutic success.
I believe that Viseu PES brings together the ideal characteristics for the pursuit of previously outlined objectives. On the one hand, it has a large reference area, with different road accesses. On the other hand, it constitutes a reference center for three BES (based in São Pedro do Sul, Tondela and Moimenta da Beira) and two MSES (placed in Guarda and Covilhã).23
Material and Methods
Study design and setting
It was used a retrospective design whose sample contains 2812 participants. The study includes only patients admitted to the resuscitation room of Viseu PES, from 1 January to 31 December 2019. Patients who died before reaching the hospital were excluded.
Since the beginning of 2018 there has been a team of doctors dedicated to PES in Viseu.22 All of them are specialists in internal medicine and they have competence in emergency medicine attributed by Portuguese Medical Association. This is responsible for the initial approach of all patients admitted to the resuscitation room and has recorded information related to each case, namely the number of the clinical file and the presumed diagnosis on admission. This room is the end-of-line emergency center for critically ill patients from the entire region of Viseu, Guarda and Covilhã.
In order to develop the study, the approval of the PES director, Ethics Committee and Board of Administration of Centro Hospitalar Tondela-Viseu (CHTV) were obtained.
Variables
Regarding the study variable, we chose 30-day mortality to assess the outcome of the emergency episode. The time option was due to the balance between two factors. First, we believe that this temporal measure already correlates strongly with long-term prognosis.24 Second, we believe that applying a shorter period of time would not fully assess the impact of the initial episode.
Concerning to explanatory variables, it was started by defining the estimated travel time in minutes from the center of each of the municipalities to SUP in Viseu.23 For this purpose, it was used the Google Maps application.25 In addition to this, it was added the variables gender and age to adjust the results. Furthermore, it was created two dummy variables related to belonging to a municipality in the area of influence of basic emergency services or medical and surgical emergency services.
Finally, another variable was created concerning pathological groups, conditions that have been previously identified as time-sensitive,14,18-20 which are described in Table 1. This variable was used to perform subgroup analysis.
Table 1: Contingency table between the diagnosis and mortality groups.
| Death after 30 days | ||||
|---|---|---|---|---|
| Not | Yes | Total | ||
| Diagnostic group | Stroke | 508 | 80 | 588 |
| Acid-base and electrolyte changes | 102 | 23 | 125 | |
| Myocardial infarction with Supra-ST | 98 | 14 | 112 | |
| Digestive bleeding | 62 | 15 | 77 | |
| Intoxication | 49 | 0 | 49 | |
| Other | 320 | 33 | 351 | |
| Other major cardiovascular events | 470 | 36 | 506 | |
| Cardio-respiratory arrest | 6 | 74 | 80 | |
| Respiratory problems | 439 | 205 | 644 | |
| Sepsis | 49 | 34 | 83 | |
| Trauma | 171 | 24 | 195 | |
| Total | 2274 | 538 | 2812 | |
Collection of information and construction of the database
In order to extract the necessary data, it was necessary to cross-check the information in the record books with administrative data (SONHO database) and clinical data (ALERT database→). SONHO database is an administrative database where the patient’s address, patient’s exemption status and patient’s origin within the Health System are recorded. ALERT database is a clinical database where the patient’s Manchester Triage classification, among other clinical information related to the emergency service visit, is recorded.6 Thus, when collecting information from each patient, the number of the clinical file recorded in the emergency book was crossed with the data from SONHO database, therefore obtaining age, gender, date of death (if applicable) and place of residence. Very rarely, it was found that this location did not belong to the area of the influence of the PES or the upstream emergency service. These cases correspond to people passing through or who have not yet changed their residence. In these, and in an effort to encompass all episodes, clinical records were consulted because they often indicate the location in which the episode happened, allowing us to complete this information. Even so, cases in which this was not possible were excluded. Then, in order to fit the patient into one of the aforementioned diagnostic groups, it was again necessary to consult the record book. In cases where the information recorded was insufficient, there was a need to consult the episode on ALERT→ or hospital clinical reports, such as discharge notes. The entire process described above required an exhaustive and individualized analysis of each patient's data, based on access to a unique and original source of records. Finally, and in order to complete the database, the formulas IFS, IF and OR, of the Microsoft Excel→ were used for the dummy variables referring to MSES and BES influence counties and, finally, to define travel time according to the municipality of residence. This process resulted in a working file with 2812 observations.
Data analysis method
Initially, descriptive statistical measures of the variables under study were obtained, namely mean, minimum and maximum values. For this purpose, Microsoft Excel® and IBM SPSS®, version 27, were used.
Subsequently, it was used the last program mentioned to estimate several models of binary logistic regression. All have in common the adjustment for age and gender and death after 30 days as a dependent variable. As a reference value for the rejection of the null hypothesis, a significance level (α) ≤ 0.05 was used. Even so, significance levels of (α) ≤ 0.10 are also commented.
Results
Descriptive analysis of variables
Among the 2812 observations under study, there were 1510 male users (54%) and 1302 female users (46%). As for the population residing in areas of influence of other levels of emergency services, 170 of the registered cases (6%) come from reference areas of Guarda or Covilhã MSES, respectively, 147 and 23 users. On the other hand, 859 (30%) live in areas served by BES (140 from Moimenta da Beira, 318 from São Pedro do Sul and 410 from Tondela reference area). There is also the existence of 923 cases (33%) that neither reside in reference areas of MSES nor in municipalities covered by BES.
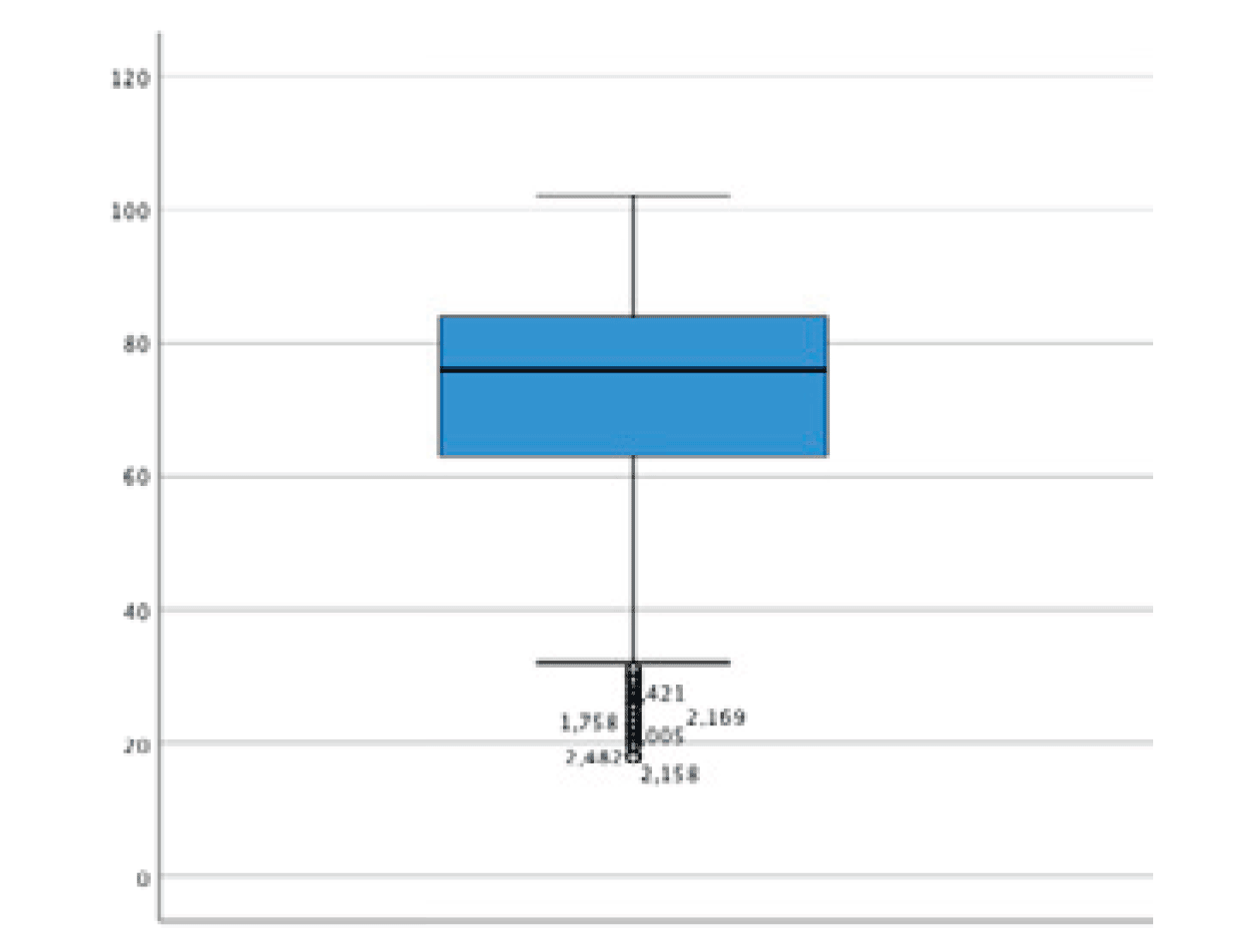
Regarding age, the mean was 72.29 years (standard deviation of 16.429 years). The minimum recorded was 18 and the maximum 102 years (Fig. 1).
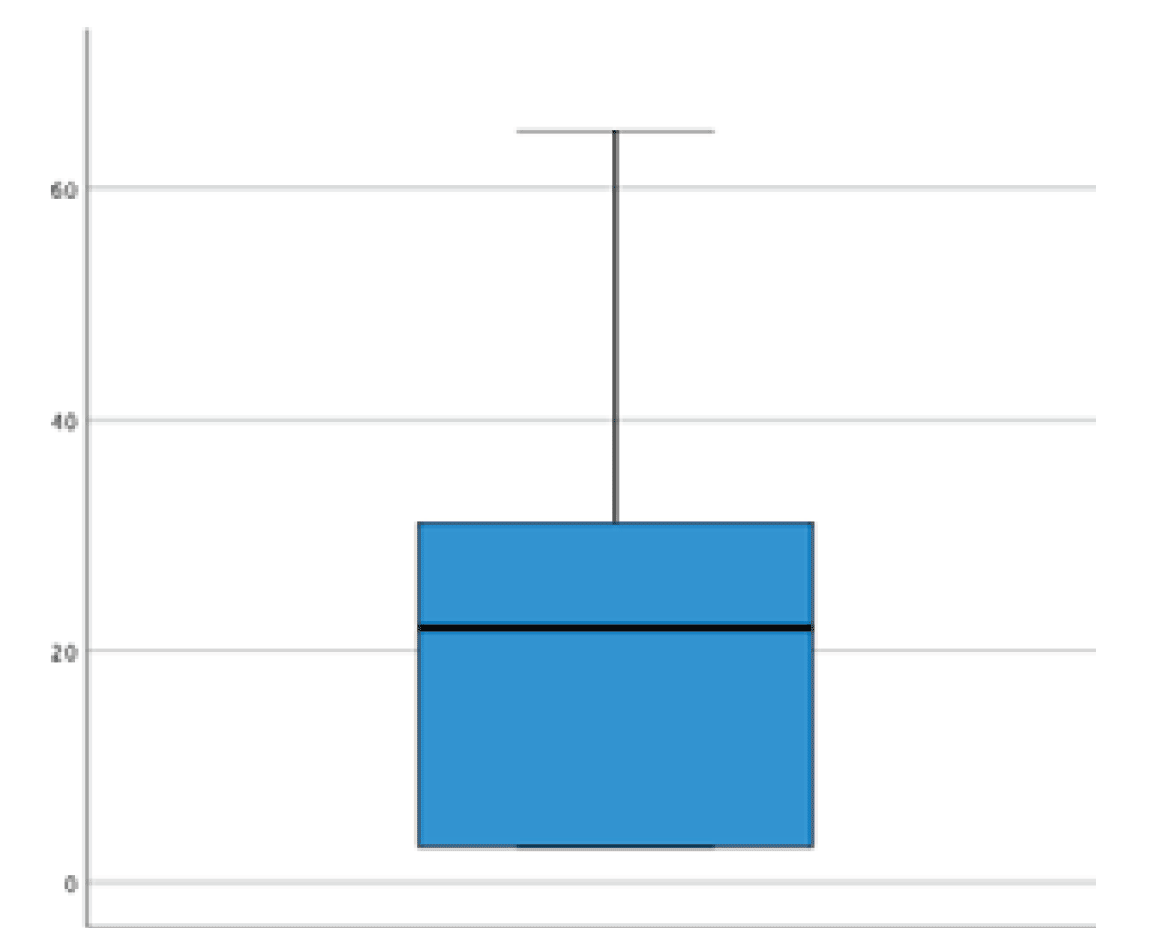
Concerning the travel time in minutes, the mean was 20.45 minutes (standard deviation of 15.168 minutes). The maximum travel time was 68 minutes (Fig. 2).
With regard to the dependent variable under study, it was found that 538 patients (19%) died during the first month after the emergency episode.
Analysis of binary logistic regressions
Global model
The first estimated model encompasses 2642 patients living in the direct reference area of Viseu PES and links mortality after 30 days with age, gender, the existence of a BES in the area of residence and the estimated travel time from the center of the municipality to the PES (Table 2, p-value for Hosmer-Lameshow test = 0.260).
As expected, age is statistically significant (p = 0.000), demonstrating an increase in the probability of dying by 0.049 percentage points for each year of life. There was a statistically significant impact of BES on mortality, with an odds ratio (OR) of 0.775 (95% IC = 0.584-0.975, p = 0.031), and it is verified that users covered by this service have a lower probability of dying during the first month after the episode, corresponding to 0.281% (a decrease of 1.47% to the average mortality rate).
Regarding the estimated travel time, there is a positive trend, but not statistically significant for the defined level (OR = 1.007, 95% IC = 0.999-1.015, p = 0.095).
Table 2: General binary logistic regression.
| B | p-value | Odds Ratio | Odds Ratio (95% CI) | ||
|---|---|---|---|---|---|
| Bottom | Higher | ||||
| Age | 0.049 | 0.000*** | 1.050 | 1.041 | 1.059 |
| Sex | 0.100 | 0.334 | 1.105 | 0.902 | 1.354 |
| Basic Emergency Service | -0.281 | 0.031** | 0.755 | 0.584 | 0.975 |
| Travel time in minutes | 0.007 | 0.095* | 1.007 | 0.999 | 1.015 |
| Constant | -5.232 | 0.000 | 0.005 | ||
The stars show the significant p-values (* for p<0.1, ** for p<0.05 and *** for p<0.01)
Comparative model of mortality MSES versus PES
In cases of gastrointestinal bleeding and myocardial infarction with Supra-ST, the most differentiated treatment is only available at the SUP in Viseu. In these situations, patients are transferred from MSES of Covilhã and Guarda. In fact, only in Viseu there is access to hemodynamic room and the technical capacity to perform gastrointestinal endoscopic treatments.
The comparative model between the two levels of responsibility was then constructed.
In this, mortality of patients from MSES, with myocardial infarction with Supra-ST or gastrointestinal bleeding, is not higher than patients from PES (OR = 0.749, 95% IC = 0.301-1.868, p-value = 0.536). Even so, we hypothesized that extra-hospital mortality was an important bias. In this sense, it was analyzed whether there were differences in the number of cases admitted with a diagnosis of acute myocardial infarction with supra-ST, since it unequivocally needs the approach in the PES by a hemodynamic team. Overall, 112 cases were registered, 50 from the MSES in Guarda and Covilhã (44.64%) and 62 from the PES area in Viseu (55.36%). The population of the MSES added corresponds to 237 140 inhabitants (46.32%) and that of the PES to 274 826 inhabitants (53.68%)23,26,27 According to the provisions, it appears that the number of cases adjusted to the population is very similar, corroborating the hypothesis that there are no differences in mortality between groups.
Comparative model of mortality by group of pathology
Following, the cases referring to each pathological group were aggregated and, for each of them, a model was estimated. It was compared 30-day-mortality with distance to PES and the existence of a BES in the area of residence. Adjustments were made for age and sex.
Therefore, it was started with stroke, a group with a relevant number of cases (588) and in which important results were obtained (Table 3). There is a statistically significant effect not only for the existence of BES (p = 0.042), but also in relation to the expected travel time (OR = 1.022, 95% IC = 1.002-1.042, p = 0.027).
Table 3: Stroke mortality model.
| B | p-value | Odds ratio | Odds ratio (95% CI) | ||
|---|---|---|---|---|---|
| Bottom | Higher | ||||
| Age | 0.025 | 0.024** | 1.026 | 1.003 | 1.048 |
| Sex | -0.391 | 0.137 | 0.676 | 0.404 | 1.132 |
| Basic Emergency Service | -0.643 | 0.042** | 0.526 | 0.283 | 0.976 |
| Travel time in minutes | 0.022 | 0.027** | 1.022 | 1.002 | 1.042 |
| Constant | -3.886 | 0.000 | 0.021 | ||
The stars show the significant p-values (* for p<0.1, ** for p<0.05 and *** for p<0.01)
In what concerns to ‘other major cardiovascular events’ it was found that BES do not confirm the protective effect seen previously. This group include acute pulmonary edema, myocardial infarction without ST elevation, dysrhythmias, high-risk pulmonary embolism, among others. On the other hand, travel time has an unfavorable trend, but not statistically significant for the defined level (p = 0.078).
Although it is not within the direct scope of this work, it is said that, in relation to respiratory problems, such as pneumonia, acute respiratory distress syndrome or chronic obstructive pulmonary disease with hypercapnic respiratory failure, mortality is higher in men, probably due to social (e.g. tobacco) and work (e.g. mining) habits that may be the target of public health intervention.
Regarding the cases of other groups of pathology there were no notable differences.
Comparative model of mortality by distance categorized
Finally, it was chosen to cluster patients into two groups: the first includes patients who were less than 34 minutes away (half the maximum time recorded) and the other group includes patients further than 34 minutes (Table 4). It was built another logistic model with mortality after 30 days, the existence of a BES and the estimated travel time from the center of the municipality to the PES.
In this case, it was found a significant impact related to the variable time travelled until the PES (OR = 1.551, 95% IC = 1.179-2.040). Specifically, there is an increase in mortality for the group of patients whose predicted time is equal to or greater than 34 minutes (p = 0.002).
Table 4: Comparative model of mortality by travel time group.
| B | p-value | Odds ratio | Odds Ratio (95% CI) | ||
|---|---|---|---|---|---|
| Bottom | Higher | ||||
| Age | 0.049 | 0.000*** | 1.050 | 1.042 | 1.059 |
| Sex | 0.103 | 0.319 | 1.109 | 0.905 | 1.359 |
| Basic Emergency Service | -0.232 | 0.038** | 0.793 | 0.637 | 0.987 |
| Travel time in minutes ≥ 34 | 0.439 | 0.002*** | 1.551 | 1.179 | 2.040 |
| Constant | -5.183 | 0.000 | 0.006 | ||
The stars show the significant p-values (* for p<0.1, ** for p<0.05 and *** for p<0.01)
Discussion
The main objectives of this study were to assess the impact of distance to the polyvalent emergency service and to evaluate the contribution of less differentiated services to the mortality of critically ill patients.
Regarding the first point, it was found that travel time contributes to increased mortality in critically ill patients. Even so, this effect is not as evident as is commonly believed. Our data are in agreement with the most recent literature that emphasizes that distance (or time) as a continuous variable and as estimates by simple linear regressions tends to underestimate the impact of this variable on the model.14,15,20 Relevantly, it was also shown that the impact of distance is particularly important in stroke patients.
Another question under analysis was to determine if users in the areas of Guarda and Covilhã would have a higher mortality due to diagnoses whose more differentiated treatment is only available in the PES of Viseu. In our analysis it was concluded that there is no evidence of a difference neither in mortality nor in the number of patients admitted for the most commonly referred diagnosis: acute myocardial infarction with ST elevation. It is also important to mention that the mortality rate after 30 days was 12.5%, and this value is within that registered in western countries.28) Our results dispel fears raised by an OECD report, which revealed regional disparities in Italy, a country where the performance of angioplasty in 48 hours varies between 5% and 60% and mortality between 5% and 18% depending on the municipality.29 There are studies that contribute to the framing of our results. Analyses carried out in Spain and Belgium have shown that the development of the referral network leads to a decrease in mortality, with no differences between hospitals with intervention cardiology and hospitals that refer their patients.30-32 Therefore, we can conclude that there is a good functioning of the MSES in Covilhã and Guarda with PES in Viseu.
An important contribution of our work is the evaluation of BES in reducing the mortality of urgent and critically ill patients. We are not aware of any work that addresses the effect of the existence of these services on the mortality of severe cases. This issue is indeed important, because it is obviously not feasible to build a differentiated emergency service in each location. Our results establish the pioneering idea that BES, which do not have the capacity to carry out treatments, contribute to reducing mortality. It was found that this effect is achieved mainly through stroke cases. In fact, our analysis shows that the protector effect of BES is largely accomplished by the gains in this pathology. In cases of stroke, it is established that time is crucial and there are delays in treatment motivated by the reluctance of users to resort to a medical service.33,34 In fact, there are several studies that show that elderly men who live in rural areas are the most resistant35-37) and it happens that this group has a high representativeness in our sample. In addition, it is also noted that SUB can be a good solution to avoid overcrowding of central emergency services, a well-identified problem that has been shown to lead to worse clinical results.38,39
Although we believe in the validity and relevance of results and the consequent conclusions drawn from it, it is necessary to recognize some main limitations of the work.
First, the center of the municipality of residence was considered as the starting point for each patient, which is an imperfect approximation of the place where they were located at the time of the onset of the acute illness episode.
Second, although most studies like ours analyze the mortality of cases admitted to the hospital, it is recognized that this method is imperfect because it does not account for extra-hospital mortality. The ideal model would require crossing hospital data with information from national records of causes of death by municipality.19 In our work, this analysis would be difficult to perform, since we did not evaluate a specific diagnosis.
Third, the different types of emergency services were evaluated based on the mortality of patients from their areas of influence, although we do not know whether they were actually treated in these services. Still, the demonstration of the absence of differences between populations with direct access to MSES or PES is relevant in itself. In addition, we have found no other explanation for the decrease in mortality of the population covered by BES. Furthermore, since by-pass is expected to occur in the network22, it would be impossible to avoid selection bias when comparing patients who were or were not initially treated in these services.
Conclusion
This study is pioneer in demonstrating that BES have a clear protective effect on critical ill patient mortality. In addition, it was found that travel time contributes to increased mortality. These variables are particularly relevant in cases of stroke.
In addition, it was concluded that there is no difference in the mortality depending on the level of differentiation of the central emergency service. A good interconnection between different levels of care allows for the creation of experienced referral centers and the provision of better-quality services to all patients.