Diaphragmatic eventration is the abnormal elevation of a hemidiaphragm due to lack of muscle/nerve function, maintaining its anatomical fixations.1 It is a very rare condition with an incidence of less than 0.05%, more commonly affecting the left hemidiaphragm.2 It may be congenital or acquired, thus presenting in both the pediatric and adult populations. Acquired cases are more common and are due to etiologies that result in phrenic nerve injury and muscle atrophy.1,2
A 64-year-old caucasian woman, victim of a left perforating cervical trauma that resulted in a phrenic nerve injury and left upper limb paralysis ten years ago, presented in our health unit with dyspnea, epigastralgia, anorexia and weight loss that has been worsening in the past year. Physical examination showed decreased breath sounds at the left lung base and discomfort on palpation of the epigastrium. A chest X-ray was requested, showing an elevation of the left diaphragmatic dome - possible diaphragmatic hernia/eventration (Fig. 1). Computed tomography (CT) was requested confirming the presence of a diaphragmatic eventration, as well as signs of gastric volvulus with mediastinal shift and partial atelectasis of the left lower lung lobe (Fig. 2). Spirometry showed a restrictive pattern. Radial diaphragmatic plication surgery with gastropexy was performed (Fig. 1). After treatment, the patient was asymptomatic, having fully recovered lung function.
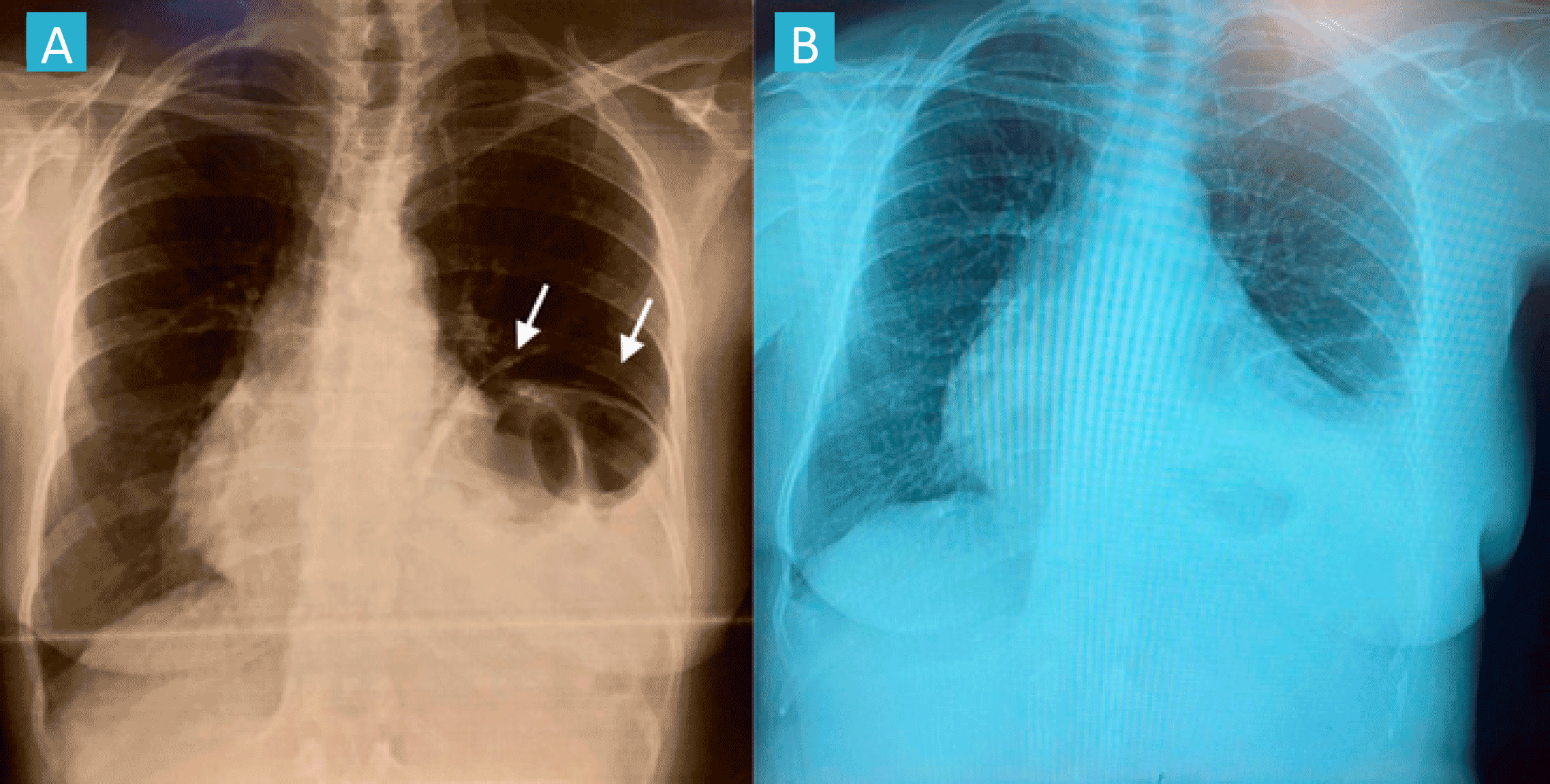
Figure 1: Comparison between preoperative X-ray and one month postoperative control X-ray. Preoperative X-ray shows marked elevation of left diaphragmatic dome (arrows), with elevation of the abdominal visceras (A). One month postoperative control X-ray shows partial atelectasis of the left lower lung lobe (smaller than previous exam) and occlusion of the left costophrenic recess (B).
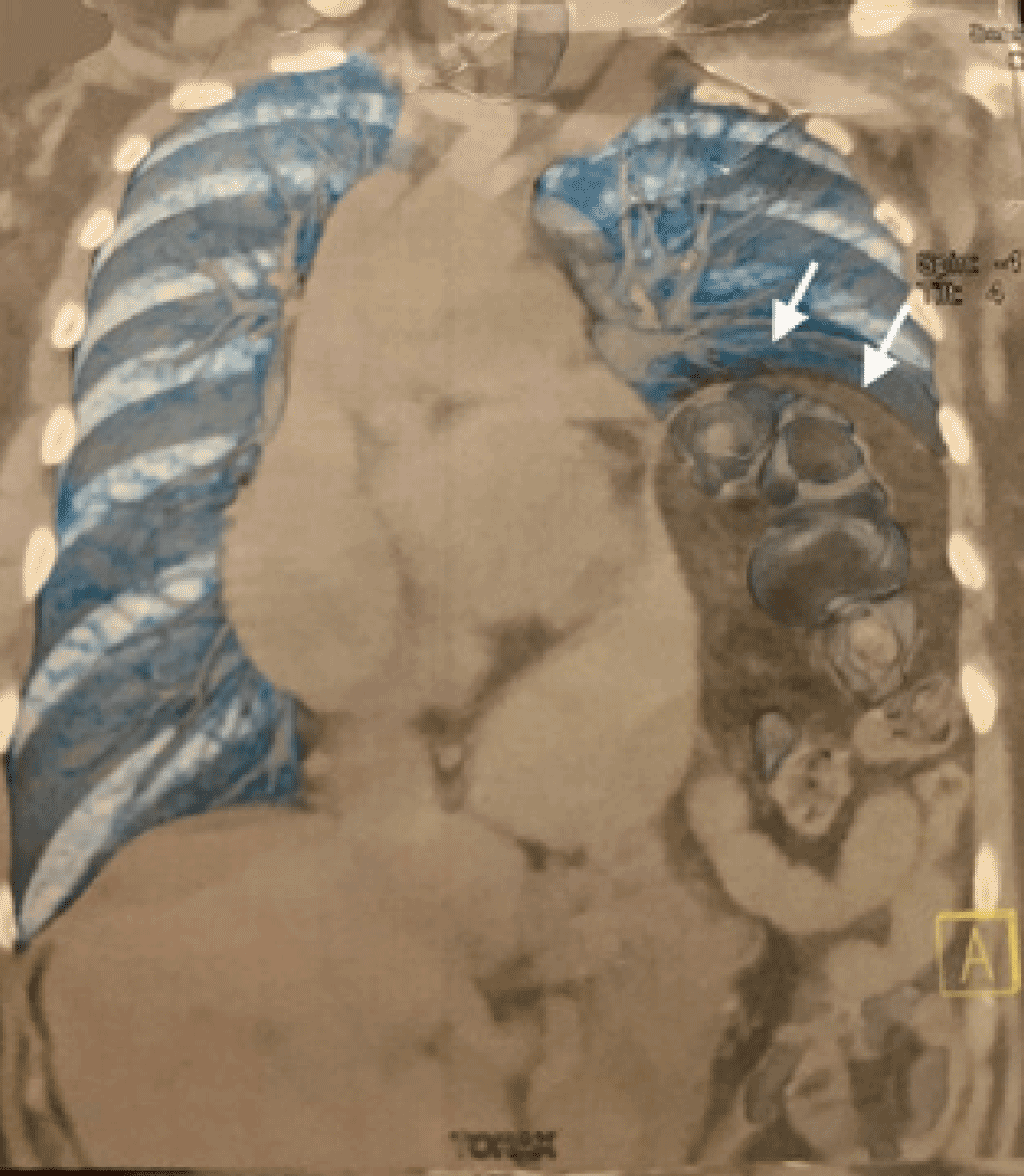
Figure 2: Computer tomography shows left diaphragmatic eventration (arrows) causing right mediastinal shift and left atelectasis of the lower lung lobe.
Diaphragmatic eventration patients have variable presentations. Most patients are asymptomatic; however, some may present important, but nonspecific, gastrointestinal and respiratory symptoms.1 X-ray and CT are used to confirm the diagnosis, and pulmonary function tests should be performed.2,3 Treatment is determined by etiology and clinical severity. In asymptomatic or mild cases, supportive care is recommended. In severe cases (respiratory distress, recurrent pneumonia, mediastinal shift, inability to be removed from mechanical ventilation), surgical plication may be indicated.1,4















