Introduction
Landau-Kleffner syndrome (LKS) is a rare epileptic syndrome of childhood characterized by loss of acquired language ability and continuous spike and wave during slow sleep on electroencephalogram (EEG) and clinical seizures, described first in 1957 by Landau and Kleffner. It occurs in previously healthy children with normal language skills and development. It is characterized by epileptic seizures, aphasia and characteristic EEG abnormalities.1,2 However, epileptic seizures are infrequent and not a prerequisite for LKS. Despite the severe electroencephalographic abnormalities, seizures never occur in 20%-30% of patients.3
The exact etiology is not known, though a genetic predisposition has been postulated.4
Boys are affected twice as frequently as girls, and a little over 200 cases have been reported so far.
Aphasia starts commonly among children of 3 to 8 years old, with a peak between 5 and 7 years. Verbal auditory agnosia is the typical language dysfunction. Patients have difficulty understanding what they are being told and respond to visual as well as auditory stimuli. (2-4 The aphasia has a subacute onset and a progressive course, with a fluctuating pattern of spontaneous improvements and exacerbations.3
Electroencephalographic findings during sleep are continuous slow spike and waves, mainly at 1.5-2.5 Hz, persisting through all the slow-sleep stages. This pattern of continuous spikes and waves during slow sleep or electrical status epilepticus in sleep in patients with LKS may be unilateral or clearly lateralized, over the temporal or parieto-occipital regions.3
The language disorder of LKS has similarities with autism spectrum disorder. Communication deficits in autism include abnormal development of spoken language and impaired ability to initiate or sustain conversation. Additionally, seizures may occur in autism, and EEG abnormalities are also common. Furthermore, at least a third of autistic toddlers demonstrate neurodevelopmental regression, involving language, social skills, play, and cognition. LKS represents selective loss of language in association with an abnormally paroxysmal EEG, characterized by electrographic status epilepticus of slow-wave sleep. That is why the differential diagnosis can be challenging, and it is important to increase awareness about this entity. The differential diagnosis also includes attention deficit hyperactivity disorder, deafness, elective mutism and acute psychiatric disorders.5
The benign course of the epilepsy versus devastating language impairment, fluctuating course of aphasia, lag of improvement in relation to the EEG, possibility of spontaneous remission, and rarity of the disorder render multiple barriers to controlled clinical trials. The determination of treatment efficacy is difficult. There is relatively scarce mention in the literature regarding antiepileptics of choice.5
Case Report
A 6-years-old male child, with normal psychomotor development, who begins to experience difficulties in understanding the meaning of some words, sometimes with incoherent speech, writing difficulties, with irregular handwriting and spelling errors, which according to the mother were new.
In the neurological evaluation, he presented a loss of comprehensive language with auditory verbal agnosia, as well as difficulties in fine motor skills and in graphomotor coordination (Fig. 1).
After clinical suspicion, because of the auditory verbal agnosia and watching his notebook (Fig. 1), the diagnosis of LKS was confirmed by night video-EEG, with abundant paroxysmal activity of bilateral and independent fronto-center-temporal spikes and spike-wave activity, with an almost continuous exacerbation during sleep (Fig. 2).
Initially treated with the association of valproate and clobazam, without improvement, he started prednisolone, with improvement in language, writing and normalization of the EEG (Figs. 1 and 2).
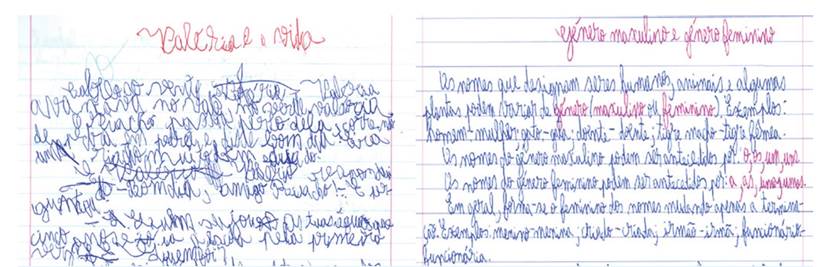
Figure 1 On the left, handwriting at the time of diagnosis. On the right, handwriting under therapy with valproate, clobazam and steroid.
Discussion
The diagnosis of LKS, in this case, was made on the basis of rapid loss of comprehensive language with auditory verbal agnosia, as well as difficulties in graphomotor coordination, in a previously normal child, associated with abnormal EEG compatible with the diagnosis of epilepsy.
Among 50% of the cases, language problems are the first symptoms, like in the present case. Impairment in language and speech may show wavy changes and recurrences in follow-up.2
This disorder appears to be relatively uncommon, and its precise frequency is unknown. The likelihood of misdiagnosing is high due to lack of knowledge of the disease by health care professionals. It is imperative that those leading with neurodevelopmental problems (like neurodevelopmental pediatricians, neuropsychologists and speech therapists) become alert to the characteristic symptoms of LKS.6
Further cases could be misdiagnosed as deafness during this period. Therefore, otorhinolaryngology polyclinics may be the first admission point. Cases cannot respond to loud-voice stimuli and may be misdiagnosed as loss of audition. The diagnosis of LKS is often delayed for many reasons. The clinical features of auditory agnosia may be subtle at the beginning, or the cases may be misdiagnosed with psychiatric disorder.2
While there is considerable overlap in the semiology of LKS and autism, some differences emerge. The great majority of children with autism who undergo language regression do so before 3 years of age, versus a mean age of language regression in LKS of 5-7 years. LKS does not feature the behavioral profile that encompasses the core deficits of autism, i.e., abnormalities of reciprocal social relatedness and restricted stereotypical patterns of interests and behaviors.5
Almost all cases have abnormal EEG predominantly involving the temporoparietal regions, but 30% may not have associated clinical seizures, like our patient.3 EEG of our patient showed abundant paroxysmal activity of bilateral and independent frontal-center temporal spikes and spikes, with sleep exacerbation (Fig. 2).
Diagnosis of LKS is based on characteristic EEG abnormalities and acquired aphasia in children with previously normal language and developmental milestones. EEG may be accepted as most objective diagnostic test in LKS.2-4
Early and aggressive therapy is mandatory. The seizures may respond to a combination of anticonvulsants including valproic acid, clobazam, clonazepam, levetiracetam, ethosuximide and sulthiame. Others, such phenytoin, phenobarbital, and especially carbamazepine and oxcarbazepine as well as new antiepileptic drugs, such as lamotrigine and topiramate are generally to be avoided because they have been associated with exacerbations of the epileptiform discharges. Corticosteroids have been reported to markedly improve the evolution of the disease, especially when started early in the course, but seizure and aphasia may relapse when these are tapered. Prolonged, chronic, or intermittent therapy may be warranted if significant improvement of neuropsychological function is attained. Intravenous immune globulin demonstrated promising results in some cases of LKS. The ketogenic diet and vagus nerve stimulation, as well as subpial transection, has led to some clinical improvement in selected patients.3-5
Our patient was treated with valproic acid, clobazam and oral steroids, after which he showed improvement. His language function, graphomotor coordination and EEG abnormalities had improved significantly (Figs. 1 and 2).
The prognosis of these patients in terms of seizure (when present) outcome was good, but outcome of language and cognitive functions was variable. Adequate and early treatment management may avoid language and cognitive deterioration. There are few long-term follow-up studies and no firm conclusions regarding potential for recovery. Outcomes range from complete recovery to permanent severe aphasia, with most experiencing improvement and residual moderate language deficits.3-5
In conclusion, LKS is a condition of unpredictable outcome and varying severity with a potentially relapsing remitting course, requiring constant adaptation and resourcefulness from parents, speech/language therapists, neuropsychologists, and neurologists. In the presented case, high index of suspicion after clinical evaluation and the awareness of the pediatric neurologist was crucial for the adequate diagnosis and early treatment.
















