A 69-year-old man with sleep apnea, high blood pressure, dyslipidemia, and personal history of aortic valve replacement with a mechanical valve 12 years prior, presented with dyspepsia, nocturnal epigastric pain, and perceived abdominal “fullness”. He described ongoing symptoms for about 2 years, with an abrupt onset after a single episode of self-limited, severe epigastric pain, that appeared during anterior flexion of the trunk, while lifting a weight from the floor.
After showing no symptomatic improvement with protein pump inhibitors, an upper gastrointestinal endoscopy showed a foreign body (apparent metal wire), with one extremity adherent to the gastric body wall (Fig. 1). Endoscopic removal was unsuccessful.
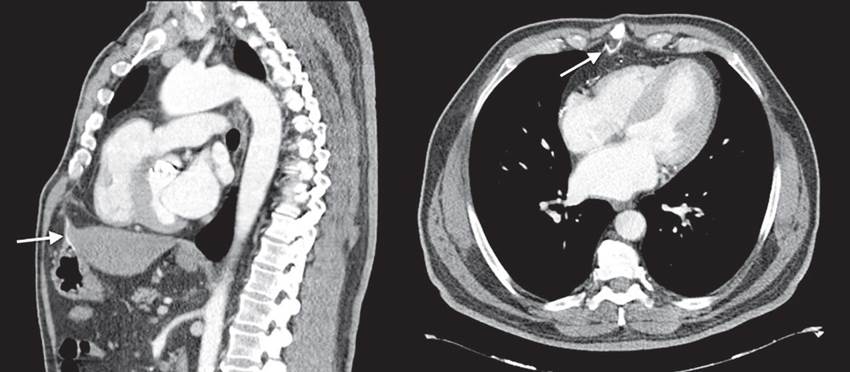
Thoracic-abdominal computed tomography shows sternotomy wires from previous surgery, along with a metallic wire that extends from a subxiphoid location to a perigastric position, and perforates the anterior wall of the gastric body, with no signs of pneumoperitoneum or fluid collection (Fig. 2).
Migration of thoracic wires is a known, albeit rare complication of cardiac surgery. 1,2 Although, frequently, this complication presents on a post-operatory setting, cases of migrating temporary epicardial pacemaker wires, as well as migrating sternal fixation wires, have been previously reported, years after stability in the precordium. (1-3
After multidisciplinary evaluation, due to clinical and imagiologic stability, the patient’s comorbidities, and no signs of local complication, a decision against an invasive and potential high-risk procedure to remove the wire was made, and an active surveillance approach has been adopted.

Figure 1 Upper gastrointestinal endoscopy shows a 50 mm metal wire, with millimetric thickness, perforating the anterior wall of the gastric body.