Introduction
The aging of the population and the rise in life expectancy, coupled with the high prevalence of chronic-degenerative diseases and their complications, call for changes in higher education regarding the care of vulnerable populations, including older adults and end-of-life care (Ministério da Educação e Cultura - MEC, 2014; WHO, 2020). Terminal illness is a significant challenge that requires reflection on the training of health professionals, especially doctors who care for older adults (Gryscheck et al.,2012; Caldas et al., 2012), as well as the sick and family members/caregivers (Jorge et al., 2018). The particularities of teaching care for older adults (Jorge et al., 2018) and knowledge of palliative care and end-of-life among teachers (Albuquerque et al., 2020; Brito et al., 2020; Correia et al., 2018; Correia et al., 2020; Freitas, 2017; Lemos et al., 2017; Marques et al., 2019; Malta et al., 2018; Mateus et al., 2019; Orth et al., 2019; Pereira et al., 2019; Sousa et al., 2020) can facilitate essential and thought-provoking discussions in higher education and provide practical strategies to expand educational programs, articulating health benefits, end-of-life care, and quality of life for patients and family members/caregivers.
This study emphasizes the importance of improving higher education programs, particularly regarding care for vulnerable populations and end-of-life care. Medical professionals must be adequately equipped to handle the challenges of the aging population and chronic-degenerative diseases. Developing effective educational strategies could lead to better health outcomes for patients and caregivers. The study also highlights the need for ongoing research and development to ensure that healthcare professionals have the knowledge and skills needed to address the unique challenges of caring for older adults and those at the end of life. It is noteworthy that the literature also pointed out physiological changes inert to longevity, bringing with them diversity in health conditions for the geriatric patient, in addition to the strong relationship with the path to the end of life of the older persons, which deserves broader attention from health professionals on tactics and techniques that promote quality and acceptability at the end of life (Brito et al., 2020; Malta et al., 2018; Marques et al., 2019; Melo et al., 2019; Pineli et al., 2016). Palliative Care provides care professionals in a multidisciplinary team that services patients with incurable chronic diseases and/or terminally ill (WHO, 2020). PC must be fully offered to patients, as they attribute to the prevention and treatment of pain, in addition to minimizing client/family suffering (Caldas et al., 2018; Marques et al., 2019; Malta et al., 2018; Freitas, 2017; Pereira et al., 2019; Dalpai et al., 2017; Caldas et al., 2016; Castro et al., 2021). The changes brought about by the evolving epidemiological landscape have led to educational innovation in medical training. The Ministry of Education has institutionalized new national curriculum guidelines to address these changes. Moreover, the changes in the epidemiological landscape have necessitated adjustments to the organization, development, and assessment of medical degrees in Brazil (Albuquerque et al., 2020; Pereira et al., 2019; Melo et al., 2019; Pineli et al., 2016).
Integrating pedagogical care activities into Palliative Care offers valuable opportunities to train healthcare professionals capable of approaching diverse situations related to life-threatening illnesses with a holistic, individualized, and compassionate approach. Furthermore, this care model offers a superior alternative across all levels of healthcare, minimizing unnecessary costs while prioritizing patient care, as well as the needs of their families and caregivers, in diverse physical, social, cultural, and spiritual contexts. Nonetheless, providing palliative care demands a true calling to attend to individuals with incurable chronic diseases. It involves cultivating essential skills and competencies such as empathy, effective communication, personal maturity, sincerity, and scientific knowledge (Freitas et al., 2017; Pereira et al., 2019; Melo et al., 2019; Pineli et al., 2016; Dalpai et al., 2017; Caldas et al., 2016; Castro et al., 2021). Despite its importance, however, gaps remain in the approach to this topic, particularly regarding communicating complex news, managing challenging signs and symptoms, and preparing for the inevitability of death and the ethical dilemmas stemming from religious beliefs (Pereira et al., 2019; Melo et al., 2019; Pineli et al., 2016). Therefore, this research aims to integratively review how Brazilian medical schools incorporate palliative care into their curricula.
Methods
This study is an integrative literature review that aims to provide a descriptive analysis. The methodological approach involves six steps: (1) defining the research question, (2) setting eligibility criteria and selecting articles, (3) choosing a sample, (4) presenting the chosen studies in a table format, (5) conducting a critical analysis of the findings, and (6) interpreting and synthesizing the results.
The PICO strategy was used to construct the research question, representing an acronym for “Patient, Intervention, Control, and “Outcomes.” These four components are fundamental for defining the research question and searching for scientific evidence. The study aimed to investigate palliative care teaching in Brazilian medical schools. It was guided by the research question: What is the current status of palliative care education in medical schools across Brazil?
The study’s literature search was conducted using the Virtual Health Library (VHL), which includes LILACS (Latin American and Caribbean Literature on Health Sciences Information), SciELO (Scientific Electronic Library Online), and Medline (PubMed) databases. The search strategy utilized DeCS (Descriptors in Health Sciences) and MeSH (Medical Subject Headings) terms, including Palliative Care, Medical Education, and Diseases, all registered in DeCS.
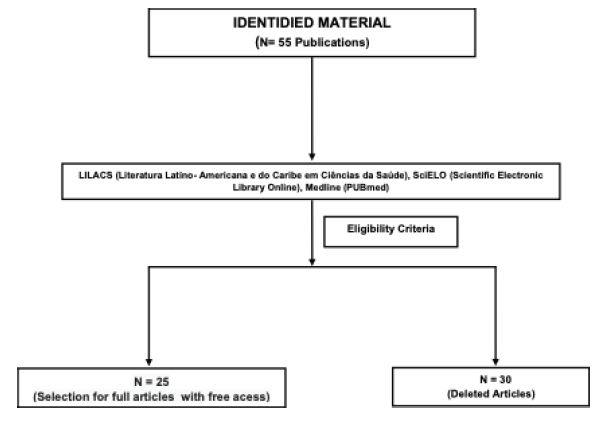
The study used inclusion criteria that required publications in English, Portuguese, and Spanish, in the form of full-text articles that were freely accessible through the Virtual Health Library (VHL) databases LILACS, SciELO, and Medline (PubMed). Dissertations, theses, and book chapters were excluded. The initial screening of the bibliographic material involved reading the abstracts to identify articles that met the study’s objectives. Of the 55 publications identified from 2016 to 2021, only 25 met the inclusion criteria (Figure 1). After the initial screening, each article was thoroughly read to extract and systematize the relevant information according to Table 1.
Results
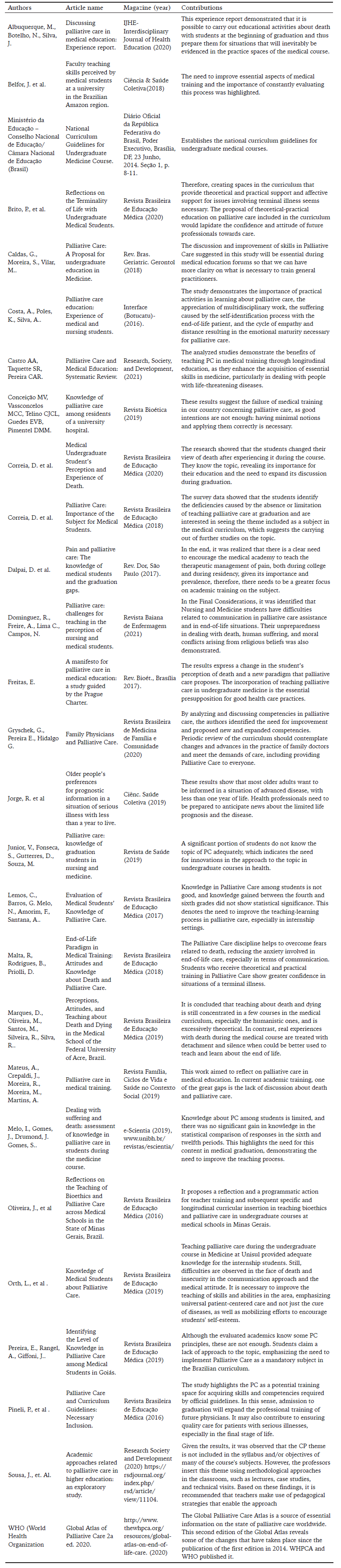
After identifying and evaluating 55 publications from 2016 to 2021, 25 articles were found to meet the inclusion criteria. The final sample includes publications that were published between 2016 and 2021, which is a period that coincides with the Ministry of Education’s publication of the National Curriculum Guidelines for undergraduate courses in Medicine in Brazil (2014) and the 2nd edition of the Global Atlas of Palliative Care. These publications highlighted the importance of Palliative Care in medical education, emphasizing the positive impact of such education in improving professionals’ decision-making when caring for patients in advanced stages of life with an imminent risk of death (Table 1).
Palliative Care is a broad and significant topic in medical sciences. The literature search for scientific-based studies provided insights into the following main results: 1- The complexity of care for patients with incurable chronic diseases and their families demands a humanized approach and raises reflections and questions about life and death. Palliative Care can help alleviate patients’ physical and emotional suffering, improve their quality of life, and support family members/caregivers; 2- The training of future healthcare professionals in Palliative Care during their undergraduate education has limitations, and curriculum innovations are necessary. The proposals of new curriculum guidelines, established by the Ministry of Education in 2014, can provide opportunities to improve skills and competencies for learning the solid principles of care based on comprehensive, person-centered models. This can contribute to tackling the challenges of dealing with people with incurable chronic diseases, frail and dependent older adults, and their families. A humanized approach from the interdisciplinary team is required, bringing reflections and questions about life and, consequently, finitude.
Discussion
The National Curriculum Guidelines (DCN) regulate the training of medical professionals to recognize and solve real problems of individual and collective health at different levels of health care while emphasizing social responsibility and the commitment to defending citizenship and human dignity. Therefore, academic training should focus on the integral health of the human being and gradually increase the inclusion of palliative care in the curriculum. Several studies support this notion (Brasil, 2014; Correira et al., 2018; Freitas, 2017; Gryscheck et al., 2012; Malta et al., 2018; Pereira et al., 2019; Pineli et al., 2016). It is important to include palliative care in the curriculum is necessary to prepare future physicians to deal with the complexity of caring for patients with incurable chronic diseases, frail and dependent older adults, and family members/caregivers. This requires a humanized approach from the interdisciplinary team and brings reflections and questions about life and finitude.
However, despite the recognized importance of PC in medical education, several studies have indicated a lack of content and inadequate teaching methods in the area, highlighting the need for curriculum reform and innovation (Belfor et al., 2018; Caldas et al., 2018; Conceição et al., 2019; Pineli et al., 2016). It is also crucial to provide theoretical and practical training in managing pain and other symptoms in terminally ill patients, as well as improving the communication skills of medical students to address the emotional and psychological needs of patients and their families (Conceição et al., 2019; Correia et al., 2020; Dalpai et al., 2017). In this context, better preparation and training of healthcare teams involved in caring for terminally ill patients are necessary to overcome existing gaps in medical education. Furthermore, maintaining the bond between the patient, family, and caregivers during this process remains challenging, affecting the ability to provide optimal care and make informed decisions (Caldas et al., 2018; Freitas, 2017; Malta et al., 2018; Mateus et al., 2019).
The literature highlights the need for educational incentives to promote adequate PC practice to meet the needs of eligible patients by health professionals in Brazil (Belfor et al., 2018; Brito et al., 2020; Caldas et al., 2018; Correia et al., 2018). However, health professionals tend to have a curative perception of illnesses, and a multidisciplinary approach prioritizing training in this area is required to handle patients with life-threatening and incurable chronic diseases effectively (WHO, 2020; Albuquerque et al., 2020; Brito et al., 2020; Caldas et al., 2016; Conceição et al., 2019; Correia et al., 2020; Junior et al., 2019).
Therefore, it is crucial to implement joint pedagogical and therapeutic actions in PC during health professional training (Castro et al., 2021; Conceição et al., 2019; Oliveira et al., 2018; Sousa et al., 2020; WHO, 2020). The team must experience different patient care situations to provide humanized and individualized care, thereby maintaining the quality of life for all those involved in the evolution of incurable and life-threatening diseases (Conceição et al., 2019; Dominguez et al., 2021; Junior et al., 2019; Oliveira et al., 2018). Thus, the PC theme must be gradually increased in different educational scenarios to favor the improvement of health professionals (Jorge et al., 2018; Junior et al., 2019; Lemos et al., 2017; Mateus et al., 2019; Melo et al., 2019; Oliveira et al., 2019). This will lead to better care for patients, families, and caregivers in various physical, social, cultural, spiritual, and economic contexts (Dominguez et al., 2021; Pineli et al., 2016; WHO, 2020).
Based on the findings of the integrative review, it is recommended that medical schools in Brazil increase the content on PC in their curriculum and provide better training to health professionals in this area. The training should include theoretical and practical approaches to managing pain and other symptoms in terminally ill patients and maintaining the bond between the patient, family, and caregiver.
To achieve this, joint pedagogical and therapeutic actions in PC should be implemented during the training of health professionals. These actions can be achieved through multidisciplinary approaches that prioritize training in PC. Additionally, medical students should be exposed to different patient care situations to provide humanized and individualized care and maintain the quality of life for all involved in the evolution of incurable and life-threatening diseases.
It is also important to note that the current literature on PC teaching in higher education institutions in Brazil is limited. Further research is needed to encourage multi-disciplinarity in PC and enhance potential research to favor the immersion of this subject in the undergraduate environment. Improving PC education in medical schools can lead to better care for patients/family/caregivers assisted in multiple physical, social, cultural, spiritual, and economic contexts.
Conclusion
The importance of teaching palliative care in medical education cannot be overstated. Preparing future healthcare professionals to provide comprehensive care that focuses on the person, not just the cure of diseases, is crucial. Palliative care provides an approach that emphasizes quality of life and comfort for patients, as well as support for their families and caregivers.
In addition, the complexity of dealing with patients with threatening incurable chronic diseases requires a humanized approach and raises questions about life and death. Healthcare professionals must be adequately prepared to handle such situations, providing the necessary support, comfort, and guidance to patients and their loved ones.
Therefore, it is essential to include palliative care in medical curricula to equip future professionals with the skills and knowledge needed to provide high-quality care to patients and their families. It is a crucial step towards ensuring that vulnerable patients receive the best care possible and that healthcare professionals are prepared to handle the difficult and complex situations that may arise during palliative care.