INTRODUCTION
Surgery is an activity that seeks diagnosis and medical treatment of trauma, deformities and diseases using manual and instrumental actions1. Laparotomy is a surgery involving an incision in the abdominal wall to access the abdominal cavity. It can be diagnostic, in which case the nature of the disease unknown, being necessary to identify the cause or therapeutic when the cause was identified, and the procedure is required to treat it.2Postoperative complications are defined as all dysfunctions that occur in this period and have a disease or anomaly associated clinically relevant that affects recuperation's progression negatively. Frequently considered the major cause of morbidity, mortality and prolonged institutionalization, being related with an increase of healthcare costs.3According to Fonseca4postoperative complications factors can be subdivided into two major categories. The first one is intrinsic to the patient like being older than 60 years, having a background of respiratory pathology (chronic bronchitis, emphysema, asthma, obstructive sleep apnea,(among others), heart congestive disease, anesthetic risk classification by the American Society of Anesthesiology (ASA) ≥ II, smoking and alcoholic habits, obesity, poor general condition, malnutrition and metabolic changes with special focus on diabetes. The second one is related with the surgery procedure itself. Surgeries up to 3 hours have increased risks due to mechanical ventilation, the amount of anesthetic drugs and analgesics and accumulation of bronchial secretions during the procedure. On the other hand, the type of surgery, incision, anesthesia and analgesia also play an important role, being that the last one is related with the effect on muscular function, indirectly through the blockage of the neuroaxis, central or the motor plate. Both, upper abdominal e thoracic, are the ones with the highest risk.5The main pulmonary postoperative complications (PPC) are pneumonia, bronchospasm, respiratory failure, atelectasis, hypoventilation, hypoxia, and infections.3The prevalence of PPCs in upper abdominal surgery range from 17% to 88%.6However, a more recent study found a decrease of PPC prevalence in laparotomy to only 7%.5Incentive spirometers are mechanical devices developed to allow high pulmonary volumes by sustaining maximum inspirations leading to an increase of current volume, inspiration time and inspiratory flux that assures alveolar stability.7 It was introduced by Bartlett and his coworkers to encourage postoperative patients to take long, deep, slow breaths to increase lung inflation.8 The efficacy of postoperative respiratory exercises in abdominal surgery is still debatable. Pasquina et al.9 suggest that the regular use of postoperative respiratory exercises for abdominal surgeries is not justified, arguing that few clinical trials demonstrate their efficacy as prophylaxis. Lawrence, Cornell and Smetana10 report that any pulmonary expansion intervention in the postoperative period of abdominal surgeries reduces the risk of pulmonary complications. An initial search of the Joanna Briggs Institute Database of Systematic Reviews and Implementation Reports, the Cochrane Library, PROSPERO, PubMed and CINAHL found no existing systematic review that examine the effects of respiratory exercises in patients undergoing laparotomy surgery. Therefore, it is necessary to examine the decision to use incentive spirometry in the patient undergoing laparotomy surgery, which involves an intense critical analysis based on scientific evidence.
Deepening, the review focuses on the following questions:
Is incentive spirometry in the patient submitted to laparotomy, effective in reducing PPC?
Is incentive spirometry in the patient submitted to laparotomy, effective in reducing hospital length-of-stay and readmissions?
What are the characteristics of incentive spirometry exercises (frequency, time, repetitions and skilled professional involved)?
METHODS
This review follows the methodology proposed by the Joanna Briggs Institute (JBI) for the conduct of systematic reviews11 and complies with the Preferred ReportingItems for SystematicReviews and Meta-Analyses.12
Search strategy
| PubMed - searched in May 17th, 2019: 48 results ((("incentive spirometry"[Title/Abstract] ) OR spirometry[MeSH Terms])) AND ((((ICU[Title/Abstract]) OR "post-anesthesia care unit"[Title/Abstract]) OR "intensive care unit"[Title/Abstract]) OR "surgery ward"[Title/Abstract]) Filters: English; Portuguese; Spanish; Publication date from 2008/01/01 to 2020/12/31 | |
| CINAHL - searched in May 17th, 2019: 6 results S14 S12 AND S13 Limiters - Published Date: 20080101-20201231; Exclude MEDLINE records; Language: English, Portuguese, Spanish S13 S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 S12 S1 OR S2 OR S3 S11 TI "surgery ward" S10 AB "surgery ward" S9 AB "intensive care unit" S8 TI "intensive care unit" S7 TI "post-anesthesia care unit" S6 AB "post-anesthesia care unit" S5 AB ICU S4 TI ICU S3 MH spirometry S2 AB "incentive spirometry" S1 TI "incentive spirometry" |
6 48758 5528 15 95 28392 11744 92 171 19363 7031 5473 125 109 |
| Scopus- searched in May 17th, 2019: 59 results ( ( TITLE-ABS-KEY ( "incentive spirometry" ) OR TITLE-ABS-KEY ( spirometry ) ) ) AND ( ( TITLE- ABS-KEY ( icu ) OR TITLE-ABS-KEY ( "post-anesthesia care unit" ) OR TITLE-ABS-KEY ( "intensive care unit" ) OR TITLE-ABS-KEY ( "surgery ward" ) ) ) AND ( LIMIT- TO ( PUBYEAR , 2019 ) OR LIMIT-TO ( PUBYEAR , 2018 ) OR LIMIT- TO ( PUBYEAR , 2017 ) OR LIMIT-TO ( PUBYEAR , 2016 ) OR LIMIT- TO ( PUBYEAR , 2015 ) OR LIMIT-TO ( PUBYEAR , 2014 ) OR LIMIT- TO ( PUBYEAR , 2013 ) OR LIMIT-TO ( PUBYEAR , 2012 ) OR LIMIT- TO ( PUBYEAR , 2011 ) OR LIMIT-TO ( PUBYEAR , 2010 ) OR LIMIT- TO ( PUBYEAR , 2009 ) OR LIMIT-TO ( PUBYEAR , 2008 ) ) AND ( LIMIT- TO ( LANGUAGE , "English" ) OR LIMIT-TO ( LANGUAGE , "Spanish" ) OR LIMIT- TO ( LANGUAGE , "Portuguese" ) ) AND NOT ((((PMID (1*)) OR (PMID (2*)) OR (PMID (3*)) OR (PMID (4*)) OR (PMID (5*)) OR (PMID (6*)) OR (PMID (7*))) OR (PMID (8*)) OR (PMID (9*)))) | |
| DART-Europe - searched in May 17th, 2019: 32 results spirometry AND (ICU OR post-anesthesia care unit OR intensive care unit OR surgery ward) Filters: English; Portuguese; Spanish; Publication date from 2008/01/01 to 2020/12/31 | |
| Open Grey - searched in May 17th, 2019: 18 Results spirometry Filters: English; Portuguese; Spanish; Publication date from 2008/01/01 to 2020/12/31 | |
| RCAAP - Repositório Científico de Acesso Aberto de Portugal - searched in May 17th, 2019: 1 result |
spirometry (Abstract) AND ICU OR post-anesthesia care unit OR intensive care unit OR surgery ward (Abstract) Filters: English; Portuguese; Spanish; Publication date from 2008/01/01 to2020/12/31 |
The search strategy aimed to find both, published and unpublished studies. At first, an initial limited search was done in MEDLINE and CINAHL, followed by the analysis of text words in the titles, abstracts and index terms used to describe the article. In the final step, the reference list of all identified reports and articles were searched for additional studies. English, Spanish and Portuguese studies have been considered for inclusion in this review.
This review considered studies after 2008, that evaluate the effectiveness of incentive spirometry prophylaxis in adult patients in preventing postoperative respiratory complications. This choice is supported, by the fact that it is reasonable to base our review on recent research activity. The databases searched included: CINAHL Plus with Full Text, PubMed and Scopus. The search for unpublished studies included: DART-Europe, OpenGrey and RCAAP.
Quality Assessment and Data Analysis
Mendeley version 1.17.6 was used to manage the list of articles retrieved; any duplications were removed. All identified articles were assessed for relevance according to the title and abstract. Whenever the title and abstract lacked data to make a decision, we verified the inclusion criteria described previously by reading the full-text articles. Articles selected for retrieval were assessed by 2 independent reviewers for methodological validity before their inclusion in the review using standardized critical appraisal instruments from the JBI Critical Appraisal Checklist for Randomized Controlled Trials.13 The cutoff point for inclusion of a study in the review was receiving a ‘‘yes’’ answer to at least 10 questions (80%) on the standardized critical appraisal instrument. Two independent reviewers assessed all studies. Any disagreements that arose between the reviewers were resolved through consultation with a third reviewer. The data was extracted from the article included in the review independently by 2 reviewers, using a data extraction table, by taking into account the review questions. The data extracted included specific details about the study aims, design, measurement instrument, and setting; the sample characteristic; and the main results of significance to the aims of this review (Table 1). Any disagreements arising between the reviewers regarding what data was relevant for extraction were resolved through discussion or consultation with a third reviewer. A narrative synthesis was used for the data analysis of the included study. Therefore, the findings are presented in narrative form.
Table 1 Data Presentation Over the Included Studies in the Systematic Review
| Author(s) Year Country | Aims | Study Design: Measurement Instrument | Setting | Sample Characteristic | Main Results |
|---|---|---|---|---|---|
| Fernandes, S, et. Al Brazil (2016)(14) |
Evaluate vital capacity after 2 respiratory techniques in patients undergoing abdominal surgery | Randomized prospective study: - Medical Research Council - Functional Independence - Measurement Vital Capacity |
Intensive Care Unit (ICU) | TOTAL: 38 Positive Intermittent Pressure Group: 20 Volumetric Incentive Spirometer Group: 18 |
- There was no significant difference between the 2 groups. - Both groups showed significant difference in VC measurements when comparing the 1st measurement before respiratory therapy and the last measurement before discharge from ICU - No correlation was found between VC and functionality measurements and muscle strength on day 1 or day of discharge |
RESULTS
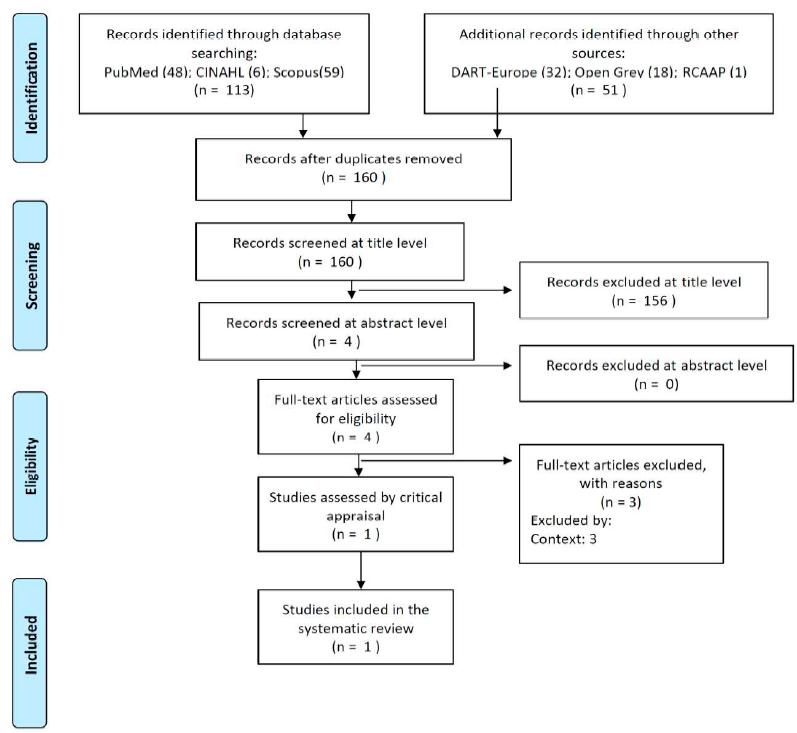
A total of 160 abstracts were reviewed, and 4 articles met the inclusion criteria and were reviewed in their entirety. Subsequently, 1 article fulfilling all of our inclusion criteria underwent a methodological quality assessment using the JBI Critical Appraisal Checklist for JBI Critical Appraisal Checklist for Randomized Controlled Trials.13 The stages of the systematic review process can be seen in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram (Figure 1).
Study Characteristics, Settings, and Sample
The included study was published in 2016.14 It was conducted in Brazil. The study setting was the Intensive Care Unit. There aren’t any studies in surgery wards or post-anesthesia care. The sample size included 38 patients over 18 years who underwent abdominal surgery, with or without pulmonary complications. Measurement of vital capacity (VC) was performed as described by the American Thoracic Society and by the European Respiratory Society.15 In this study there was no significative pulmonary complications in either group. There was no data referring to hospital length-of-stay or readmissions. The incentive spirometer group was used in three series of ten repetitions each. The professionals involved in this study were physical therapists.
DISCUSSION
Abdominal surgery, both, lower or upper, takes pulmonary risks to the patient.5 Thus, we sought to validate scientific evidence that substantiated the importance of incentive spirometry, in the postoperative period of laparotomy surgery, regarding specific complications such as atelectasis, residual volume reduction, secretions, among others. The importance of respiratory therapy or rehabilitation in the context of effective pulmonary recovery is commonly recognized.10,16
However, much of the scientific evidence is based on several other techniques in combination or supported by spirometry. Thus, arises the need to approach incentive spirometry, either volume or flow, alone. That said, having defined the terms of this systematic review, we found one study regarding the usefulness of incentive spirometry in reducing postoperative complications in abdominal surgery. A randomized clinical trial by Fernandes, et al.,14 divided the patients into a Positive Intermittent Pressure (PIP) Group and into a Volumetric Incentive Spirometer (VIS) Group. Both groups did the following exercises: lower limb free or assisted active exercises, respiratory physiotherapy associated to upper limb free or assisted active exercises, assisted cough, and, if necessary, nasotracheal aspiration. The study states that independently of the technique or devices, respiratory rehabilitation is always beneficial for the patient. This is a randomized trial so it has a high degree of evidence, however the type of abdominal surgery was different in both groups. In the VIS group the prevalence of lower abdominal surgery was higher (83,3%) and in the PIP group the prevalence of upper abdominal surgery was higher (80%). Even though the literature states that upper abdominal surgeries tend to trigger more pulmonary complications5,17 this study did not show significant pulmonary complications.
Some factors, such as the population being exclusively obtained in contexts of post-anesthesia care unit, intensive care units and surgery wards, where the number of patients are usually reduced and with short duration of hospitalization, may be the reason why there is a reduced number of studies. This study was done by physical therapists, however depending on the country this is a task related to rehabilitation nurses, who have a lack of published studies, so the need for further studies emerges, in order to verify the use of incentive spirometry alone or in combination with other techniques, as it seems that the combination of both does not raise any doubt in benefits for the user. This idea is reinforced by Manzano, Carvalho, Ramanhola & Vieira16 since it uses and demonstrates the validity of spirometry in the functional assessment of lung capacity in the pre and postoperative period, stating that it is somewhat controversial. The patient may not present its maximum vital capacity due to several factors, and there seems to be no additional information with the use of spirometry as a predictive factor in relation to the normal clinical information.
CONCLUSION
This study revealed that information regarding the use of incentive spirometry in the postoperative period of laparotomy is poorly disseminated, and only 1 study was found. Thus, further studies should be conducted to evaluate the relevance of the use of incentive spirometry in the post-laparotomy surgery, in order to prevent complications inherent to the procedures. It seems that manual techniques are more used than incentive spirometry, which seems to assume only a predictive character of the pulmonary function of the patient.
This systematic review is intended as a starting point for the systematization of the main evidence in this thematic area. This systematic review is expected to enhance new scientific developments, including the identification of potential intervention foci, with significant results for good clinical practice.
It is also intended that this review can substantiate the need for the development of a new and improved research line, as well as the optimization of study designs and research methodologies to be implemented in future studies.