INTRODUCTION
Worldwide, cerebrovascular accident (CVA/Stroke) is classified as the second leading cause of death and it is a pathological process with a significant impact on public health due to its serious social and economic consequences(1, 2).
Regardless of whether it is an ischemic or hemorrhagic stroke, depending on the affected areas of the brain, the person may present various changes in what concerns mobility, sensitivity, language, vision, swallowing, cognitive ability and elimination(3, 4, 5). The truth is that two-thirds of stroke survivors are discharged from hospital with a disability6.
Irrespective of the affected brain territory, the sequel that lasts the longest is the decrease or absence of muscle strength (paresis/plegia) in the hemibody contralateral to the brain injury, thus hemiplegia is the main cause of disability3.
Immediately after the stroke, there is a period of time known as brain shock and its duration is varied and may last for a few days or weeks. At this stage, muscle tone is hypotonic and people experience difficulty in mobilizing the affected limbs and in facial, tongue and trunk movements5. Due to hypotonia, the affected hemibody is flaccid and without voluntary movement, hence it leads to the loss of awareness and the appearance of inappropriate movement patterns. Regaining muscle strength may be accompanied by the development of the spastic pattern5. Spasticity is defined as an “uncontrolled contraction of skeletal muscles; increased muscle tone; muscle stiffness and uncoordinated movements”7. Its installation speed is related to the location and severity of the brain injury or the absence of a rehabilitation program. Previous research has confirmed that 40-60% of people after stroke develop spasticity(8, 9).
After a long investment in this field, in 1979, Johnstone described the spastic pattern and hence become a world reference in the rehabilitation of the person after a stroke. As described by the author, when spasticity settles in the upper limb, the person presents the following posture: shoulder retraction, depression and internal rotation, elbow flexion and forearm pronation, finger flexion and adduction. Although it is less frequent, when spasticity develops in the lower limb, there is retraction, extension and external rotation of the hip, extension of the knee and ankle, inversion and plantar flexion. In addition, lateral trunk flexion to the affected side is added10.
When the spastic pattern is installed, it causes motor and balance changes, self-care dependence, pain, joint stiffness, muscle contractures and pressure ulcers, contributing to a decrease in the quality of life(11, 12, 13). Spasticity, not only negatively affects the life of the sick person and of their family, but also increases healthcare costs. In a research carried out, the authors concluded that on average the healthcare cost of people with spasticity is twice as high when compared to people without spasticity. In addition, people with spasticity were hospitalized longer and more frequently14.
Caring for people with stroke requires systematic work by the entire team, with special emphasis on the nursing professionals. During the acute phase, their interventions prevent complications and/or their early detection, later, in a post-acute phase, it acquires special focus on empowering the person for self-care, which can be deeply conditioned by spasticity(9, 11). Of all the interventions that are relevant to the prevention of spasticity, the anti-spastic positioning pattern is of particular importance and it should be performed since the acute phase. In this sense, having as a reference a fully or partially compensatory system and/or a support and education system15, nurses play a crucial role, not only in the correct execution of the positioning in an anti-spastic pattern, but also in teaching, instructing and training different types of positioning, so that the person may maintain the anti-spastic position, 24 hours a day.
The anti-spastic pattern must be meticulously followed, when the person is lying down or sitting, with the shoulder in protraction and external rotation; the elbow in extension; the forearm in supination; fingers in extension and abduction; the hip in protraction, flexion and internal rotation; the knee and ankle in flexion and trunk elongation on the affected side(10, 16, 17).
Considering that spasticity leads to a decreased quality of life, to dependence in self-care and commitment to recovery and knowing that anti-spastic positioning prevents its onset or prevents its worsening, it was considered important to understand whether the positioning is performed in an anti-spastic pattern during hospitalization.
In this sense, this study it analyzes whether the positioning is performed in an antispastic pattern in persons following a cerebrovascular accident (Stroke), which positions are most used and whether these decisions are influenced by the characteristics of patients or of the nurses.
METHODOLOGY
A quantitative and cross-sectional study was carried out in a hospital located in Northern Portugal. The sample consists of the pattern positioning performed by nurses in persons after a cerebrovascular accident, admitted to a neurology ward service. The sampling technique is a non-probability and was selected by convenience, considering that was observed the positioning performed on people after stroke who were hospitalized and the nurses who were working at the moment when an observer was available. The following inclusion criteria was defined: positioning performed in people admitted to a neurology ward with a diagnosis of Stroke and were registered in the SClínico (computer program of the Portuguese National Health System) as having a moderate or high degree of dependence in positioning themselves and who presented, according to the Medical Research Council Scale, muscle strength ≤ 3 in at least one of the limbs.
The sample was calculated based on the number of people hospitalized with Stroke in the previous year, multiplied by the national average length of stay in hospital and the estimated average of positioning performed within 24 hours. Thus, it was taken into account that in 2018, 328 persons with a diagnosis of Stroke were admitted to this ward and, on average, six daily positions were performed and the national average length of hospital stays in Portugal, in 2018, was 8.6 days18. As a result of this data was obtained a value of 16925, which provides a prediction of 376 positions, hence it guarantees a confidence interval of 95% and a margin of error of 5%. Thus, the sample consisted of 376 positions, performed by 34 nurses in 23 persons after Stroke.
To carry out the data collection, was created an instrument consisting of three parts. The first part, referred to the nurses’, who performed the positioning, sociodemographic and professional data. The second part, referred to the sociodemographic data and to the persons’ after Stroke health condition. Regarding the health condition, was evaluated the state of consciousness - Glasgow Coma Scale (GCS); spasticity - Modified Ashworth Scale; muscle strength - Scale of the Medical Research Council, as well as the joint range of motion of the hemibody on the affected side. This part of the instrument also integrated the Barthel Index. The third part, included a grid for observing the positioning in an anti-spasticity pattern on the bed (dorsal decubitus, lateral decubitus for the affected side and lateral decubitus for the non-affected side) and on the chair. The grid was built taking into account the anti-spasticity pattern defined by Margaret Johnstone10.
Data collection was carried out between February and May 2019, after obtaining authorization from the ethics committee of the organization where the study was carried out. Was observed the positioning of all of the body segments, assigning 1 point, when it was not in accordance with the anti-spastic pattern and 2 points, when it was in the anti-spastic pattern. The total score of each positioning corresponds to the sum of the score attributed to the position of each body segment. Later, to facilitate the analysis, the average rating of each positioning was calculated.
The fact that the observations were always carried out by the same researcher should be highlighted. After being informed about the study’s objectives, both the nurses and the patients or their legal representatives signed informed consent, guaranteeing confidentiality and anonymity.
For data statistical treatment, we used the Statistical Package for Social Science (SPSS), version 26, with descriptive and inferential analysis, using non-parametric tests, namely the Mann-Whitney U test applied to independent samples and the Kruskal-Wallis test applied to independent samples, according to the variables under study.
RESULTS
Of the 34 nurses who performed positioning, 81.2% were female, with a mean age of 30.8 years (SD=6.2) and 48.0% had a specialization in rehabilitation nursing. The average professional practice time was 8.2 years (SD=6.4), while in the neurology ward the average time was 5.3 years (SD=6.5).
As for the people in whom positioning was performed, 65.5% were male, with an average age of 79.7 years (SD=7.3). The minimum age was 66 years and the maximum 94 years and 59.9% of the positioning was performed in people over 80 years. In what concerns the type of Stroke, in 58.6% of the cases it was ischemic, in 9.5% was hemorrhagic and in 1.9% it was ischemic with hemorrhagic transformation. The number of days that people stayed in hospital ranged between 3 and 75 days, with an average of 27.8 days in hospital (SD=22.95).
Regarding health condition, 54.9% of the people had the left hemibody affected, 43.8% the right and 1.3% bilateral commitment. The participants' state of consciousness ranged between 5 and 15 points on the GCS with an average score of 12.7 (SD=2.18 points). 25.7% of the participants had an GCS score of 15 points and 4.9% obtained 14 points. In relation to spasticity, it was found that 49.6% of the participants did not present spasticity in the upper and lower limbs when the evaluation took place, however, in 20.2% of the cases the installed spasticity in the upper limb was grade 4. After evaluating the muscle strength of the affected side, it was found that 60-70% of the participants had grade 0 in the muscle groups of the upper limb and 35-45% of the people had grade 2 in the muscle groups of the lower limb. Regarding the joint range of motion, although in the shoulder, elbow, fingers and toes, hip and ankle it was decreased in most of the observations, it was in the shoulder joint that a decreased range of motion was found more frequently (62.3%). After applying the Barthel Index, 90.5% were totally dependent and 9.5% were severely dependent.
Of the 376 positions observed, 43.2% took place during the night shift, 35.5% during the afternoon shift and 21.2% during the morning shift. Concerning the type of positioning, 40.4% of the observations referred to supine, 28.2% to lateral decubitus to the affected side, 23.9% to lateral decubitus to the unaffected side and 7.4% to positioning in the chair.
Regarding the supine position, which corresponded to 152 positions (40.4%), Table 1 displays the data collected from the observations. In more than 50% of the observations, the shoulder was not in protraction, the affected upper limb was not on a pillow from the scapula, the shoulder was not in external rotation, the elbow was not in extension and the forearm was not in supination, consequently these segments, in most observations, did not meet the anti-spastic pattern. In the lower limb, in more than 50% of the observations, the hip was not in protraction and the ankle was not in flexion.
In the observation of the dorsal decubitus position, it was found that the classification varied from 16 to 28, with a minimum of 14 for - no segment correctly positioned and a maximum of 28 for - all segments well positioned. The average classification was 21.6 (SD=2.92) and the mode 20, highlighting the fact that, no situation occurred in which all of the segments were totally misplaced, however only 0.7% had the maximum score.
Concerning lateral decubitus for the affected side, a total of 106 positions (28.2%) were observed. The observational data is displayed in Table 2. As to the upper limb, in more than 50% of the observations the shoulder was not in external rotation, the elbow was not in extension and the forearm was not in supination. Regarding the lower limb, in 86.8% of the observations, the ankle was not in flexion.
Table 1 Records of the observations of the supine positioning in an anti-spastic pattern
| Anti-spastic pattern positioning | Yes | No | |||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Positioning of the affected upper limb | |||||
| 1 | The shoulder is protracted. | 53 | 34.9 | 99 | 65.1 |
| 2 | The affected upper limb is on a pillow from the shoulder blade. | 38 | 25.0 | 114 | 75.0 |
| 3 | The shoulder is in external rotation. | 34 | 22.4 | 118 | 77.6 |
| 4 | The elbow is in extension. | 61 | 40.1 | 91 | 59.9 |
| 5 | The wrist is in extension. | 142 | 93.4 | 10 | 6.6 |
| 6 | The forearm is in supination. | 26 | 17.1 | 126 | 82.9 |
| 7 | The fingers of the hand are in extension. | 120 | 78.9 | 32 | 21.1 |
| 8 | The fingers of the hand are in abduction. | 122 | 80.3 | 30 | 19.7 |
| Positioning of the affected lower limb | |||||
| 9 | The hip is in protraction. | 57 | 37.5 | 95 | 62.5 |
| 10 | The hip is in slight flexion. | 147 | 96.7 | 5 | 3.3 |
| 11 | The leg is in internal rotation. | 99 | 65.1 | 53 | 34.9 |
| 12 | The knee is in flexion. | 146 | 96.1 | 6 | 3.9 |
| 13 | The ankle is in flexion. | 37 | 24.3 | 115 | 75.6 |
| 14 | With deviation of body alignment by hip protraction. | 66 | 43.4 | 86 | 56.6 |
Fonte: prepared by the authors
Table 2 Records of the observations of the lateral decubitus for the affected side positioning in an anti-spastic pattern
| Anti-spastic pattern positioning | Yes | No | ||||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| Positioning of the affected upper limb | ||||||
| 1 | The affected upper limb is propped up in bed. | 70 | 66.0 | 36 | 34.0 | |
| 2 | The shoulder is in protraction. | 97 | 91.5 | 9 | 8.5 | |
| 3 | The shoulder is in external rotation. | 43 | 40.6 | 63 | 59.4 | |
| 4 | The elbow is in extension. | 50 | 47.2 | 56 | 52.8 | |
| 5 | The forearm is in supination. | 37 | 34.9 | 69 | 65.1 | |
| 6 | The wrist is in extension | 96 | 90.6 | 10 | 9.4 | |
| 7 | The fingers of the hand are in extension. | 82 | 77.4 | 24 | 22.6 | |
| 8 | The fingers of the hand are in abduction. | 81 | 76.4 | 25 | 23.6 | |
| Positioning of the affected lower limb | ||||||
| 9 | The hip is in slight flexion. | 104 | 98.1 | 2 | 1.9 | |
| 10 | The hip is in protraction. | 96 | 90.6 | 10 | 9.4 | |
| 11 | The leg is in internal rotation. | 102 | 96.2 | 4 | 3.8 | |
| 12 | The knee is in flexion. | 106 | 100 | 0 | 0.0 | |
| 13 | The ankle is in flexion. | 14 | 13.2 | 92 | 86.8 | |
| 14 | Maintains body alignment. | 86 | 81.1 | 20 | 18.9 | |
Fonte: prepared by the authors
In lateral decubitus positioning for the affected side, the classification varied between 19 and 28, for a minimum of 14 and a maximum of 28. It was found that the average classification was 24.0 (SD= 2.09) and the mode 23, emphasizing that there was no situation of totally incorrect positioning, however only 1.0% presented the maximum classification.
As regards the lateral decubitus position for the non-affected side, which corresponded to 90 positions (23.9%), in most observations the upper limb was positioned in an anti-spastic pattern with the exception of the shoulder, since it was not in external rotation in 91.1% of the positions.
As for the affected lower limb, most segments complied with the anti-spastic pattern, the lowest percentage was 74.4% (corresponding to hip protraction) and in 100% of the cases the knee was in flexion. However, in 84.3% of the positioning the ankle was not in flexion, not meeting the anti-spastic pattern (Table 3).
Table 3 Records of the observations of the lateral decubitus for the non-affected side positioning in an anti-spastic pattern.
| Anti-spastic positioning pattern | Yes | No | |||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Positioning of the affected upper limb | |||||
| 1 | The affected upper limb is resting on a pillow. | 81 | 90.0 | 9 | 10.0 |
| 2 | The shoulder is in protraction. | 47 | 52.2 | 43 | 47.8 |
| 3 | The shoulder is in external rotation. | 8 | 8.9 | 82 | 91.1 |
| 4 | The elbow is in extension. | 58 | 64.4 | 32 | 35.6 |
| 5 | The wrist is in extension. | 85 | 94.4 | 5 | 5.6 |
| 6 | The fingers of the hand are in extension. | 73 | 81.1 | 17 | 18.9 |
| 7 | The fingers of the hand are in abduction. | 66 | 73.3 | 24 | 26.7 |
| Positioning of the affected lower limb | |||||
| 8 | The hip is in prostration. | 67 | 74.4 | 23 | 25.6 |
| 9 | The leg is in internal rotation. | 78 | 86.7 | 12 | 13.3 |
| 10 | The hip is in flexion. | 89 | 98.9 | 1 | 1.1 |
| 11 | The knee is in flexion. | 90 | 100 | 0 | 0.0 |
| 12 | The ankle is in flexion. | 15 | 16.7 | 75 | 83.3 |
| 13 | Maintains body alignment | 73 | 81.1 | 17 | 18.9 |
Fonte: prepared by the authors
Regarding decubitus for the non-affected side, the classification varied between 18 and 26, for a minimum of 13 points and a maximum of 26 points. It was found that the positioning score obtained a mean of 22.2 (SD=1.92) and a mode of 24, with only 1.1% achieving the maximum score.
Sitting, was only observed 28 times (7.4%) and always during the morning shift. If we take a closer look at Table 4 we can see that all the chairs had a wide base and adequate arms, however, only in 57.1% of the situations the height of the chair enabled a 90 degree knee flexion. In most observations, the knees were bent at 90 degrees, people had a support table, their forearms were resting on the table, their wrists were in extension, their fingers were in extension and abduction and their body alignment was maintained. Nevertheless, in 53.6% of positioning the trunk was not inclined forward and in 57.1% of positioning the forearms were neither inclined forward nor parallel.
In the sitting position the classification varied from 16 to 22, for a minimum of 11 and a maximum of 22. It was found that the distribution obtained an average of 20.0 (SD = 1.63) and it should be highlighted that of the 28 observations in the sitting position, only 17.9% achieved the maximum score.
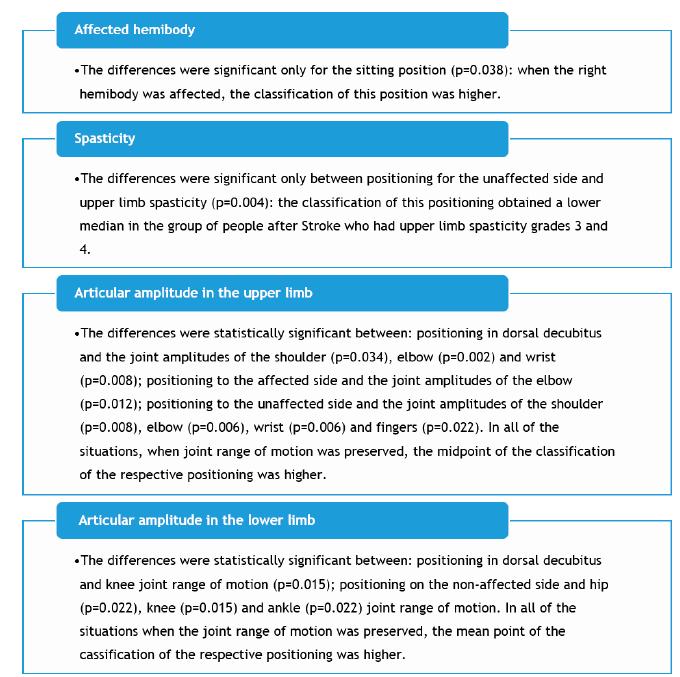
When analyzing the results concerning the classifications attributed to the post-stroke positions and characteristics, differences were found regarding the variables affected hemibody, spasticity and joint amplitude (Figure 1).
Table 4 Records of the observations of the characteristics of chairs and seating positioning in an antispasmodic pattern
| Chair features | Yes | No | |||
|---|---|---|---|---|---|
| n | % | n | % | ||
| 1 | The chair has a wide base. | 28 | 100 | 0 | 0.0 |
| 2 | The chair has adequate armrests. | 28 | 100 | 0 | 0.0 |
| 3 | The height of the chair enables a 90º bending of the knees. | 16 | 57.1 | 12 | 42.9 |
| Positioning the person sitting on a chair | |||||
| 4 | The knees are bent at 90º. | 27 | 96.4 | 1 | 3.6 |
| 5 | The person has a support desk. | 27 | 96.4 | 1 | 3.6 |
| 6 | The trunk is leaning forward. | 13 | 46.4 | 15 | 53.6 |
| 7 | The forearms are resting on the table. | 27 | 96.4 | 1 | 3.6 |
| 8 | The forearms are bent forward and parallel. | 12 | 42.9 | 16 | 57.1 |
| 9 | The fists are in extension. | 28 | 100 | 0 | 0.0 |
| 10 | The fingers of the hand are in extension to abduction. | 24 | 85.7 | 4 | 14.3 |
| 11 | Maintains body alignment | 22 | 78.6 | 6 | 21.4 |
Fonte: prepared by the authors
Regarding the classifications assigned to the positioning and the nurses’ characteristics, there were differences concerning the variables gender and professional training. With regard to gender, the differences were significant only for the sitting positioning (p<0.001), and the mean rating of this positioning was higher in female nurses. As regards professional training, the differences were significant for the positioning in dorsal decubitus (p<0.001) and for the positioning on the non-affected side (p<0.001), and in the group of Specialist Nurses in Rehabilitation Nursing (SNRN) the median classification of these two positioning was higher than in the other two groups - graduate nurses and specialist nurses in other fields.
DISCUSSION
Some of the socio-demographic variables are risk factors for Stroke. Regarding age, it is known that as age advances, the risk of Stroke increases. In a research carried out in 2019, 49.3% of the participants were aged 65 or older8. In the present study, all participants were aged over 65 years. Male gender was adduced to a higher risk of Stroke (19,20, which is in line with this study, in which 65.5% of the people after Stroke were male. Most observations were performed in persons with ischaemic Stroke, which are in line with the literature19,20. In a research conducted between January 2010 and December 2016, in a total of 1200 patients, 63.0% had a diagnosis of ischaemic Stroke, 17.2% haemorrhagic Stroke and 19.8% Transient Ischaemic Attack (TIA)21.
With regard to the patients’ state of consciousness, more than half presented alterations, this fact is extremely important since these alterations may condition the recovery process3,22. Regarding spasticity, a research revealed that in the first 10 days after a haemorrhagic Stroke, 58.1% of the participants developed mild spasticity (grade 1 or 1+), where as in participants with ischemic Stroke, only 36.2% had no spasticity8. Contrarily to the above-mentioned in the present study, almost 50% of the people following Stroke did not present spasticity at the moment of the evaluation, and afterwards there was a higher frequency of people with grade 4 in the affected upper limb and grade 2 in the affected lower limb. Another research23 concluded that the prevalence of spasticity following Stroke, during the first three months was 17-25% and that the severity of spasticity was more incident in the upper limbs, just as demonstrated in the present study.
Most positioning observations were carried out on totally dependent people, which confirms the inability to perform activities inherent to self-care after the Stroke (16,24.
As far as professionals are concerned, more than 80% of the positioning were performed by nurses, which is in agreement with the national reality of the profession25. On the other hand, when the study was carried out, although most of the registered nurses in Portugal were aged between 31 and 35 years25, in this study the highest percentage was between 23 and 30 years. As for the specialization field, most positioning were executed by Specialized Nurses in Rehabilitation Nursing (SNRN), followed by nurses with a degree. The data is not in accordance with the reality of the profession25 since in the year in which the study was carried out, there were 56046 general care nurses and only 20003 specialist nurses, however, the realities of the different services are disparate since there are services without specialist nurses and other services with several.
Although the anti-spastic positioning in dorsal decubitus should be the least performed, it was found to be the most commonly performed. Considering that it is the positioning that most promotes spasticity, whenever it is necessary to perform it, the fulfilment of the anti-spastic pattern should be guaranteed10. However, it was found that in only 0.7% of the observations the classification was maximum. Furthermore, when the average classification of this positioning was compared to the others, we concluded that it was the positioning that was most distant from the maximum value, i.e., it was the positioning in which the anti-spastic pattern was often not fulfilled. The most frequently missed positioning was forearm supination, followed by shoulder external rotation and ankle flexion. This may be due to therapeutic positioning being distinct from positioning in an anti-spastic pattern and perhaps the nurses could have performed therapeutic positioning26.
As regards the anti-spastic positioning in lateral decubitus for the affected side, which provides more sensory stimuli, it was confirmed that it was the best performed, considering that it obtained a higher average classification than the others. However, there were also errors in their execution and the position that most failed was the ankle flexion, followed by forearm supination. Another point to consider in the lateral decubitus for the affected side is the need for correct positioning of the shoulder, as this decubitus is more likely to trigger changes in the shoulder, such as painful shoulder syndrome27, which may condition the recovery process and lead to disability(3, 28). According to this study’s findings, the shoulder was in protraction in 91.5% of the people, but on the other hand it was only in external rotation in 40.6% of the cases.
The anti-spastic positioning in lateral decubitus for the non-affected side, is the one that most inhibits spasticity16, hence it should be more performed during the 24 hours, however it was the third most observed positioning. On the other hand, it was evidenced that it was the second positioning with the best average classification. The positioning that was less performed was the external rotation of the shoulder, as well as the flexion of the ankle. It should be emphasized that failure to flex the ankle increases the risk of equinus foot, which can lead to numerous complications such as impaired walking.
To perform positioning in an anti-spastic pattern it is necessary that the sick persons have sufficient mobility for the nurse to position the limbs in the correct position.
If the person presents grade 2 installed spasticity, he/she already shows a marked increase in tone in most of the movement amplitude, which worsens with the increase in the degree of spasticity and in grade 4 the affected parts are rigid to flexion or extension, which makes it impossible to perform a correct positioning10. In this study, significant differences were confirmed between the classification of the positioning for the non-affected side and the degree of spasticity and the median classification of this positioning was lower in people who presented in the upper limb spasticity higher than grade 2 and in the lower limb higher than grade 1+.
The sitting position was the least observed, which may be due to the fact that it is more often performed during the morning shift, where only 21.2% of the positions were observed. In addition, the first lifting after Stroke may take a few days, hence it limited the observation of this positioning. It should be highlighted that significant differences were identified in the classification of this positioning in relation to the affected hemibody and that in patients who had the right hemibody affected, the median classification of the positioning was higher. The fact that the right hemibody is dominant may possibly increase the nurses' attention.
Joint mobility influences the positioning in an anti-spastic pattern because its decrease may lead the nurse to be unable to perform the positioning in an anti-spastic pattern. When the findings of this variable were analysed, significant differences were confirmed between: positioning in dorsal decubitus and the joint range of motion of the shoulder, elbow, wrist and knee; positioning for the affected side and the range of motion of the elbow; positioning for the non-affected side and the range of motion of the shoulder, elbow, wrist, fingers, knee and ankle, showing that when the joint range of motion was preserved the midpoint in the classification of the 3 types of positioning was higher. This may be due to the fact that the preserved joint amplitude facilitates correct positioning.
Although the average of none of the positions was lower than the established cohort value, the percentage of positioning with the maximum rating was small. It is noteworthy that SNRN performed positioning in anti-spastic pattern in the dorsal decubitus and lateral decubitus for the unaffected side better, when compared to general care nurses and nurses with other specialties. This may be related to the fact that the training program of the specialty in rehabilitation nursing includes the improvement of skills in this field.
Despite the relevance of the results, we must assume that the fact that a mixed research was not carried out is a limitation of the present study. The existence of a qualitative approach would permit a deeper understanding of this issue. In addition, although the scarce scientific production in this field hampered the discussion, we hope that this study may trigger reflection on the topic.
CONCLUSION
The results of this study confirm that, during hospitalization, nurses do not systematically position persons following Stroke in an anti-spastic pattern.
The anti-spastic positioning in dorsal decubitus was the one that presented the most gaps and it should also be highlighted that in this positioning, as in all the other positioning, ankle flexion was the least verified, which may contribute significantly to equinus foot and consequently gait compromise.
Among the contributions of this study, we underline the need to rethink the approach of this content in the basic and specialized nursing training, as well as in life-long learning/training. Taking into account SNRN skills, they should raise the nursing team's awareness that anti-spastic positioning plays a crucial role in the recovery process.
The replication of this study in other clinical practice settings, as well as the conduct of qualitative research would facilitate the compression on the nurses' decision-making process and the gaps evidenced in the different positions.