Introduction
Deep neck infections (DNI) are defined as an abscess or cellulitis located in the cervical spaces limited by layers of the deep cervical fascia 1. These infections may rapidly spread through the cervical fascia planes and descend to the mediastinum 2. Thus, DNI are associated with lethal and high morbidity complications, such as mediastinitis, Lemierre Syndrome or necrotizing fasciitis 3. To optimize the treatment of DNI, clinicians must be aware of the epidemiology and factors leading to unfavorable outcomes.
The main objective of this study is to analyze the epidemiology and predictive factors of mediastinitis in DNI.
Methods
Retrospective observational study including every adult patient submitted to surgery due to DNI in the otorhinolaryngology department of a tertiary hospital center from January 2015 to December 2021. Exclusion criteria were patients with isolated peritonsillar abscess and the presence of a malignant head and neck tumor.
Patients were all treated according to the department’s protocol for DNI. Every patient performed blood analysis and a contrast enhanced computed tomography (CT) scan previously to the surgery. The type of surgery (intra-oral or external drainage) was chosen according to the clinical and imaging examination and purulent exudates were collected in every case for microbiological assessment. Antibiotic therapy was initiated empirically with ceftriaxone (1 g/IV/q.12.h.) and clindamycin (600 mg/IV/q.6.h.) and was directed after antimicrobial susceptibility tests. Drains were placed in every patient submitted to external drainage and daily lavages were performed with Microdacyn®.
Data was analyzed retrospectively to assess patients’ demographics (age, gender) and clinical history (DNI etiology, previous antibiotic therapy, symptoms duration, other diseases), blood tests at admission (C-Reactive Protein - CRP, leucocyte count, lymphocyte count, neutrophil count and neutrophil to lymphocyte ratio - NLR), purulent exudate cultures and contrast enhanced CT scan (involved spaces, highest dimensions, infra-hyoid extension and presence of gas), treatment, hospitalization days and complications of DNI. Furthermore, patients who developed mediastinitis were compared with patients with isolated DNI to assess prognostic factors leading to mediastinitis.
A descriptive analysis of patient’s characteristics was performed taking into consideration absolute and relative frequencies for categorical variables, mean and standard deviation for normally distributed continuous variables and median and range for non-normally distributed continuous variables. Normality of continuous variables was assessed with the Kolmogorov-Smirnov Test. Association of different variables with mediastinitis was analysed with Chi-square Test or Fischer’s Exact Test for categorical variables, Student’s T Test for normally distributed continuous variables and Mann-Whitney U Test for non-normally distributed continuous variables. A multivariate analysis taking into consideration age, aetiology, laboratory parameters (neutrophil count, lymphocyte count and NLR), CT parameters (highest dimensions, infra-hyoid extension, and the presence of gas), location and laterality was performed using a logistic regression to assess predictive factors of progression to mediastinitis. All statistical analysis was made with the software IBM® SPSS® Statistics version 27 and associations were considered significant when p<0,05.
Results
Epidemiology of DNI:
A total of 165 patients with DNI were included. Mean age at presentation was 48,5 ± 16,6 years, there was a male predominance (n=106; 64,2%) and 23 patients (13,9%) had diabetes mellitus (DM). Median symptom duration until otorhinolaryngological evaluation was 5 (1-30) days and 105 (63,6%) patients had taken antibiotics previously, from which, 52,4% were under treatment with amoxicillin with clavulanic acid.
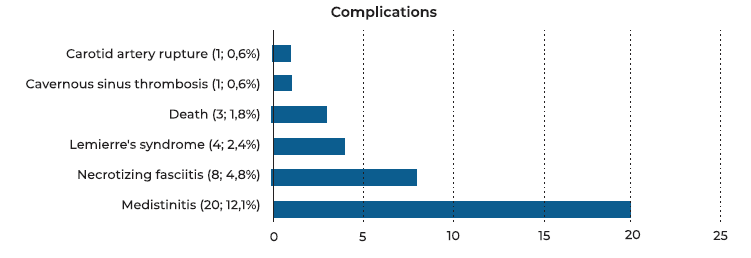
Most patients (n=134; 81,2%) were submitted to external cervical drainage while the remaining were submitted to intra-oral drainage (n=31; 18,2%). After surgery, median hospitalization days were 10,5 (1-133) days and 40 (24,2%) of the patients required a re-intervention. Registered complications are reported in Figure 1. The most common complication was mediastinitis in 20 (12,1%) patients.
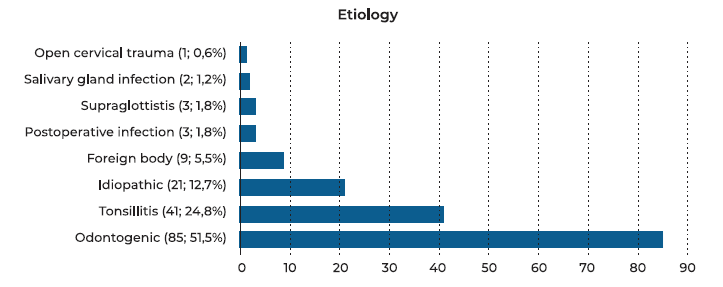
The most frequent etiology was odontogenic infection (n=86, 52,1%) and the second most common was tonsillitis (n=42; 25,5%). Etiologies are shown in Figure 2. Furthermore, the most frequently involved neck space was the submandibular space (n=100; 60,6%) followed by the parapharyngeal space (n=69; 41,8%), as reported in Figure 3.
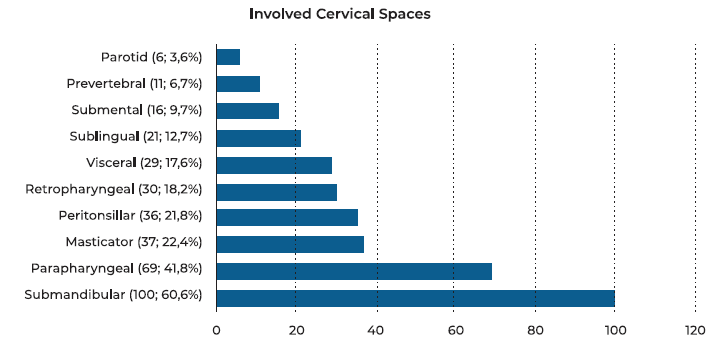
Figure 3 Neck Spaces Involved by DNI; the sum up of percentages is higher than 100% because one DNI may involve more than one neck space.
Samples for bacterial cultures were obtained in every surgery and cultures are reported in Table 1. When considering every patient with DNI (n=165), cultures were negative in 76 (46,1%) cases and in 18 (10,9 %) were positive for multiple bacteria. The most common isolated organisms were Streptococcus Anginosus in 30 (33,7%) cultures, Streptococcus Constellatus in 28 (31,4%) and Prevotella Spp in 17 (19,1%). In patients with mediastinitis, cultures were negative in 9 (45%) cases and multiple bacteria were isolated in 3 (15%). The most common isolated bacteria in patients with mediastinitis were similar to what was reported for every patient with DNI, with Streptococcus Anginosus in 6 (54,5%) cultures, Streptococcus Constellatus in 2 (18,2%) and Prevotella Spp in 3 (27,3%).
Prognostic Factor for Progression to Mediastinitis
In a univariate analysis, progression to mediastinitis was associated with older age (p=0,007), tonsillitis (p<0,001), bilateral involvement (p<0,001), laboratory parameters such as neutrophilia (p=0,002), lymphopenia (p<0,001) and a higher NLR (p<0,001) and CT parameters such as higher dimensions (p<0,001), infra-hyoid extension (p<0,001) and the presence of gas (p<0,001). Furthermore, parapharyngeal (p=0,029), retropharyngeal (p<0,001), prevertebral (p<0,001) or visceral (p<0,001) locations were associated with mediastinitis while a submandibular location (p<0,001) was a protective factor.
In a multivariate analysis taking into consideration age, aetiology, laboratory parameters (neutrophil count, lymphocyte count and NLR), CT parameters (highest dimensions, infra-hyoid extension, and the presence of gas), location and laterality, the only factors associated with progression to mediastinitis were NLR (p=0,037) and a bilateral involvement (0,015).
Table 1 Results of bacterial cultures in Deep Neck Infection
| Cultures | Control (n=165) | Mediastinitis (n=20) |
| Negative | 76 (46,1%) | 9 (45 %) |
| Multiple Bacteria | 18 (10,9%) | 3 (15%) |
| Gram (+) Aerobic | ||
| Steptococcus Pyogenes | 3 (3,4%) | 0 |
| Streptococcus Anginosus | 30 (33,7%) | 6 (54,5%) |
| Streptococcus Constellatus | 28 (31,4%) | 2 (18,2%) |
| Streptococcus Epidermidis | 2 (2,2%) | 0 |
| Streptococcus Mitis | 2 (2,2%) | 0 |
| Steptococcus Agalactiae | 1 (1,1%) | 0 |
| Staphylococcus Aureus | 8 (9%) | 1 (9,1%) |
| Gram (-) Aerobic | ||
| Pseudomonas Aeruginosa | 1 (1,1%) | 1 (9,1%) |
| Klebsiella Pneumoniae | 1 (1,1%) | 0 |
| Anaerobic | ||
| Prevotella spp | 17 (19,1%) | 3 (27,3%) |
| Fusobacterium spp | 7 (7,9%) | 0 |
| Enterobacter spp | 3 (3,4%) | 1 (9,1%) |
| Eikenella spp | 3 (3,4%) | 0 |
| Proteus spp | 1 (1,1%) | 0 |
Table 2 Univariate analysis assessing factors associated with progression to mediastinitis.
| Control (n=145) | Mediastinitis (n=20) | P | ||
| Gender1 | Male (n=104) | 62,8% | 65% | 1,00 |
| Age2 | 47 ± 16,1 | 60,2± 16,6 | 0,007 | |
| Diabetes Mellitus1 (n=23) | 13,1% | 20% | 0,487 | |
| Etiology1 | Idiopathic (n=21) | 11% | 25% | <0,001 |
| Tonsillitis (n=42) | 22,8% | 45% | ||
| Odontogenic (n=86) | 56,6% | 10% | ||
| Others (n=16) | 9,7% | 20% | ||
| Previous Antibiotic Therapy1 (n=104) | 64,1% | 57,9% | 0,619 | |
| Symptoms duration in Days3 | 5 ± 4 | 4 ± 3 | 0,224 | |
| Laboratory Parameters | CRP 2 | 175,86 ± 112,82 | 256,17 ± 125,03 | 0,708 |
| Leucocytes2 | 15,58 ± 6,08 | 15,37 ± 6,64 | 0,642 | |
| Neutrophils %3 | 79,6 ± 14 | 87 ± 7,1 | 0,002 | |
| Lymphocytes %3 | 9,8 ± 10 | 4,9 ± 4 | <0,001 | |
| NLR3 | 8 ± 10 | 18 ± 18 | <0,001 | |
| CT Scan Parameters | Highest Dimension3 | 43 ± 21 | 130 ± 81 | <0,001 |
| Infra-hyoid Extension1 (n=64) | 30,6% | 90,5% | <0,001 | |
| Presence of Gas 1 (n=39) | 16,7% | 75% | <0,001 | |
| Involved Neck Spaces1 | Peritonsillar (n=36) | 20% | 35% | 0,247 |
| Masticator (n=36) | 24,1% | 5% | 0,079 | |
| Parotid (n=6) | 4,1% | 0% | 0,610 | |
| Submandibular (n=98) | 65,5% | 15% | <0,001 | |
| Sublingual (n=21) | 14,5% | 0% | 0,079 | |
| Submental (n=16) | 10,3% | 5% | 0,696 | |
| Parapharyngeal (n=68) | 37,9% | 65% | 0,029 | |
| Retropharyngeal (n=30) | 11,7% | 65% | <0,001 | |
| Prevertebral (n=11) | 3,4% | 30% | <0,001 | |
| Visceral (n=29) | 10,3% | 70% | <0,001 | |
| Location1 | Unilateral (n=134) | 86,2% | 45% | <0,001 |
| Bilateral (n=31) | 13,8% | 55% | ||
| Surgery1 | External Drainage (n=132) | 79,3% | 85% | 0,767 |
| Intra-oral Drainage (n=33) | 20,7% | 15% |
1 - Chi-square or Fischer’s Exact Test; represented in percentage; 2 - Student T-Test; represented in mean ± standard deviation; 3 -Man-Whitney U test; represented in median ± interquartile range ; CRP - C-reactive protein; CT - computed tomography; NLR - neutrophil to lymphocyte ratio.
Table 3 Multivariate analyses assessing factors associated with progression to mediastinitis
| Odds Ratio | 95 %Confidence Interval | P | ||
| Age | 1,03 | 0,99 - 1,66 | 0,157 | |
| Etiology | 0,294 | |||
| Idiopathic | ||||
| Tonsillitis1 | 0,88 | 0,12 - 6,34 | 0,908 | |
| Odontogenic1 | 1,64 | 0,17 - 15,31 | 0,663 | |
| Others1 | 0,18 | 0,02 - 1,85 | 0,149 | |
| Laboratory | Neutrophils % | 0,93 | 0,82 - 1,06 | 0,269 |
| Lymphocytes % | 0,89 | 0,72 - 1,09 | 0,255 | |
| NLR | 1,08 | 1,00 - 1,15 | 0,037 | |
| CT Scan | Highest dimension | 1,01 | 0,99 - 1,03 | 0,297 |
| Infra-hyoid extension | 2,93 | 0,53 - 16,18 | 0,218 | |
| Presence of Gas | 0,31 | 0,06 - 1,44 | 0,134 | |
| Involved Neck Spaces | Submandibular2 | 1,24 | 0,28 - 5,38 | 0,777 |
| Parapharyngeal2 | 3,28 | 0,95 - 11,25 | 0,061 | |
| Retropharyngeal2 | 0,43 | 0,05 - 3,38 | 0,420 | |
| Prevertebral2 | 5,89 | 0,54 - 64,04 | 0,145 | |
| Visceral2 | 2,03 | 0,42 - 9,93 | 0,380 | |
| Location | Bilateral Abscess3 | 8,28 | 1,51 - 45,36 | 0,015 |
1- In 1 - In comparison with idiopathic; 2 - In comparison with all others; 3 - In comparison with unilateral abscess; CT - computed tomography, NLR - neutrophil to lymphocyte ratio.
Discussion
The main objective of this study was to evaluate clinical data regarding symptoms, etiology, blood tests, cultures, CT scans, treatment and predictors of mediastinitis in DNI submitted to surgery in the Otorhinolaryngology department of a Portuguese tertiary hospital center. The most common DNI etiology was odontogenic and the most frequently involved cervical space was the submandibular space. The most frequently isolated bacteria were from the Streptococcus Spp. Furthermore, the most important factors predicting progression to mediastinitis were the presence of a bilateral abscess or a high NLR.
Mean age at presentation was 48,5 years and there was a slight male predominance with 63,5% male patients. Demographic results in this study were in accordance with what was previously described in other cohorts 4,5,6 Regarding etiology, odontogenic infection was the most frequent cause of DNI which is supported by other studies 6,7. Although some studies have reported tonsillitis to be the most frequent cause of DNI, these studies registered a higher number of idiopathic infections which may have led to a bias 4,5. Moreover, the most frequent involved neck space in DNI seems to be the submandibular space 6,7,8, which further supports the role of odontogenic infections in the pathogenesis of most DNI.
Most studies agree that Streptococcus Spp are the most common bacteria isolated in cultures 4,6,8. On the other hand, the most frequent isolated Streptococcus subtypes differ from study to study, which may be related to different bacterial epidemiology in different countries. In a tertiary Portuguese hospital center, the most frequent isolated bacteria were Streptococcus Anginosus, Streptococcus Constellatus and anaerobic species, where the most common was Prevotella Spp. In accordance with what was reported by Kimura et al, isolated bacteria in DNI with or without mediastinitis seems to be similar 4.
DNI may rapidly spread through the neck until the mediastinum, leading to potential life-threatening complications such as mediastinitis, necrotizing fasciitis, Lemierre’s Syndrome, cavernous sinus thrombosis, carotid artery rupture or death. Thus, it is important to be aware of factors potentially leading to these complications to optimize treatment in patients with DNI. Older age at presentation was associated with progression to mediastinitis. In accordance, it was previously found that older age in patients with DNI was associated with multiple spaces involvement, complications, multiple surgical interventions, and higher hospitalization days 9. Although we have found no association of diabetes mellitus (DM) with progression to mediastinitis, a meta-analysis found that DM is associated with a higher rate of complications and involvement of multiple spaces 10. While tonsillitis was associated with progression to mediastinitis, other studies didn’t find any association 4,11. Further studies are required to understand if there is an association between DNI’s etiology and mediastinitis.
Kimura et al found in an adjusted analysis that age ≥55, NLR ≥13, and CRP ≥30 mg/dL were clinical predictors of mediastinitis 4, which further supports our findings of an association between NLR and mediastinitis. NLR reflects the dynamic relationship between the innate and adaptive immune responses and is used as a marker of systemic inflammation 12. It is a sensitive, non-specific marker of systemic infection, sepsis and bacteremia and higher values are associated with poorer prognosis 12. It is easy to measure, fast responding to inflammatory changes with dynamic alterations that may even precede alterations in the clinical state 12. Thus, NLR should be determined in every patient with DNI in order to assess the probability of complications such as mediastinitis. Since CRP is an acute inflammatory protein with higher levels associated sepsis and poorer prognosis 13, it was expected an association between CRP and mediastinitis which was not found in this cohort. Although further studies are required to understand if CRP might be a potential clinical predictor of complications in DNI, this study results show that NLR might be a more important clinical predictor in comparison to CRP.
CT parameters may also be adequate to predict progression to mediastinitis 4. In this study, there was an association with highest dimensions on CT scan, presence of gas and infra-hyoid extension. Furthermore, a parapharyngeal, retropharyngeal, prevertebral or visceral spaces involvement was associated with mediastinitis in accordance with what was previously reported 8,11. On the other hand, we have found no previous reports of a protective association between a submandibular space involvement and DNI complications.
This study has included a large sample, larger than most studies, which has enabled an adjusted analysis of clinical predictors of mediastinitis. On the multivariate analysis performed in this study, only NLR and a bilateral DNI were associated with progression to mediastinitis. Thus, we hypothesize that these may be the most important clinical predictors of mediastinitis.
This study has several limitations. Firstly, it is a retrospective observational study which might be associated with bias and limitations in data collection. For example, there was not enough data to assess causes for re-intervention. Furthermore, other complications beside mediastinitis had a small number of patients which didn’t allow to assess clinical predictors of different complications. Lastly, some patients with DNI were treated by stomatology, maxillofacial or general surgery departments (n=78) during the study period. While these patients were not included in the analysis, this may have led to a bias that may influence generalization of results.
Conclusion
The most frequent DNI etiology was odontogenic infection and the most common abscess location was the submandibular space. Furthermore, Streptococcus Spp were the most isolated organisms in cultures. The presence of a bilateral DNI and NLR seem to be the most important clinical predictors of mediastinitis.