Introduction
Monkeypox virus (MPXV) infection is a zoonotic disease transmitted by a species of the genus Orthopoxvirus. Endemic to central, east, and west Africa, it is transmitted to humans through the ingestion or handling of wild infected animals1. Human-to-human transmission can occur through non-intact skin and the ocular, nasal, oral, genital, and anal mucous membranes, respiratory droplets, and contaminated personal items.
Since May 2022, an unexpected outbreak of monkeypox has rapidly spread to all five continents and is now a global public health concern.
The incubation period of this virus typically lasts 7 to 21 days, and although the usual signs and symptoms are fever, asthenia, myalgia, dorsalgia, headache, and lymphadenopathy, cases of oral and oropharyngeal manifestations of the disease have been described2, which may often mimic other sexually transmitted infections (STIs).
It is difficult to diagnose MPXV based only on clinical symptoms; for this reason, patient specimen testing and molecular assays are useful and crucial for case confirmation.
Usually, it is a self-limiting disease that requires only supportive symptomatic care; however, there are reports of hospitalization due to aerodigestive tract symptoms3, severe disease or complications. Smallpox vaccination is known to provide good cross-protection against MPXV and other poxvirus members, and, despite falling vaccination rates after 1980, when the World Health Organization (WHO) declared that the smallpox virus had been eradicated, since 2021, authorities have approved the smallpox vaccine manufacture because of worries about the MPXV breakout and biological weapon attacks4. Antivirals, whose efficacy against MPX is unknown, are only used in severe cases4.
Case report
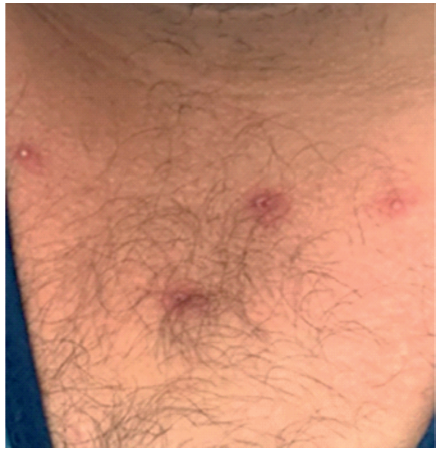
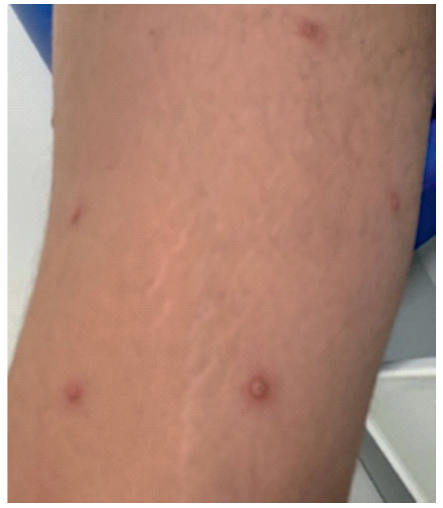
We present the case of a 23-year-old male patient who sought emergency care in June 2022 for odynophagia, total dysphagia, and 7 days of fever, treated with oral amoxicillin and clavulanic acid without improvement. On physical examination, he presented grade IV tonsils (Brodsky scale) with bilateral purulent exudate and without asymmetries or bulging of the soft palate (Figure 1). Nasofibrolaryngoscopy did not reveal other findings. A computed tomography (CT scan) suggests multiple bilateral tonsillar abscesses and voluminous reactive lymph nodes in the internal jugular, spinal accessory and submandibular chains (Figure 2). The laboratory analysis showed leukocytosis with neutrophilia and an increase in C-reactive protein. Due to the inability to tolerate oral feeding even after intravenous analgesia, hospitalization was decided for supportive fluid therapy and analgesia. On the third day of hospitalization, vesiculopustular skin lesions appeared on the upper and lower limbs and trunk (Figures 3 and 4). When questioned, he reported sexual contact with an asymptomatic same-sex individual a month earlier. He was examined by a dermatologist and an infectious disease specialist, who performed STIs screening (HIV, hepatitis B and C, herpes, syphilis, gonorrhea, and chlamydia), protein chain reaction (PCR) and culture of the pustule and oropharyngeal exudates, and pustule skin biopsy. Of the diagnostic tests performed, both the pustule and oropharyngeal exudates PCR tested positive for MPXV, and the histopathological examination of the pustule biopsy showed findings consistent with infection by this virus. He remained on contact and droplet isolation measures and was discharged after tolerating oral diet on the tenth day of hospitalization.

Figure 1 Oropharynx: grade IV tonsils on the Brodsky scale with bilateral purulent exudate and without asymmetries or bulging of the soft palate.
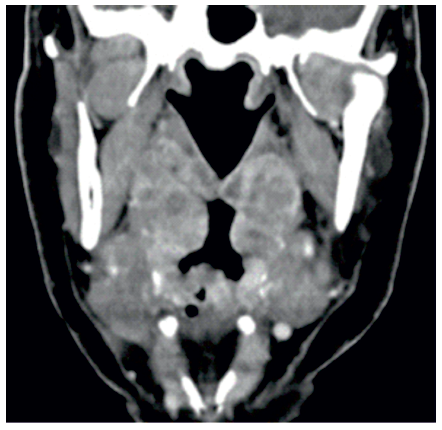
Figure 2 Cervical CT scan with intravenous contrast: multiple bilateral tonsillar abscesses and voluminous reactive lymph nodes in the internal jugular, accessory spinal, and submandibular chains.
Discussion
MPXV is not new, since African nations have been dealing with outbreaks of the virus for a long time. Although considered peculiar and atypical, oral and pharyngeal manifestations of this monkeypox outbreak may have a prevalence of around 36% of all infections5, which is why clinical assessment for patients with monkeypox or in high-risk locations for monkeypox should include oropharyngeal examination. Among these oropharyngeal manifestations, we highlight the most common: pharyngitis, tonsillitis, tonsillar abscesses, and ulcerated lesions of the oral mucosa that may evolve from vesicles to pustules. The oropharyngeal manifestations may be misdiagnosed as bacterial infections or confused with another STI, so the otolaryngologist should be alert to this pathology.
The management of this infection doesn't rely on medications designed specifically for MPXV. The majority of the patients with mild symptoms recover only with supportive measures such as analgesia and hydration. Drugs that inhibit viral DNA synthesis can be employed in severe cases. Evidence indicates that receiving the smallpox vaccine in the past could provide protection against the monkeypox virus and potentially enhance the clinical symptoms during an infection6.
In conclusion, oral and oropharyngeal manifestations of MPXV in this outbreak period can become more prevalent, which is why oropharyngeal examination should be part of the clinical assessment for patients with monkeypox. Nonetheless, every at-risk individual exhibiting oral and oropharyngeal symptoms suggestive of STIs ought to get a test for MPXV infection.
Conflito de Interesses
Os autores declaram que não têm qualquer conflito de interesse relativo a este artigo.
Confidencialidade dos dados
Os autores declaram que seguiram os protocolos do seu trabalho na publicação dos dados de pacientes.
Proteção de pessoas e animais
Os autores declaram que os procedimentos seguidos estão de acordo com os regulamentos estabelecidos pelos diretores da Comissão para Investigação Clínica e Ética e de acordo com a Declaração de Helsínquia da Associação Médica Mundial.
Política de privacidade, consentimento informado e Autorização do Comité de Ética
Os autores declaram que têm o consentimento por escrito para o uso de fotografias dos pacientes neste artigo.