Introduction
Chronic otitis media with cholesteatoma (COM-wC) is defined as a “mass formed by keratinizing squamous epithelium in the middle ear subepithelial connective tissue, with progressive accumulation of keratin debris with/without surrounding inflammatory reaction”1 which can cause significant impairment, if left untreated.
Due to its local inflammatory and destructive characteristics, it can lead to complications such as facial nerve paralysis, temporal bone/intracranial infections, and erosion of the ossicular chain and otic capsule affecting hearing and vestibular function. 2
To this day, surgery remains the mainstay of treatment. The main goals are complete eradication of the disease, maintenance of an epithelialized, self-cleaning ear and preservation of hearing. (2-4 However, there is no consensus about the best surgical technique from the innumerous described and surgeons still struggle when it comes to decide the right approach for each individual case.
Many factors come into play regarding this decision-making process, those include extension of disease, anatomical factors conditioning accessibility during surgery, comorbidities, age, socioeconomic condition, collaboration of the patient and surgeon expertise. 2,3,5,6
Surgical procedures can be largely categorized by the preservation or not of the posterior bony external auditory canal (EAC) wall, as canal wall up (CWU) or canal wall down (CWD) mastoidectomies and regarding the type of ossicular reconstruction including which interposition material used. 2,7
In this study, we performed a 10-year retrospective review of our experience regarding the surgical management of COM-wC in a peripheral hospital, comparing preoperative and postoperative parameters and the functional outcomes of different surgical approaches.
Material and Methods
We performed a 10-year retrospective review of digitized institutional medical records from patients undergoing surgical intervention for COM-wC at ULSTS hospital, Portugal, between 1 January 2012 and 31 December 2022.
Inclusion criteria comprised all patients submitted to surgery for treatment of COM-wC during the mentioned period. Exclusion criteria were applied to patients with a follow-up period of less than one year and patients in which relevant data were not available in the hospital computer system, such as audiograms and radiological results.
All patients underwent an audiometric and temporal bone CT scan evaluation prior to surgery. After intervention, clinical surveillance was carried out regularly with otoscopy examinations and an initial audiometry was performed between 3 to 6 months in all patients. Additionally, in cases of wall-up procedures, a high-resolution CT scan of the temporal bone was routinely performed after 2 years. Whenever a non-specific soft tissue density was found an additional diffusion-weighted MRI was requested.
Preoperative data was collected regarding age, sex, time of follow-up before surgery, previous otologic interventions, mastoid pneumatization from CT scans, contralateral tympanogram (as a proxy for middle ear ventilation) and audiometric results including the air-bone (A-B) gap and pure tone average (PTA) for air conduction at 500, 1000, 2000 & 4000 Hz performed within the 6 months before surgery.
At the time of surgery, the extension of cholesteatoma was classified according to the STAM classification system8 in which the middle ear and mastoid space are divided into four sites: tympanic cavity (T), attic (A), mastoid (M) and the difficult access sites, supratubal recess (S1) and the sinus tympani (S2). Other intraoperative assessments such as otoscopic findings, dehiscence of the facial or lateral semicircular canals and erosion of the tegmen tympani were also registered.
Surgeries mainly consisted in the combination of tympanoplasties and mastoidectomies, wall up or down. Decisions regarding preservation of the posterior wall of the EAC were mostly made intraoperatively. The wall down variant was the preferred method in cases with extensive cholesteatoma, poor access to certain areas of the mastoid, small mastoid volumes and relapses.
Additionally, atticotomies were also performed in cases of small attic cholesteatomas in which only a limited portion of the wall of the EAC was resected by drilling the scutum to the limits of the cholesteatoma sac.
Ossicular reconstruction was made in most cases in which there was loss of the ossicular chain integrity due to erosion. The materials used included tragus cartilage, autologous ear ossicle grafts and alloplastic prothesis such as partial ossicular replacement prosthesis (PORPs) and total ossicular replacement prosthesis (TORPs) which depended on the type of defect encountered and the gap to restore. For the classification of tympanoplasties we used the one described by Portmann.9
Postoperative data was analyzed regarding hearing outcomes, and complications such as recidivism, intermittent otorrhea, extrusion of prothesis and other significant events during the follow-up period.
Statistical analyses were performed using the IBM SPSS Statistics v29 software. Chi-squared test was performed for analysis of associations between two categorical variables and the independent sample t-tests to compare means or proportions of two independent groups. p < 0.05 was considered significant.
Results
We included 94 patients with a total of 97 cases of surgery performed by nine different specialists over a period of 10 years. 54 were males and 43 females. There was an equal distribution between sides of the affected ear and three patients had bilateral disease.
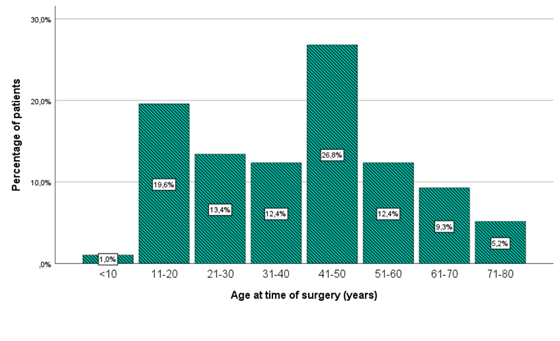
The mean age at the time of surgery was 39.7 years. Of note, 26.8 % of patients were in the age group 41-50 years with another peak seen in the group 11-20 years (19.6%) (chart 1).
On average, patients were followed in ENT consult due to otologic complaints for 21.5 months before surgery. Most cases were classified as primary acquired cholesteatomas (94.8%, n=92) associated with tympanic retraction pockets or attic tunnels, however, in 5 distinctive cases (5.2%), a previous assertive history of chronic tympanic membrane perforations (not associated with other tympanic membrane alterations) were reported, causing them to be classified as secondary acquired cholesteatomas. There were no cases of congenital cholesteatomas.
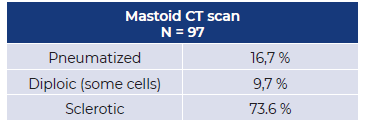
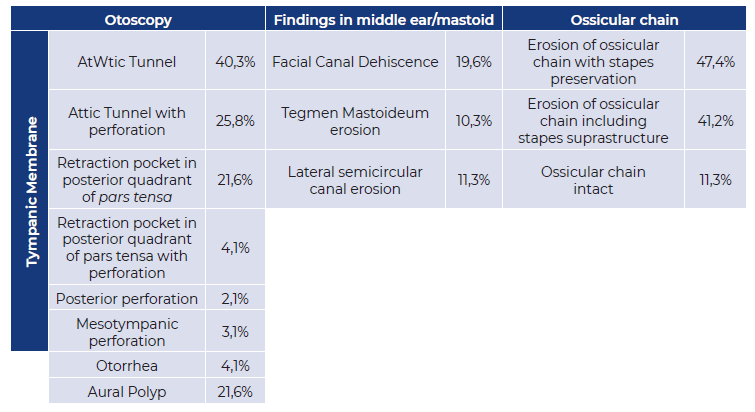
From analysis of preoperative exams, CT scans revealed a majority of patients with a sclerotic mastoid in the affected ear (73,6%) and contralateral tympanograms revealed a slight predominance of type C or B results, (51,7% of tested ears). (table 1and2)
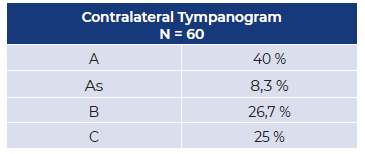
Regarding intra-operative findings (table 3), otoscopy revealed that attic tunnels (66,1% of patients) and retraction pockets of the posterior pars tensa (25,7%), with or without perforations, were the most common findings. Aural polyps were reported in 21,6% of cases and otorrhea was only seen in a small percentage of 4,1% of patients.
After entering the middle ear/mastoid space, findings were generally congruent with those of CT. Surgeons observed facial canal dehiscence in 19,6% of cases and signs of erosion at the level of the tegmen tympani and lateral semicircular canals in 10,3% and 11,3% of patients, respectively.
The integrity of the ossicular chain was also assessed. Signs of erosion were encountered in 86 patients (88,6%). In 41,2% of total cases, the stapes suprastructure was affected.
Intraoperative localization of cholesteatoma (chart 2), according to the STAM classification system, revealed that the most affected site was the attic (91.9%), followed by mastoid (65%), tympanic cavity (58,8%), supratubal recess (14,5 %) and the sinus tympani (2.1%). However, cholesteatomas extending only to a single site were observed in just 26.8% of cases. The majority of cases extended through multiple sites (73.2%). The combination of attic, mastoid and tympanic cavity was the most common, corresponding to 30.9% of total cases. There was no significant difference between the mean follow-up time before surgery between the groups with cholesteatoma extending into one or multiple sites (p=0.32).
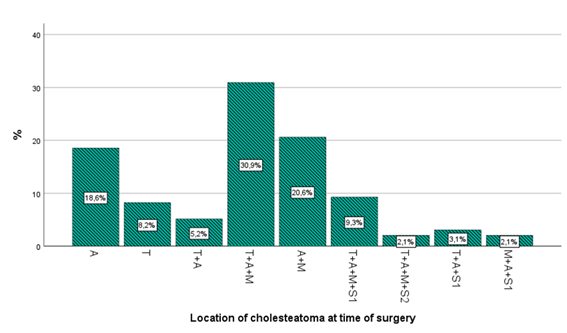
Chart 2 Location of cholesteatoma assessed during surgery. T- tympanic cavity; A - attic; M - mastoid; S1- supratubal recess; S2 - sinus tympani.
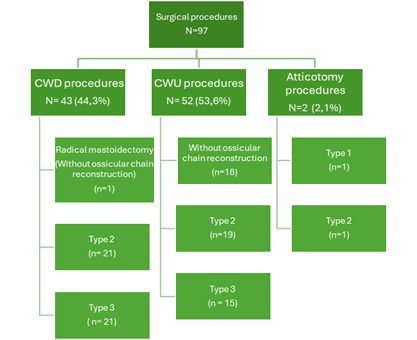
Overall, 43 patients underwent a CWD procedure (44,3%), 52 underwent a CWU mastoidectomy (53,6%) and in the remaining two, an aticotomy was performed. Ossicular chain reconstruction was attempted as a single staged surgery in 76 cases, of which 41 (53,2%) were type 2 tympanoplasties and 36 (46,8%) were type 3 (chart 3). The materials used for ossicular chain reconstruction are summarized in table 4.
Table 4 Materials used for ossicular reconstruction
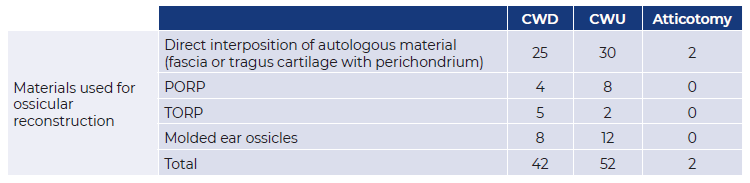
Note: All TORPs and PORPs were placed in conjunction with autologous material.
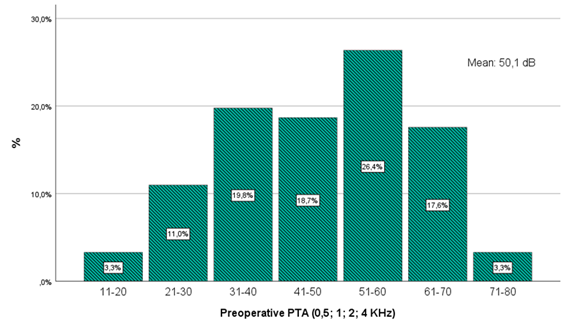
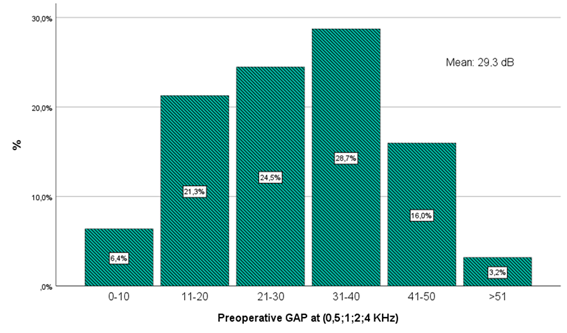
The overall average pre-operative air-bone (A-B) gap was 29,3 dB, and the average PTA was 50,1dB (chart 4and5).
There was no significant difference between patients which had cholesteatoma in only one site or multiple sites, regarding pre-operative mean PTA or A-B gap, (p=0.684 and p=0.717, respectively). However, a significant difference was seen regarding mean PTA between patients which showed signs of ossicular erosion with stapes preservation (mean 47,8 dB ± 16,8) and those in which the stapes suprastructure was affected (mean 55,3 ± 15,9), p=0.038.
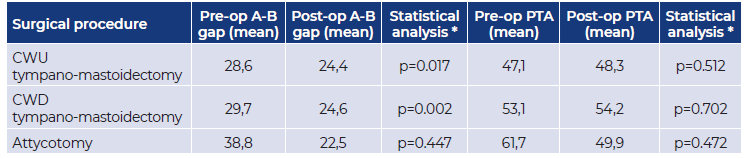
Considering hearing outcomes (table 5), in the CWU group, the average pre-operative A-B gap was 28.6 dB, and the average PTA was 47.1 dB, with an average post-operative reduction in gap of 4.2 dB and PTA worsening of 1.2 db. For the CWD group, the average pre-operative A-B gap was 29.7 dB, and the average PTA was 53.1 dB, with an average post-operative reduction in gap of 5.1 dB and PTA worsening of 1.1 dB.
From the small sample group of atticotomies (n=2), average pre-operative A-B gap was 38.8 dB, and the average PTA was 61.7 dB. After surgery, there was a marked reduction in both A-B gap (16.3 dB) and PTA (11.8 dB), however, the small sample size prevents any valid assumptions from being drawn.
Hearing outcomes were not statistically different between CWU and CWD groups regarding PTA (p=0.785) and A-B gap (p=0.722). Additionally, we concluded that there was also no significant difference when comparing type 2 and type 3 tympanoplasties: PTA (p= 0,769) and A-B gap (p= 0,373).
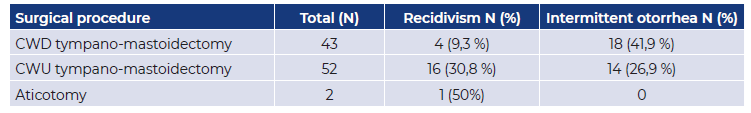
The overall relapse rate was 21.6%, (n=21). Distribution of those cases were as follows: 16 in CWU group, 4 in CWD group and 1 in the atticotomy group (table 6).
From the total relapse cases, 17 (81%) corresponded to cholesteatomas which extended through more than one site and in 9 cases (42,9 %) there was cholesteatoma visible in a difficult access site (S1 or S2). Of the total number of relapses,15 (71.4%) underwent a second surgical procedure, on average 28 months after the first.
After statistical analysis we concluded that recidivism was significantly dependent on the type of mastoidectomy performed (p=0.02) and was significantly higher in the wall up group compared to wall down (p=0.01). Infection status of the cavity after surgery was also analyzed, intermittent otorrhea was most frequently seen in CWD patients 41,9 % compared to 26,9% of CWU, (p=0.125).
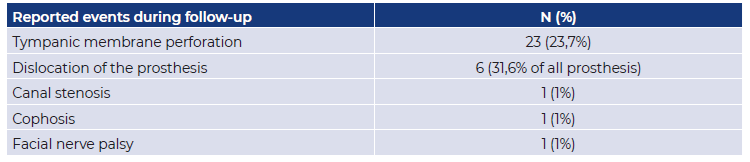
Other postoperative complications included: tympanic membrane perforation (n=23, 23,7%); dislocation/extrusion of prosthesis, (n=6, 31,6% of all prosthesis placed); canal stenosis (n=1,1%), cophosis (n=1, 1%) and facial nerve palsy (n=1, 1%). (table 7).
In the single case of facial nerve palsy, a grade II House-Brackmann paralysis was seen immediately after surgery and electromyography revealed a neuropraxia lesion which had likely occurred during unintentional manipulation of the facial nerve. The patient was treated with a small course of corticosteroids followed by regular physiotherapy and slowly improved to a complete resolution in 5 months. Nevertheless, two patients presented with facial nerve impairment preoperatively. Among them one presented with grade III and the other with grade V House-Brackman paralysis. Both required careful resection of the epidermoid tissue from the dehiscent facial canal and placement of temporal fascia over the defect. The grade V patient slowly improved facial function to a grade II after one year and a half of physiotherapy but in this case, a dead ear was seen after surgery, probably due to the advanced stage of the disease which had created a labyrinthine fistula. The grade III case had a more rapid improvement to a complete restoration of function, within two months after surgery, while also benefiting from physiotherapy.
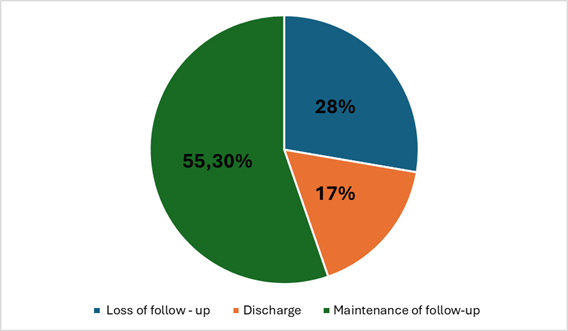
At the time of the review of medical records (chart 6), 16 patients (17% of total number of patients) were discharged from ENT consulting with stable ears. In that group we registered an average follow-up period of 2.4 years with 1 year as the minimum follow-up required. Of those, 68% were from CWU group, 25% from CWD and 7% corresponded to aticotomies. On the other hand, we registered a loss of follow-up due to unknown causes in a relevant proportion of 27.7% of patients. The remaining 55,3% of patients submitted to surgery during the 10-year timeframe covered by this study had maintained a regular follow-up at the time of writing.
Discussion
Surgery remains the mainstay of treatment for COM-wC. Literature reviews on this subject reveal a panoply of different surgical approaches which have evolved from radical mastoidectomies to the more preserving and reconstructive tympano-mastoidectomies. Up to date, there is still no consensus about the best possible intervention for each individual case.
However, controversy surrounding cholesteatoma goes beyond the debate around its surgical management. In fact, there is still a debate about the pathophysiological processes that give rise to it and innumerous theories have been developed. The most widely accepted for primary acquired cholesteatoma (the main bulk of cases encountered in this review) is the retraction theory, in which a slow ingrowth of squamous epithelium enters the middle ear from a retraction pocket of the tympanic membrane due to a dysregulation in middle ear pressure. (2 As for secondary acquired cholesteatomas, literature supports that they may develop due to migration of keratin epithelium through a tympanic membrane perforation or temporal bone fracture. 2
In this series, regarding etiopathogenesis, it became clear the chronicity of this disease, as the mean time of follow-up due to otologic complaints before surgery was 21,5 months. Additionally, from pre-operative assessments it is important to note that most patients had sclerotic mastoids (73,6%), type C or B contralateral tympanograms (51.7% of cases), and otoscopy mostly revealed attic tunnels (66.1%) and retractions pockets of the posterior pars tensa (25.7 %), all findings supporting a preexisting impairment in middle ear ventilation.
Preoperative audiometry revealed no significant relationship between the degree of hearing loss and the extent of the disease classified by the STAM system, but rather with the erosion of the ossicular chain, more specifically whether the supra-structure of the stapes was affected or not. There are multiple complex mechanisms that come into play regarding the cholesteatoma effect on hearing. While cholesteatomas could impair hearing function due to changes in middle ear resonance and limitation of the vibratory capacity of the ossicular chain or tympanic membrane 10, it may also act as a transmission bridge of acoustic energy, resulting in narrowed air-bone gaps. (11
The association between the degree of hearing loss and ossicular chain erosion in cases of COM-wC remains controversial. While some reports suggest that hearing loss is not a good predictor of ossicular chain status 11,12, a different study 10 and our review describe a correlation.
There are different features generally attributable to each type of surgery. CWD mastoidectomies have the advantage of better visibility and access to more difficult sites, providing a more consistent complete removal of the disease. However, they are associated with higher occurrences of non-self-cleaning cavities which may require regular follow-up visits, water restrictions and special molds for hearing aids. Those who favor CWU approaches argue that complete eradication of the disease can be achieved in most cases with this technique, and patients will benefit from a better quality of life during follow-up due to a self-cleaning ear.
In our practice, a general preference was given to CWU techniques in order to not create an open cavity which could significantly affect the quality of life of patients. Additionally, for CWU procedures we did not feel the need to perform a routine second-look surgery as the imaging techniques available for follow-up, namely diffusion weighted magnetic resonance imaging, have proven to be both sensitive and specific for detecting recidivism, and, therefore, are reasonable alternatives. (13,14
The decision-making process for the surgical technique was made preoperatively in some instances including relapses (which were all managed with CWD techniques). However, in most cases, it was made intraoperatively considering anatomic factors, extension of the disease and surgeon expertise. In that regard, it was common for a surgery to start as a CWU procedure, and then be converted to CWD whenever deemed necessary.
In our series, the most frequent reasons for performing a CWD tympano-mastoidectomy were an extensive disease present in difficult access areas (S1 and S2), recidivism, erosion of the posterior external auditory canal or lateral semicircular canal, low volume mastoids, presence of cholesteatoma in an only hearing ear, high surgical risk and a low likelihood of adequate follow-up.
Furthermore, in the same surgical time, ossicular reconstruction was carried out using a myriad of different techniques and materials, which have been previously described but were not subjected to a comparative analysis given the low number of cases we had for each different type.
When comparing hearing outcomes from CWU and CWD approaches we also found contrasting reports in literature. While most studies fail to find any significant difference between the two approaches. (15-17 some reported better hearing results with CWU procedures 4,18 while the opposite has also been described 19. Our results demonstrated a minimal worsening of hearing in both groups after surgery and support the notion that the preservation or not of the posterior canal wall has no significant influence on hearing results, as innumerous other factors may have a more prominent role in that respect, such as the state of the ossicular chain and the different types of ossicular reconstructions performed.
Regarding recidivism, these cases were significantly lower in the CWD group. Our results are in line with many convincing publications which showed that a wall down technique is the safest choice to prevent the need for a second surgery 4,20-22. The most likely explanation for this is that relapses may originate from residual epidermic tissue left in difficult access sites for a wall up approach. In that regard it is interesting to note that in 42,9 % of our relapses there was cholesteatoma visible in the supratubal recess or sinus tympani. On this detail, it is worth mentioning otovideoendoscopy as a breaking technology which has proven to reduce the incidence of residual cholesteatomas by enabling identification of lesions in difficult access areas under otomicroscopy. (23 This technology, which can be an added value, was not available in our institution during the reviewed surgeries.
On the other hand, intermittent otorrhea affecting quality of life was more commonly seen in the CWD group, probably due to the increased risk that an exposed open cavity has of becoming infected if the required preventive measures are not followed.
Regarding follow-up, it’s important to note that a significantly higher discharge rate was seen in the CWU group, as expected, given the main advantage of a self-cleaning ear. We also point out the seemingly large proportion of patients who had a loss of follow-up. This occurrence may have a significant negative impact on the long-term prognosis for these patients. Although not completely understood, loss of follow-up in our cohort can be in part explained by the constraints of medical care during the COVID-19 pandemic and the significant proportion of patients who have changed their residence, including emigrants, commonly reported in our population.
Conclusion
Etiopathogenesis and surgical management of cholesteatoma are still highly debated topics. Both canal wall up and down approaches have their own advantages and risks. The decision-making process should be a highly individualized one, considering clinical, anatomic, and social factors as well as the surgeon expertise. Although most cholesteatomas which are diagnosed in earlier phases can be safely managed with CWU surgeries, in more advanced cases a CWD technique can be mandatory. This study shows no significant differences in hearing results for both techniques while it favors CWD surgeries for a safer eradication of the disease.
Conflict of Interests
The authors declare that they have no conflict of interest regarding this article.
Data Confidentiality
The authors declare that they followed the protocols of their work in publishing patient data.
Human and animal protection
The authors declare that the procedures followed are in accordance with the regulations established by the directors of the Commission for Clinical Research and Ethics and in accordance with the Declaration of Helsinki of the World Medical Association.
Privacy policy, informed consent and Ethics committee authorization
The authors declare that they have obtained signed consent from the participants and that they have local ethical approval to carry out this work.