Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.21 no.5 Lisboa out. 2014
https://doi.org/10.1016/j.jpg.2014.03.003
ORIGINAL ARTICLE
Endoscopic management of digestive leaks with the Over-The-Scope Clip: A retrospective study
Resolução de fugas digestivas com Over-The-Scope Clip: análise retrospectiva
Tito Correiaa,*, Pedro Amaroa, Ana Oliveiraa, Alexandra Fernandesa, Diogo Branquinhoa, Ana Nunesb, Francisco Portelaa, Carlos Sofiaa
a Gastroenterology Department, Centro Hospitalar e Universitário de Coimbra, Coimbra, Portugal
b Gastroenterology Department, Hospital Garcia de Horta, Almada, Portugal
*Corresponding author
ABSTRACT
Introduction: The Over-The-Scope Clip (OTSC®) is a device with promising applications in endoscopic closure of perforations/dehiscence/fistulas, endoscopic hemostasis and NOTES.
Aims: To evaluate the clinical effectiveness and safety of OTSC.
Methods: Between September 2011 and September 2013, 6 consecutive patients underwent OTSC placement by two experienced endoscopists. In three patients OTSC was used in the closure of surgical dehiscences, both in upper digestive tract (after esofagojejunostomy and gastric sleeve) and in lower digestive tract (blind loop dehiscence after colorectal anastomosis). Two patients had esophageal fistulas with several weeks duration (one to the bronchial tree and other to the pleura). Furthermore, OTSC was used to close an iatrogenic perforation following colonic polipectomy.
Results: All procedures experienced technically immediate success and there were no complications related to the placement of the OTSC (1 clip). It was well tolerated and patients were hospitalized on average 15 days (5-53 days). However, during follow-up (mean = 12.4; 5-22 months) permanent closure of chronic esophageal-bronchial fistula could not be achieved in one patient.
Conclusion: In our experience, OTSC shows efficacy in solving gastrointestinal leaks.
Keywords: Over-The-Scope clip; Gastrointestinal leaks; Fistula; Perforation
RESUMO
Introdução: O endoclip Over-The-Scope (OTSC) é um acessório com possíveis aplicações no encerramento de perfurações/deiscências/fístulas, hemostase endoscópica e em NOTES.
Objectivo: Avaliar a eficácia clínica e segurança do OTSC.
Métodos: Entre Setembro de 2011 e Setembro de 2013, seis pacientes consecutivos foram submetidos à colocação OTSC por dois endoscopistas com experiência em modelos animais. Em três pacientes o OTSC foi utilizado no encerramento de deiscências cirúrgicas, tanto no tracto digestivo superior (após esofagojejunostomia e sleeve gástrico) como no tracto digestivo inferior (deiscência de ansa cega após anastomose colorretal). Dois pacientes apresentaram fístulas esofágicas com duração de várias semanas (um para a árvore brônquica e outro para a pleura) que dificultou a colocação do OTSC. O OTSC foi usado, igualmente, para fechar uma perfuração iatrogénica após polipectomia do cólon.
Resultados: Todos os procedimentos obtiveram sucesso técnico imediato e não se observaram complicações relacionadas com a colocação do OTSC (1 clip). O procedimento foi bem tolerado e os pacientes permaneceram internados, em média, 15 dias (553 dias). No entanto, durante o acompanhamento (média=12,4; 5-22 meses) o encerramento definitivo de fístula esôfago-brônquica crônica não foi possível em um dos pacientes.
Conclusão: O OTSC provou a sua aplicabilidade na resolução de soluções de continuidade gastrointestinais.
Palavras-chave: Over-The-Scope clip; Deiscência gastrointestinal; Fístula; Perforação
Introduction
Post-surgical complications such as fistula and anastomotic leaks are conventionally submitted to surgical repair (open, laparoscopic or external drainage). However, surgical reintervention has a significant morbidity and mortality, prolongs hospital stay and increases the costs.1 Several endoscopic techniques have been described for closure of gastrointestinal leaks (perforations, leaks, and fistulas) by using various devices and methods such as clipping with multiple metallic endoclips,2-4 ligating with endoloops and rubber bands,5 fibrin glue sealing,6 prolene mesh plugging and application of cyanoacrylate,7 clips and endoloop together by using a double channel endoscope.8 In 2007, Kirschniak et al. described the first cases of small mural leaks closure with a new endoclip system, the over-the-scope clip- OTSC® (Ovesco Endoscopy, Tuebingen, Germany).9 This endoclip is made of super-elastic shape memory nitinol alloy (MRI-safe material), which resumes its former unbent shape after the clip is released and exerts a more sturdy closure compared to conventional endoclips due to its capacity to grasp more visceral tissue and apply a greater compressive force. The system consists of a clip that is preloaded on a transparent applicator cap mounted on the endoscope tip, which can be released by pulling a taut wire threaded through the working channel to the hand-wheel of the scope, similar to band-ligation systems. Recently, case series and reviews have been published describing its success in treatment of gastrointestinal bleeding, fistula, and perforations.10-18
The present retrospective study, performed within the endoscopy unit of a tertiary referral center, evaluated the clinical effectiveness and safety of the OTSC system in the management of non-malignant gastrointestinal tract wall leaks.
Patients and procedures
Clinical cases of six consecutive patients that underwent OTSC placement between September 2011 and September 2013 were reviewed. Patient characteristics are summarized in Table 1. The OTSC system was mounted onto the tip of a gastroscope (Olympus GIF-1T Q160; diameter of 9.8 mm; working channel of 2.8 mm; Olympus, Tokyo, Japan) in the same manner as a band ligation device. Traumatic version (t type) of OTSC, medium sized caps twin type graspers (OTSC Twin Grasper® Ovesco Endoscopy, Tuebingen, Germany) and anchor (OTSC Anchor®, Ovesco Endoscopy GmbH, Tuebingen, Germany) were used. Two endoscopists with previous experience in animal models performed the application of the device. All procedures took place under conscious sedation with intravenous midazolam or deep sedation with intravenous propofol.
All procedures were performed by two advanced endoscopists with experience of OTSC placement in animal models.
To all patients had been previously explained the therapeutic procedure and all signed the respective informed consent.
Results
A systematic approach of the data, including patient procedure details, technical and clinical outcomes, is represented in Table 1.
Patient 1: A 71-year-old man underwent total gastrectomy and Roux-en-Y esofagojejunostomy for gastric adenocarcinoma. A blind loop jejunal dehiscence and complex fistula occurred 10 days later. After a couple of weeks under antibiotherapy and external drainage, he suddenly developed dyspnea and hemoptysis. New CT and barium transit described a transdiaphragmatic tract linking the abdominal collections to a lung abscess with fistula to the bronchial tree. Despite broad-spectrum antibiotics and external drainage, there was progressive clinical deterioration due to severe septic shock, not allowing surgical approach. Endoscopy was then performed whichrevealed a 12 mm dehiscence of the Roux-en-Y blind loop closure. As it has not been possible to aspirate the fistula hole into the device it was decided to suck the entire circumference of normal mucosa upstream the orifice, creating a new closure of the loop by the placement of the OTSC. The immediate clinical response was extremely favorable, as evidenced by the swift recovery from the septic state and resolution of the suppurated abdominal fistula to the bronchial tree. The patient remains asymptomatic after 17 months of follow up.19
Patient 2: An 84-year-old man underwent anterior rectal resection for rectal cancer, with protective ileostomy and colorectal anastomosis. Two weeks after the surgery, an anastomotic dehiscence was diagnosed by CT, which identified a pre-sacral abscess (12 cm × 6 cm), close to surgical anastomosis, as well as air in the retroperitoneum.
After pelvic drainage and antibiotitherapy there was clinical improvement. However, soon after, he developed pelvic pain and fever, and CT and barium transit confirmed per- sistence of colorectal anastomosis dehiscence and pelvic abscess. Endoscopy, revealed a fistulous orifice in the colon blind loop (Fig. 1a). Leak margins were easily grasped with the OTSC anchor and invaginated into the applicator cap and the wall was closured by a OTSC with occlusion of the fistula lumen (Fig. 1b). The patient fully recovered and was discharged after seven days.

Patient 3: A 36-year-old woman underwent laparoscopic sleeve gastrectomy for obesity. She presented on the fifteenth postoperative day with abdominal pain, fever and vomiting. CT revealed a postoperative leak in the proximal third of the gastric sleeve. Initially, a new laparoscopic approach was performed, with abdominal abscess drainage, fistula rafia and abdominal drains were placed. Symptoms persisted and an esophagogastroduodenoscopy confirmed the maintenance of the gastric fistula. Subsequent placement of fully covered esophageal stent (Poliflex®, 12 cm long, 20 mm diameter) was possible and assisted to clinical improvement. However, shortly thereafter, the patient developed obstructive symptoms and maintained purulent material by surgical drains. Endoscopically, prior esophageal stent was removed (medium part was damaged) upkeeping the gastric fistula and a OTSC was deployed. The patient presented clinical (purulent drainage stopped) and imagiological improvement (no contrast leak). At follow-up, the patient continued to tolerate oral intake, maintaining a stable weight, without abdominal pain or fever.
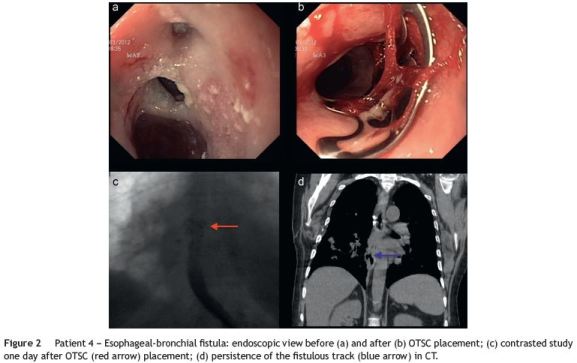
Patient 4: A 66-year-old woman underwent surgical esophogorraphy after spontaneous rupture of the esophagus. Three months later she developed symptoms of esophago-bronchial fistula, confirmed by endoscopy and barium transit. Medical and endoscopic treatments were performed with placement of three partially covered self-expandable stents, which presented distal migration. The patient showed clinical improvement with resolution of fistula in the barium transit. Six months after she presented with fever and a respiratory infection was diagnosed. Esophagogastroscopy was performed and two small holes compatible with esophageal-bronchial fistula were identified in the mid esophagus. She was referred to our department and an OTSC was deployed after traction with an anchor with apparent closure of the fistulous orifice, confirmed by contrast study (Fig. 2 a-c). A few days after, the patient developed a respiratory exacerbation and it was verified the absence of the esophageal OTSC. The persistence of the fistulous track (Fig. 2d) led to a new surgical approach, also without success.
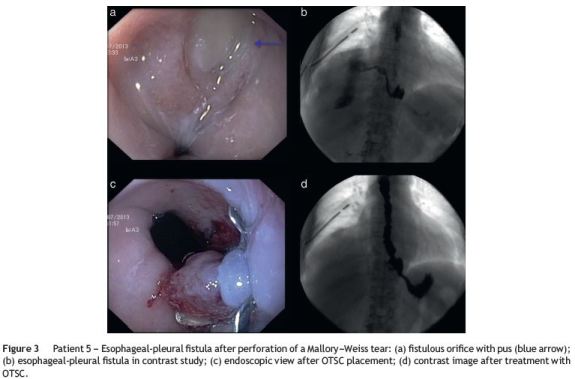
Patient 5: A 71-year-old women presented with hematemesis due to Mallory-Weiss tear. A few days later she developed sepsis consequent to respiratory infection, with right pleural effusion. Placement of chest drain identified purulent liquid. After resumption of oral feeding, it was observed food content in pleural drainage, confirmed by contrast examination with identification of fistulous track with about 5 cm from the distal esophagus to the right pleural space (Fig. 3a and b). Persistence of pleural effusion led to endoscopic attempt to closure the fistulous orifice using endoclip OTS with anchor (Fig. 3c). During the procedure methylene blue was instilled in the lumen, and no drainage by the chest tube was identified. New contrasted study took place 15 days after OTSC placement, which showed no leak- age of the contrast product (Fig. 3d). Clinically, the patient resumed oral feeding, without evidence of recurrence of the fistula or other complications.
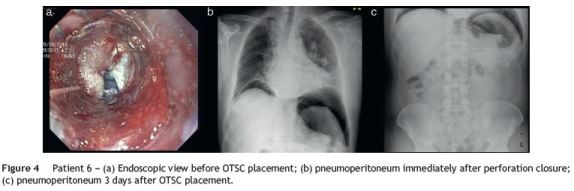
Patient 6: A 63-year-old man previously healthy under- went elective colonoscopy in our department to perform polypectomy. At 45 cm from the anal margin, there was a large and bulky sessile polyp, with a multilobulated surface, measuring about 5 cm in diameter. After mucosal elevation with diluted epinephrine and methylene blue, the polyp was removed with a snare. Upon verification of the scar, there was a perforation of 10 mm (Fig. 4b). Using a therapeutic gastroscope, the colic perforation was closed using an OTSC, with apparent success. The residual polypoid tissue was also removed with a snare. The patient was admitted under broad-spectrum antibiotics and no oral intake. He showed positive clinical, analytical and radiological evolution (Fig. 4c), and three days after the event liquid diet was introduced. He was discharged asymptomatic, seven days after admission.
Discussion
Spontaneous or iatrogenic perforation of the gastrointestinal tract wall may cause a variety of clinical settings, ranging from an asymptomatic course up to severe (and even lethal) complications, requiring prompt closure and control of extraluminal fluid collections and sepsis. Anastomotic leaks are probably the most dreaded complications of intestinal surgery, with mortality rate often reported to be up to 10-15%.20 The incidence of intestinal anastomotic leaks ranges from 1 to 19% depending on the location of the anastomosis. However, small bowel anastomosis tends to be associated with a lower risk of anastomotic disruption than large bowel anastomosis, particularly when compared to the distal rectum or anal canal.20 Anastomotic leakages following esophagectomy occur in about 10% of cases. Anterior rectal resections lead to anastomotic leakages in 9.6% if a diverting ileostomy is used, with even higher rates if an ileostomy is omitted.20
In endoscopic procedures, the risk of perforation depends essentially on the purpose of the exam. Perforation occur by accident in 0.06-0.12% of diagnostic colonoscopies.21,22 However, reported perforation rates are 0.3-0.5% after endoscopic mucosal resection and 4-10% in endoscopic sub- mucosal dissection, and hence substantially higher than conventional endoscopic procedures.23
Until recently, iatrogenic or surgical leaks were surgically managed, using a diversity of procedures (proximal diversion, omentoplasty) combined with percutaneous drainage and intravenous antibiotics. Nonetheless, direct surgical repair is difficult, hazardous and often not feasible. Recent advances in endoscopic techniques have improved the treatment of this severe event using endoclips and self-explandable stents. The choice to treat a perforation endoscopically is made on the basis of the cause, location, duration and severity of the perforation, patients age and general health and, finally, on the endoscopist and surgeons experience. Furthermore, endoscopic treatment allows shorter hospitalization, a negligible morbidity and mortality, prompt resumption of an oral diet and reduced costs.24
Since 1993 several series of endoscopic closure using endoclips have been described in literature, involving the esophagus, stomach, duodenum-jejunum and colon-rectum.2-7 Conventional endoclips (metallic double-pronged clips introduced through the operative channel of the scope) are used for the management of bleeding and perforations. However, they have limitations, namely restricted opening distance between the jaws and low closure force, which hamper its use in the presence of scarred and hardened tissue or inflammatory mucosa. It is common experience that a high number of clips are necessary to treat gastrointestinal leaks. The use of self-expandable stents is effective for sealing and healing chronic gastrointestinal dehiscence. Yet, removal of partially covered stents may be difficult due to ingrowth at uncovered ends with the risk of mucosal tears, whereas fully covered stents show a migration rate up to 50% and often require replacement.25 Although the success rate is satisfactory, healing can sometimes take months to occur, and many patients experience a slew of added morbidities while they wait: alkaline and acid reflux, epigastric pain, downright intolerance.
The choice of OTSC technique in the cases presented was based not only on the nature of the injury but also because of the unique characteristics of the clip itself. Indeed, this new approach has proved to be useful in similar situations, in which alternative options were lacking.11,12,15-17,26 Proper application of OTSC requires perfect coaptation with the injury and aspiration of tissues into the cap so that they can be captured on release of the clip. Alternatively, the tissues can be pulled using the devices handled through the working channel and marketed specifically for this purpose (OTSC Twin Grasper® or OTSC Anchor®). Made of highly elastic nitinol, biocompatible and easily delivered, this new device is remarkable and its full potential to help endoscopists and surgeons get out of a jam and has yet to be realized. The success described in the closure of acute perforations is explained by the fact that margins of the defect are commonly flexible and elastic to allow approximation by simply sucking them in the cup or, in larger leaks, by grasping them, avoiding laceration.9 On the other hand, dificulties may arise in the treatment of chronic leaks, which are surrounded by hardened and inelastic tissues unfit to be approached. Indeed, Kirschniak15 and Albert26 have reported that the success rate of OTSC is inversely proportional to the time from diagnosis of the clinical leakage to the application of the clip, ranging from 100% after 1 week to less than 60% with increasing time.
Our series demonstrates the capacities and limitations of OTSC system. Although OTSC application was technically successful in all patients, we experienced one patient with fistula recurrence within a few days (patient 4). However, when referred to our department, this patient had a chronic esophago-bronchial fistula, with two small holes identified in the middle esophagus. The attempt to place the OTS clip was hampered by the presence of fibrotic tissue, inelastic, and unfit to be sucked to the cup. Despite immediate clinical success with apparent fistula closure after the OTSC release (clip was present, but with no contrast leak), ten days after the patient presented with recurrent respiratory symptoms, no visualization of the clip and fistula maintenance. This long-term clinical failure is probably explainable by the small amount of tissue between the OTSC jaws, consequence of tissue fibrosis. In patient 5, while there was esophageal-pleural fistula, better margins traction was achieved allowing the correct release of the OTSC and con- sequent closure of fistula. Closure of the blind jejunal loop dehiscence was performed by a particular technique not yet described. Due to inability to directly access the fistulous orifice, we held circumferential aspiration of healthy tissue (without traction) located about 2 cm upstream of the orifice, with subsequent release of the OTSC.19 The aim of this approach was to create an endoscopic closure of the loop, using healthy tissue proximal to dehiscence and thereby excluding it from luminal contact. The possibility of complete luminal closure used deliberately in this case has been described as an adverse effect in two cases of a series published in 2012.18 In two other cases, success was achieved by releasing the clip on the surgical leak, with consequent clinical improvement and completely resolution of the wall defect. In the last patient OTSC placement was achieved in an iatrogenic perforation of the colon in the context of a mucosal resection, thus avoiding surgical approach. The five successfully treated patients had fast recovery and started oral ingestion with no further treatment.
In our series there were no immediate or late complications associated with OTSC placement, but is clear that there was a learning curve when using this device and associated accessories. Some severe adverse events are described in the literature, such as complete lumen closure secondary to clip misplacement.18 Other possible complications include mucosal damage caused by the teeth of the OTSC protruding out of the hood top during insertion. Therefore, special care should be taken when the OTSC is inserted into physiologically narrow sites, such as the esophageal entrance, pyloric or anal ring.27
Although it has not been used so far in our center, OTSC has been described to be effective as hemostatic therapy. It may be of particular benefit in some cases of ulcer hemorrhage refractory to conventional therapy and in surgical anastomotic bleeding lesions.27
In conclusion, OTSC can be useful in the management of gastrointestinal leaks. OTSC has several advantages over through-the-scope clips, allowing the closure of orifices of larger size using a single clip. The cost of this clip is not negligible, though earlier hospital discharge is expected when compared to surgery. Management of small iatrogenic or spontaneous GI perforations or leaks should involve multidisciplinary collaboration including surgeons and endoscopists. In our opinion, endoscopic treatment should be considered earlier in course of the disease, thus trying to prevent tissue fibrosis which hampers this approach.
References
1. Schecter WP, Hirshberg A, Chang DS, Harris HW, Napolitano LM, Wexner SD, et al. Enteric fistulas: principles of management. J Am Coll Surg. 2009;209:484-91. [ Links ]
2. Qadeer MA, Dumot JA, Vargo JJ, Lopez AR, Rice TW. Endoscopic clips for closing esophageal perforations: case report and pooled analysis. Gastrointest Endosc. 2007;66:605-11. [ Links ]
3. Cho SB, Lee WS, Joo YE, Kim HR, Park SW, Park CH, et al. Therapeutic options for iatrogenic colon perforation: feasibility of endoscopic clip closure and predictors of the need for early surgery. Surg Endosc. 2012;26:473-9. [ Links ]
4. Magdeburg R, Collet P, Post S. Endoclipping of iatrogenic colonic perforation to avoid surgery. Surg Endosc. 2008;22:1500-4. [ Links ]
5. Will U, Meyer F, Hartmeier S, Schramm H, Bosseckert H. Endoscopic treatment of a pseudocystocolonic fistula by band ligation and endoloop application: case report. Gastrointest Endosc. 2004;59:581-3. [ Links ]
6. Rabago LR, Ventosa N, Castro JL, Marco J, Herrera N, Gea F. Endoscopic treatment of postoperative fistulas resistant to con- servative management using biological fibrin glue. Endoscopy. 2002;34:632-8. [ Links ]
7. Disibeyaz S, Parlak E, Koksal AS, Cicek B, Koc U, Sahin B. Endoscopic treatment of a large upper gastrointestinal anastomotic leak using a prolene plug and cyanoacrylate. Endoscopy. 2005;37:1032-3. [ Links ]
8. Endo M, Inomata M, Terni T, Oana S, Kudara N, Obara H, et al. New endoscopic technique to close large mucosal defects after endoscopic mucosal resection in patients with gastric mucosal tumors. Dig Endosc. 2004;16:372-5. [ Links ]
9. Kirschniak A, Kratt T, Stüker T, Braun A, Schurr MO, Königsrainer A new endoscopic over-the-scope clip system for treatment of lesions and bleeding in GI tract: first clinical experiences. Gastrointest Endosc. 2007;66:162-7. [ Links ]
10. Repici A, Arezzo A, De Caro G, Morino M, Pagano N, Rando G, et al. Clinical experience with a new endoscopic over-the-scope clip system for use in the GI tract. Dig Liver Dis. 2009;41:406-10. [ Links ]
11. Seebach L, Bauerfeind P, Gubler C. Sparing the surgeon: clinical experience with over-the-scope clips for gastrointestinal perforation. Endoscopy. 2010;42:1108-11. [ Links ]
12. Parodi A, Repici A, Pedroni A, Blanchi S, Conio M. Endoscopic management of GI perforations with a new over-the-scope clip device. Gastrointest Endosc. 2010;72:881-6. [ Links ]
13. Renteln D, Denzer UW, Schachschal G, Anders M, Groth S, Rösch T. Endoscopic closure of GI fistulae by using an over-the-scope clip. Gastrointest Endosc. 2010;72:1289-96. [ Links ]
14. Manta R, Manno M, Bertani H, et al. Endoscopic treatment of gastrointestinal fistulas using an over-the-scope clip (OTSC) device: case series from a tertiary referral center. Endoscopy. 2011;43:545-8. [ Links ]
15. Kirschniak A, Subotova N, Zieker D, Königsrainer A, Kratt T. The over-the-scope clip for the treatment of gastrointestinal bleeding, perforations, and fistulas. Surg Endosc. 2011;25: 2901-5. [ Links ]
16. Pohl J, Borgulya M, Lorenz D, Ell C. Endoscopic closure of post- operative esophageal leaks with a novel over-the-scope clip system. Endoscopy. 2010;42:757-9. [ Links ]
17. Surace M, Mercky P, Demarkuay JF, Gonzalez JM, Dumas R, Ah-Soune P, et al. Endoscopic management of GI fistulae with the over-the-scope clip system. Gastrointest Endosc. 2011;74:1416-9. [ Links ]
18. Baron TH, Song LM, Ross A, Tokar JL, Irani S, Kozarek RA. Use of an over-the-scope clipping device: multicenter retrospective results of the first U.S. experience (with videos). Gastrointest Endosc. 2012;76:202-8. [ Links ]
19. Correia T, Amaro P, Sofia C. Tratamento de deiscência cirúrgica grave com sistema Over-the-scope clip. GE - J Port Gastrenterol. 2013;20:261-5. [ Links ]
20. Hyman NH. Managing anastomotic leaks from intestinal anastomoses. Surgeon. 2009;7:31-5. [ Links ]
21. Iqbal CW, Cullinane DC, Schiller HJ, Sawyer MD, Zietlow SP, Farley DR. Surgical management and outcomes of 165 colonoscopic perforations from a single institution. Arch Surg. 2008;143:701-6. [ Links ]
22. Araujo SE, Seid VE, Caravatto PP, Dumarco R. Incidence and management of colonoscopic colon perforations: 10 years experience. Hepato-gastroenterol. 2009;56:1633-6. [ Links ]
23. Kantsevoy SV, Adler DG, Conway JD, Diehl DL, Farraye FA, Kwon R, et al. Endoscopic mucosal resection and endoscopic submu- cosal dissection. Gastrointest Endosc. 2008;68:11-8. [ Links ]
24. Mangiavillano B, Viaggi P, Masci E. Endoscopic closure of acute iatrogenic perforations during diagnostic and therapeutic endoscopy in the gastrointestinal tract using metallic clips: a literature review. J Dig Dis. 2010;11:12-8. [ Links ]
25. Feith M, Gillen S, Schuster T, Theisen J, Friess H, Gertler R. Healing occurs in most patients that receive endoscopic stents for anastomotic leakage; dislocation remains a problem. Clin Gastroenterol Hepatol. 2011;9:202-10. [ Links ]
26. Albert JG, Friedrich-Rust M, Woeste G, Strey C, Bechstein WO, Zeuzem S, et al. Benefit of a clipping device in use in intestinal bleeding and intestinal leakage. Gastrointest Endosc. 2011;74:389-97. [ Links ]
27. Nishiyama N, Mori H, Kobara H, Rafiq K, Fujihara S, Kobayashi M, et al. Efficacy and safety of over-the-scope clip: including complications after endoscopic submucosal dissection. World J Gastroenterol. 2013;19:2752-60. [ Links ]
*Corresponding author
E-mail address: Titocorreia@gmail.com (T. Correia).
Ethical disclosures
Protection of human and animal subjects. The authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of data. The authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interest
The authors have no conflicts of interest to declare.
Received 14 January 2014; accepted 27 March 2014














