Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.22 no.1 Lisboa fev. 2015
https://doi.org/10.1016/j.jpge.2014.07.005
ENDOSCOPIC SNAPSHOT
Single-balloon Enteroscopy Assisted Endoscopic Retrograde Cholangiopancreatography with the Rendezvous Technique
Colangiopancreatografia Retrógrada Endoscópica com Enteroscópio Utilizando a Técnica de Rendezvous
Teresa Pinto Pais a,∗, Rolando Pinhoa, Luísa Proençaa, Carlos Fernandesa, Iolanda Ribeiroa, Tiago Pereirab, João Carvalhoa, José Fragaa
a Gastrenterology and Hepatology Department, Centro Hospitalar de Gaia/Espinho, Gaia, Portugal
b Radiology Department, Centro Hospitalar de Gaia/Espinho, Gaia, Portugal
* Corresponding author.
Endoscopic retrograde cholangiopancreatography (ERCP) in patients with surgically altered upper gastrointestinal anatomy such as a Roux-en-Y anastomosis is challenging. The use of balloon-assisted enteroscopy allows evaluation of the surgically excluded segment, access to the biliopancreatic tract and performance of endoscopic therapy.
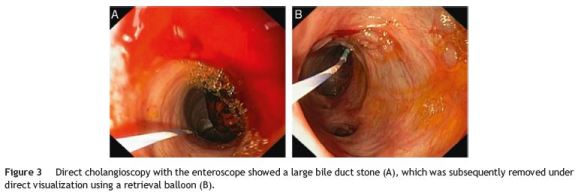
A 79-year-old female patient, with history of cholecistectomy (2005) and total gastrectomy with Roux-en-Y anastomosis for gastric cancer (pT2N0M0, 2007), suffered from recurrent episodes of cholangitis (2012). Abdominal ultrasonography revealed pronounced bile duct dilation (20 mm) caused by a large gallstone (17 mm) in the distal third of the common bile duct. After a failed standard ERCP, a percutaneous transhepatic biliary drainage (PTBD) was initially performed to relieve the obstruction. However, stone extraction was not accomplished. Therefore, she was referred to us for SBE-assisted ERCP, which was performed using a rendezvous technique, since there was a previously placed PTDB. The SBE (SIF-Q180 Olympus Medical Systems, Tokyo, Japan) was advanced to the afferent limb up to the papilla, where externalization of the percutaneously inserted guidewire was observed. A 4 Fr catheter (0.038´´ 65 cm, Cordis) was placed over the wire and the percutaneous guidewire removed. A 500 cm 0.0035´ guidewire (Endoflex 21535500, Germany) was placed percutaneously through the catheter and grasped with a standard polypectomy snare. Then, biliary cannulation over the guidewire using the rendezvous technique was performed. Only limited sphincterotomy was achievable, due to the use of a longer (280 cm) conventional sphincterotome (Endoflex OE1042230DL-280, Germany) (Fig. 1). To safely perform a large sphincterotomy, a long Bilroth II-type sphincterome should be used, due to the retrograde approach. Subsequently, endoscopic papillary dilation was performed using a standard 12-15 mm balloon (CRE Boston Scientific, Tokyo, Japan), under direct visualization and radiologic control (Fig. 2). Peroral direct cholangioscopy (PDCS) was possible with the enteroscope, owing to pronounced biliary dilation. The large bile duct stone was removed under direct visualization using a retrieval balloon (Fig. 3). Finally, residual gallstones were excluded by PDCS and PTDB cholangiogram. There were no procedure-related complications. The patient had an uneventful recovery, and remains stable after 2-year follow-up.
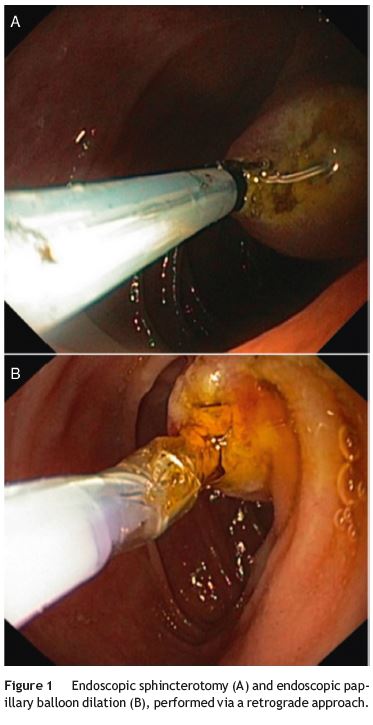

Balloon-assisted enteroscopy-ERCP is now an accepted interventional modality in patients with complex postsurgical anatomy, such as Roux-en-Y anatomy.1 The enteroscope allows deep insertion into the small bowel and access to the papilla and the biliary tract. However, cannulation and sphincterotomy are technically difficult with a forwardviewing instrument, via retrograde approach. Additionally, the use of devices, such as dilating balloons, through a narrow and long working channel is limited. Also, the device maneuverability is difficult, particularly from looping and twisting scope position.2,3 A systematic review by Skinner et al. reported an overall ERCP success of approximately 74%, due to these limitations.4
Traditionally used in conventional ERCP, the rendezvous technique has improved the success rate of biliary cannulation in enteroscope-assisted ERCP. The SBE-ERCP rendezvous technique presented herein allowed successful therapeutic techniques such as sphincterotomy, papillary balloon dilation and biliary stone extraction, under direct endoscopic view. Our case, as other recent reports, illustrates the gradual disappearance of barriers for endoscopic biliary interventions in patients with altered upper gastrointestinal tract anatomy.5
References
1. Mönkemüller K, Popa D, McGuire B, Ramesh J, Wilcox CM. Doubleballoon enteroscopy-ERCP rendezvous technique. Endoscopy. 2013;45:E333-4. [ Links ]
2. Itokawa F, Itoi T, Ishii K, Sofuni A, Moriyasu F. Singleand double-balloon enteroscopy-assisted endoscopic retrograde cholangiopancreatography in patients with Roux-en-Y plus hepaticojejunostomy anastomosis and Whipple resection. Dig Endosc. 2014;26 Suppl. 2:136-43. [ Links ]
3. Skinner M, Popa D, Neumann H, Wilcox CM, Mönkemüller K. ERCP with the overtube-assisted enteroscopy technique: a systematic review. Endoscopy. 2014;46:560-72. [ Links ]
4. Mönkemüller K, McGuire B, Wilcox CM, Ramesh J, DuBay D, Eckhoff D. Percutaneous balloon dilation and placement of endoscopic biliary stent by using the double-balloon enteroscopy ERCP rendezvous technique. Gastrointest Endosc. 2013;78:383-5. [ Links ]
5. Pinho R, Proença L, Alberto L, Carvalho J, Pinto-Pais T, Fernandes C, et al. Biliary self-expandable metallic stent using single balloon enteroscopy assisted ERCP - overcoming limitations of current accessories. Rev Esp Enferm Dig. 2013;105:561-4. [ Links ]
*Corresponding author
E-mail address: teresapintopais@gmail.com (T. Pinto Pais).
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interest
The authors have no conflicts of interest to declare.
Received 8 May 2014; accepted 14 July 2014














