Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.22 no.6 Lisboa dez. 2015
https://doi.org/10.1016/j.jpge.2015.06.005
ENDOSCOPIC SNAPSHOT
Brunners Gland Hamartoma - A Rare Cause of Upper Gastrointestinal Bleeding
Hamartoma das Glândulas de Brunner - Uma Causa Rara de Hemorragia Digestiva Alta
Sandra Barbeiro∗, Catarina Atalaia Martins, Pedro Marcos, Cláudia Gonçalves
Gastroenterology Department, Centro Hospitalar de Leiria, Leiria, Portugal
* Corresponding author.
Keywords: Brunner Glands; Gastrointestinal Hemorrhage; Hamartoma
Palavras-Chave: Glândulas de Brunner; Hemorragia Gastrointestinal; Hamartoma
1. Case report
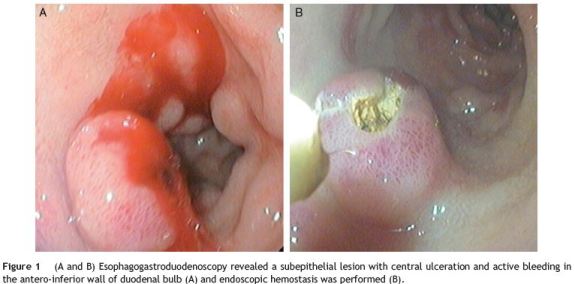
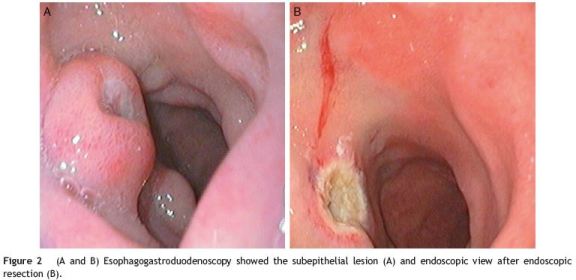
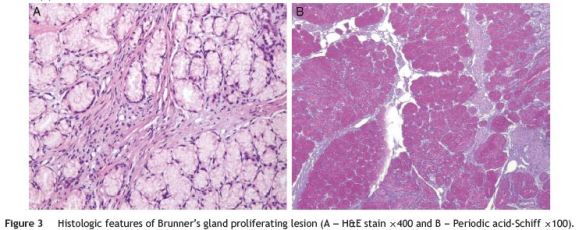
A 45-year-old male presented with recent melena. He referred recent anti-inflammatory drugs for a leg trauma. At physical examination, slight tachycardia and pallor was noted. Laboratory tests showed anaemia (9.2 g/dL). Esophagogastroduodenoscopy demonstrated a 1.0 cm subepithelial lesion with central ulceration and blood oozing in the antero-inferior wall of duodenal bulb (Fig. 1A). Endoscopic hemostasis with adrenaline injection and argon plasma coagulation was achieved (Fig. 1B) and no bleeding recurrence was observed. Later, endoscopic biopsies were taken, but pathologic examination was inconclusive. Endoscopic ultrasound revealed a 1.1 cm hypoechoic lesion with regular margins and limited to the submucosa. Enbloc endoscopic resection was performed. Histological examination allowed diagnosis of Brunners glands hamartoma and confirmed complete resection (Figs. 2 and 3). Endoscopy performed five months after resection revealed that the duodenal bulb was normal and confirmed a complete resection.
2. Discussion
Brunners glands are submucosal mucin-secreting glands, mainly located in the first and second portions of the duodenum.1 Duodenal tumours are rare and Brunners gland hamartoma comprises 5-10% of these tumours (an estimate incidence of 0.008%).1,2 Most cases occur in the fifth and sixth decades of life, with neither gender nor race predominance.4 Brunners gland hamartoma is usually a solitary lesion with 1.0-2.0 cm often incidentally found during imaging or endoscopic studies.1,2 Its pathogenesis remains unknown. Hyperchlorhydria, Helicobacter pylori infection and chronic pancreatitis have been suggested as possible causes, but none has ever been proven.1,3
In the majority of cases, patients are asymptomatic. Occasionally, Brunners gland hamartoma may cause haemorrhage or intestinal obstruction.1,4 Endoscopic biopsy is frequently negative because it is not deep enough to reach the submucosa.1 Removal of the suspected Brunners gland hamartoma is recommended to confirm the diagnosis as well as to avoid potential complications. Endoscopic polypectomy, the ideal approach method, is more cost-effective and less invasive than surgery.1 Decision depends on the location and size of the tumour as well as the patients symptoms and status.2,3 Although mainly benign in nature, malignant transformations are occasionally described, but recurrences after resection have not been reported.2,3
References
1. Rocco A, Borriello P, Compare D, De Colibus P, Pica L, Iacono A, et al. Large Brunners gland adenoma: case report and literature. World J Gastroenterol. 2006;12:1966-8. [ Links ]
2. Qayed E, Wehbi M, Rutherford R. Gastrointestinal bleeding from Brunner gland hamartoma. Clin Gastroenterol Hepatol. 2011;9:e4-5. [ Links ]
3. Wang Y, Kuo Y, Lu C. A rare cause of gastrointestinal bleeding. Gastroenterology. 2013;145:261-2. [ Links ]
4. Levine JA1, Burgart LJ, Batts K, Wang KK. Brunners gland hamartomas: clinical presentation and pathological features of 27 cases. Am J Gastroenterol. 1995;90:290-4.
* Corresponding author.
E-mail address: sandrabarbeiro@gmail.com (S. Barbeiro).
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that no patient data appear in this article.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Conflicts of interest
The authors have no conflicts of interest to declare.
Received 28 February 2015; accepted 30 June 2015














