Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.23 no.1 Lisboa fev. 2016
https://doi.org/10.1016/j.jpge.2015.07.007
REVIEW ARTICLE
Contrast-Enhanced Cross Sectional Imaging and Capsule Endoscopy: New Perspectives for a Whole Picture of the Small Bowel
Cápsula Endoscópica e Estudos Imagiológicos Contrastados: Diferentes Perspectivas para uma Imagem Mais Completa do Intestino Delgado
Pedro Boal Carvalhoa,∗, José Cottera,b,c
a Gastroenterology Department, Centro Hospitalar do Alto Ave, Guimarães, Portugal
b Life and Health Sciences Research Institute (ICVS), School of Health Sciences, University of Minho, Braga, Portugal
c ICVS/3Bs, PT Government Associate Laboratory, Guimarães, Portugal
* Corresponding author.
ABSTRACT
Small bowel evaluation is a challenging task and has been revolutionized by high-quality contrasted sectional imaging (CT enterography - CTE) and magnetic resonance enterography (MRE) as well as by small bowel capsule endoscopy (SBCE).
The decision of which technique to employ during the investigation of small bowel diseases is not always simple or straight forward. Moreover, contraindications may preclude the use of these techniques in some patients, and although they are noninvasive procedures, may present with various complications.
SBCE plays a crucial role in the investigation of both obscure gastrointestinal bleeding and Crohns Disease, but it is also useful for surveillance of patients with Peutz-Jeghers Syndrome, while CTE is very accurate in small bowel tumours and in established Crohns Disease, and its use in patients presenting with gastrointestinal bleeding is increasing. MRE, an expensive and not widely available technique, is essential for the study of patients with Crohns Disease, and presents an attractive alternative to SBCE in Peutz-Jeghers syndrome surveillance.
These diagnostic modalities are often not competitive but synergistic techniques. Knowing their characteristics, strengths and limitations, indications, contraindications and potential complications, as well as the adaptation to local availability and expertise, is essential to better select which procedures to perform in each patient, both safely and effectively, in order to optimize management and improve patient outcomes.
Keywords: Chronic Disease; Capsule Endoscopy; Gastrointestinal Hemorrhage; Intestinal Neoplasms; Small Intestine
RESUMO
A investigação do intestino delgado, previamente difícil e limitada, sofreu uma revolução com o aparecimento de técnicas imagiológicas contrastadas de elevada qualidade, como a enterografia por tomografia axial computadorizada (enteroTC) e a enterografia por ressonância magnética (enteroRM), assim como pela enteroscopia por cápsula (EC).
A decisão na escolha da técnica a utilizar nas diferentes patologias do intestino delgado não é na maioria das vezes simples ou óbvia. Adicionalmente, a presença de contraindicações pode restringir o uso destas técnicas em alguns doentes, e apesar de não serem consideradas técnicas invasivas, não são isentas de riscos e complicações.
A EC tem um papel crucial na investigação da hemorragia digestiva de causa obscura e da Doença de Crohn, mas tem-se revestido também de utilidade na vigilância de doentes com Síndrome de Peutz-Jeghers; a enteroTC revelou uma elevada capacidade diagnóstica para neoplasias do intestino delgado e na Doença de Crohn estabelecida, e a sua utilização na hemorragia digestiva de causa obscura tem vindo a expandir. A enteroRM, apesar de dispendiosa e de disponibilidade limitada, tem uma elevada eficácia no estudo da Doença de Crohn, e é uma alternativa válida à EC no Síndrome de Peutz-Jeghers.
Estas técnicas diagnósticas são frequentemente singergísticas e complementares, ao invés de competitivas. O reconhecimento das suas características, das suas capacidades e limitações, assim como das indicações, contraindicações e potenciais complicações, e aliado à adaptação à disponibilidade e competências locais, é essencial na correcta escolha de procedimentos seguros e eficazes para cada doente, de forma a optimizar a abordagem e o prognóstico.
Palavras-Chave: Doença de Crohn; Enteroscopia por Cápsula; Hemorragia Gastrointestinal; Intestino Delgado; Neoplasias Intestinais
1. Introduction
The study of the small bowel has been traditionally limited to low yield techniques, such as push enteroscopy and small bowel follow-through, or invasive techniques such as intraoperative enteroscopy.
By the end of the past century, cross-sectional imaging techniques with excellent resolution, namely CT enterography (CTE) and magnetic resonance enterography (MRE), were developed to better observe and characterize small bowel pathology, while a new contender, small bowel capsule endoscopy (SBCE) has been shown to provide excellent diagnostic yield in a myriad of small bowel diseases.
The choice of what technique or even which combination to use for small bowel study in the different clinical settings encountered daily is often challenging, and depends on technical characteristics but also on local expertise and availability.
2. Technical characteristics
CTE was developed in 1997 to better assess small bowel Crohns Disease (CD).1 The preparation for CTE includes a clear liquid diet for the 4-6 h previous to the examination, as well as the administration of 1000-2000 cc of an oral contrasting agent, usually over 45-60 min, followed by intravenous contrast during image acquisition.2 Oral contrast is used in order to accomplish bowel distension and maximize the contrast between the lumen and the bowel wall.2 CT enteroclysis, where oral contrast is administered through a nasojejunal tube, allows for superior jejunal distension,3 but poor patient tolerance and low efficiency limits its use.2 A number of oral neutral contrasting agents are available, including methylcellulose, polyethylene glycol, manitol, low-density barium solution and water alone the latter is rapidly absorbed, resulting in poor distension, particularly in the distal ileum, and may contribute to fluid overload.2 For the intravenous contrast, 100-150 cc of an iodine-based contrasting agent is used, and as in regular CT, caution should be employed in the prevention of iodine nephropathy, particularly in diabetic and elderly patients.2,4
A prokinetic, such as metoclopramide (10-20 mg po), is often administered at the start of the oral contrasting agent ingestion, and hyoscine butylbromide (20 mg iv) at the start of the intravenous contrasting agent in order to reduce peristalsis imaging artefacts.2
MRE was more recently made available to clinicians, but the same core principles apply in regards to CTE. After a 4-6 h fast, 1000-2000 cc of a biphasic water-based oral contrast similar to the ones used during CTE is administered, often with metoclopramide (10-20 mg po), followed by a gadolinium-based intravenous contrast (0.65 mg/kg) together with either hyoscine butylbromide (20 mg iv) or glucagon (0.5 mg iv).5,6
Small bowel capsule endoscopy (SBCE) was first unveiled in 2001.7 For the procedure, ESGE guidelines support the indication for a clear liquid diet on the day preceding the exam, as well as a 12 h fast.7 A purgative bowel preparation (commonly using 1000-3000 cc polyethylene glycol-based solutions) is often administered before capsule ingestion as it was shown to significantly improve the diagnostic yield (OR 1.68; 95% CI 1.16-2.42).8 Just as well, the antifoaming agent simethicone (300 mg po before capsule ingestion) results in a significantly better mucosal visualization by reducing the presence of air bubbles inside the intestinal lumen.8-10 To prevent incomplete SBCE, domperidone (10 mg po) has been advocated, for its use was significantly associated with a higher rate of procedure completion by reducing gastric transit time,11 despite the fact that newer capsules, with prolonged battery duration, may in the future obviate the need for prokinetics in SBCE.12
3. Contraindications and complications
Immediate complications related to CTE and MRE are rare, and most frequently associated with intravenous contrast administration. When transient physiologic responses to the contrast (e.g. localized warmth sensation) were excluded, immediate adverse reactions following intravenous contrast administration were recently reported to be as low as 0,6%13,14 in two large series of paediatric and adult populations, and resolved without complications after prompt treatment administration (corticosteroids or epinephrine) in the vast majority of the cases. Moreover, severe adverse effects are rare (<1 in 1000),13,14 and a large scale Japanese study showed no deaths attributed to adverse reactions to intravenous fluid injection in 170,000 patients.15 Nevertheless, history of asthma, allergy requiring medication or previous allergic reaction to the contrast should alert the clinician to either avoid administration of the contrast or consider the use of premedication with corticosteroids, as well as having the equipment for resuscitation made available.15 Contrast nephropathy occurs in 1.6-2.3% of the patients,16 but this risk is sharply increased in patients with impaired renal function, diabetes or elderly age.
Delayed complications may occur in up to 50% of the patients,2,17 includingskin rash, fever, musculoskeletal pain, nausea, vomit, while very late adverse reactions are rare but significant, such as iodine-based thyrotoxicosis and gadolinium-associated nephrogenic systemic fibrosis. Cumulative ionizing radiation exposure constitutes another complication of CTE. In fact, up to 2% of the neoplasia incidence may be due to radiation, and the lifetime risk of neoplasia resulting of CT procedures is 2-4 in 10,000 patients.18 This risk is dose but also age-related, with the paediatric population representing the highest risk group, and patients aged over 40 having a very low risk of future CT radiation implications.19
With capsule endoscopy, the most frequently observed complication is capsule retention, defined as the presence of the capsule within the patients bowel after 14 days of capsule ingestion, with an overall incidence of 1-2%.20 Such risk is very low among healthy volunteers, as well as in patients presenting with OGIB or suspected CD, but increased in patients with history of NSAID consumption, abdominal surgery or radiation, and particularly in patients with established CD or small bowel neoplasias, in which the incidence of retention may reach 13% and 25%, respectively.7,20,21 Other complications, such as bowel perforation or capsule aspiration, are exceedingly rare.22,23 Current capsule endoscopy guidelines consider the following as contraindications to capsule endoscopy: pregnancy, suspected bowel obstruction, swallowing disorders and imminent MRI procedure.7,21 Nevertheless, there is a possibility for endoscopic placement of the capsule in the duodenum for patients with swallowing disorders,21 which should also be considered in patients with previous gastric surgery (e.g. partial gastrectomy with Billroth II anastomosis)24 and patients with delayed gastric emptying.21 Additionally, no complications were reported in pregnant women submitted to SBCE during the first trimester,7 and in certain settings, SBCE was proven to be safe and feasible even in patients with known small bowel stenoses.25 Finally, paediatric age21 and pacemakers or implantable cardioverter defibrillators7,26 are no longer considered contraindications to SBCE.
Pregnancy is also a contraindication to CTE, not only secondary to ionizing radiation,18 but because iodinated contrast may depress neonatal thyroid function,27 as well as to MRE, due to concerns regarding the teratogenic potential of gadolinium.27 Other contraindications to CTE include known allergy to iodine-based contrast14 and impaired renal function18; young age, particularly in the setting of inflammatory bowel diseases or Peutz-Jeghers syndrome, where multiple small bowel evaluations are warranted throughout a lifetime, may also constitute a relative contraindication to CTE.28,29 MRE is contraindicated in patients with metallic foreign objects and depressed renal function,30 but may be used in claustrophobic and younger patients if light sedation is available.30
4. Inflammatory bowel disease
Both cross-sectional imaging and SBCE have uses in a multitude of diseases, but nowhere is the clinical decision of which technique to employ more frequent and influential than on patients with inflammatory bowel diseases.
CTE exhibits high spatial resolution, allowing for accurate imaging of mural and extra-luminal diseases, especially when a multidetector row is used.2,4 The sensitivity for CTE in the context of established CD is up to 90%,31,32 and typical radiological findings include mucosal hyperenhancement, mural thickening (>3-4 mm is considered abnormal, and up to 2 cm may be observed in CD), ulceration, mesenteric inflammation and engorgement of vasa recta (resulting in the classical comb sign)2,33 ; extra-luminal CD findings, such as abdominal abscesses and fistulae may also be observed and characterized.2 Likewise, MRE allows for the diagnosis of both intestinal and extra-intestinal abnormalities in CD, and the radiological findings are similar between the two techniques. MRE, in particular, exhibits a very high sensitivity and specificity (up to 84% and 100%, respectively) in the evaluation of intra-abdominal fistulae.4 A common concern among CD patients submitted to CTE is the cumulative radiation exposure, particularly as these patients are often of younger age and present with multiple relapses of disease activity.4
CD is one of the main indications for SBCE, both for diagnosis as well as for known disease. It allows for mucosal evaluation of the entire small bowel, and for the detection of CD lesions such as villous oedema, erosions, ulcers and stenoses.7 SBCE has been shown to display a high sensitivity for CD, significantly superior to other diagnostic modalities, including both CTE34 and MRE,35 particularly for proximal and superficial lesions,35,36 resulting in a very high negative predictive value, ranging from 96 to 100%.37 In fact, SBCE has recently been shown to be equivalent to ileocolonoscopy in the diagnostic yield of small bowel CD.38 Furthermore, inflammatory activity on the proximal small bowel detected on SBCE has been shown to have a significant impact on disease course and was independently associated with a significant risk of relapse,39 and directly contributed to changes in the therapeutical approach in up to 30% of patients with known CD.40 Inflammatory activity scores such as the CECDAI (or Niv Score)41 and the Lewis Score42-44 have been developed and validated in order to quantify inflammation severity, extent and distribution.41,43
Nevertheless, when compared to both CTE and MRE, SBCE presents a lower specificity,33,45 in part due to the fact that up to 20% of healthy subjects may present small bowel erosions during SBCE,46 but also because small bowel lesions akin to CD may be encountered in other entities, such as during non-steroidal anti-inflammatory drug use.47 Additionally, SBCE in the setting of established CD is usually limited to patients with non-stricturing non-penetrating diseases, although recent evidence suggests that the capsule may be able to traverse CD small bowel stenoses in the majority of the patients.25 The use of the patency capsule, a device with dissolvable components precluding the occurence of obstruction, identifies patients with an increased risk of SBCE retention, and it is currently recommended by the ESGE guidelines before performing SBCE in patients with established CD.47
In patients with suspected CD with a negative ileocolonoscopy, current ECCO48 and ESGE47 guidelines consider SBCE to be a first-line examination in the absence of obstructive symptoms, whereas in such patients, crosssectional imaging should be preferred. On the other hand, in patients with established CD, cross-sectional imaging, with the potential to assess both intestinal and extra-intestinal disease, should be the modality of choice to evaluate the small bowel, preferably MRE due to absence of ionizing radiation. SBCE should be reserved to patients with unexplained symptoms or OGIB, when MRE/CTE are inconclusive.
5. Obscure gastrointestinal bleeding
OGIB has been defined as bleeding of unknown origin that persists or recurs after a negative initial endoscopy study (esophagogastroduodenoscopy and colonoscopy).49
OGIB may be responsible for up to 5% of all gastrointestinal haemorrhage,50 and in the vast majority of the cases, originates within the small bowel.7 Currently, SBCE is considered to be the first-line investigation in patients presenting with OGIB,47 demonstrating very high sensitivity and specificity (up to 95% and 75%, respectively) when compared to the gold standard of intraoperative enteroscopy,51 and resulting in clinical management changes in two thirds of the patients.52
The diagnostic yield of SBCE in OGIB has been reported to be up to 60% in recent meta-analysis and systematic reviews,20,53 significantly superior to other diagnostic modalities, such as push-enteroscopy (56% vs. 26%)54 and angiography (53% vs. 20%)55 and non-inferior to double balloon enteroscopy (62% vs. 56%).53 Independent risk factors associated with an increased diagnostic yield of SBCE in OGIB include the presence of overt OGIB,56 shorter interval between presentation and the procedure,57 recurrent OGIB with >6 months of duration or more than one bleeding episode,21 advanced age50 and antithrombotic use.58 The diagnostic yield may be further improved by the use of chromoendoscopy techniques, such as the Flexible Spectral Imaging Colour Enhancement (FICE, Fujinon Corporation® , Saitama, Japan), incorporated in Given Imaging® (Yoqneam, Israel) software, that enhance surface patterns to better observe mucosal lesions,59-61 and the use of such techniques should be considered in patients where a strong suspicion for small bowel abnormalities remain despite a negative SBCE.
Nevertheless, a negative SBCE does not always preclude important small bowel lesions, and while OGIB recurrence has been shown to be less likely in this setting,62 a recent study reported rebleed rates of up to 25% during long-term follow-up.63 In these patients, further investigation may be warranted, and CTE presents as a valid alternative. Studies have shown that SBCE is associated with an increase in diagnostic yield of 20-40%64,65 when compared to CTE, and this advantage was even more pronounced in superficial lesions with no luminal repercussion, such as vascular malformations,65 the most frequently observed origin of OGIB (20-55%).66 However, CTE may be the superior diagnostic modality in some cases, particularly during massive overt OGIB, where SBCE may be unable to locate or define the origin of the bleeding,67 and in patients with small bowel tumours.68
Few studies have reported on the usefulness of MRE in the context of OGIB, but its use it limited by a lower spatial resolution than CTE,5 reduced availability in the urgent setting,6 and cost.69 When compared to SBCE, MRE demonstrated a significantly inferior diagnostic yield (53% vs. 21%).70
6. Small bowel tumours and Peutz-Jeghers syndrome
Small bowel tumours are rare, accounting for less than 5% of gastrointestinal neoplasias and less than 0.5% of all tumours.5,7,71 The most common indication for investigation in patients presenting with small bowel tumours is OGIB, in 70 to 90% of the cases.7 In fact, small bowel tumours are responsible for OGIB in 10-20% of the patients, second in frequency to vascular malformations, and ahead of CD (2-10%) and NSAID enteropathy (5%).66 Moreover, in patients under 40 years, small bowel tumours overcome vascular malformations as the leading cause of OGIB originating in the small bowel.66
Nevertheless, a low prevalence of small bowel tumours, coupled with their predominant location in the jejunum, nonspecific presentation of OGIB, abdominal pain and weight loss, frequently leads to delayed investigation and advanced neoplasia at diagnosis.71
The advent of SBCE allowed a paradigm shift, and recent studies have shown SBCE to detect small bowel neoplasia in patients with a previous work-up of 2-4 procedures,71 and impact management decision in 55-80% of the cases.71,72 There are, however, limitations to SBCE in the diagnosis of small bowel tumours: SBCE exhibits a false negative rate of up to 66% in the proximal small bowel or in submucosal lesions, even in large and protruding lesions,73 because of limited field of vision, folds and loop angulations, poor bowel preparation, rapid transit time, non-continuous image capture and incomplete examination; additionally, SBCE is unable to adequately characterize both the size and the location of the tumour,21,73 and presents a retention rate of up to 25% in such patients.7
CTE sensitivity and specificity for small bowel tumours have been reported to be up to 93% and 99%, respectively.2,74 Furthermore, CTE is able to adequately locate and characterize both location, size, extra-intestinal invasion and metastatic disease (lymphatic and disseminated).74 In a recent prospective study, CTE with a 64-section multidetector row demonstrated a superior diagnostic yield when compared to SBCE (88 vs. 38%), and this difference largely resulted from the detection of 100% of small bowel tumours compared to only 33% observed with SBCE,68 and these results were replicated in other published reports.2,5,74 As a result, CTE should be considered as a valid alternative to SBCE as a first line diagnostic procedure in younger patients presenting with OGIB, a population where small bowel tumours are the most prevalent finding.66
The use of MRE for small bowel tumour diagnosis is limited due to its lower spatial resolution and susceptibility for movement artefacts, but, similarly to CTE, it allows for the tumour characterization, as well as the assessment of metastatic disease.5,6
Peutz-Jeghers syndrome (PJS) is an autosomal dominant condition presenting with mucocutaneous pigmentation and gastrointestinal hamartomatous polyps.29 Almost 90% of PJS patients present with small bowel polyps, and the chief indication for small bowel surveillance is the significantly increased risk of intussusception,75 particularly in larger polyps76 by age 20, intussusception has occurred in half the patients with PJS, and, in the majority of them, presented with acute abdomen requiring surgical approach.77 In the European Mallorca consensus of 2007, the decision was made to use SBCE in the screening and surveillance of PJS every 2-3 years after 8 years of age and in symptomatic patients,76 and these recommendations were adapted and incorporated in the recently published ACG guidelines on the management of hereditary gastrointestinal cancer syndromes, allowing for the second small bowel SBCE to be delayed until the age of 18, if the first SBCE detected no polyps, and no symptoms developed.77
Nevertheless, SBCE has been shown to miss the detection of up to 20-40%78,79 of PJS small bowel polyps, including large polyps78 as well as those in the proximal small bowel.79,80 Recently, a number of authors have reported superior capabilities of SBCE versus MRE in polyps <10 mm,81 equivalence of both techniques in polyps 10-15 mm,81,82 but crucially, MRE superiority in diagnostic yield, as well as better size and location estimation, in larger small bowel polyps.29,47,81,82 This advantage of MRE was not observed in another prospective study, where a polyp of 30 mm was missed by MRE, and identified during SBCE.83 Thus, current ESGE guidelines consider small bowel surveillance to be adequate with both SBCE and MRE, depending on availability and local expertise.47
No role exists for CTE in PJS, due to the repeated need for small bowel assessment in young patients, resulting in an unacceptable ionizing radiation exposure.29
7. Conclusion
In conclusion, SBCE remains the first-line examination for OGIB, and plays a key role in the diagnosis of CD, as well as the surveillance of PJS. Its use on small bowel tumours and established CD, however, should be reserved to selected cases due to the risk of retention and inability to precisely define location and extra-intestinal involvement of either pathology.
CTE has proven to be the most effective modality in the study of small bowel tumours, and may be used in the diagnostic work-up of OGIB in patients where this diagnosis is more likely to occur. CTE should also be considered both in suspected and established CD, but ionizing radiation exposure should pose concerns, particularly in younger patients.
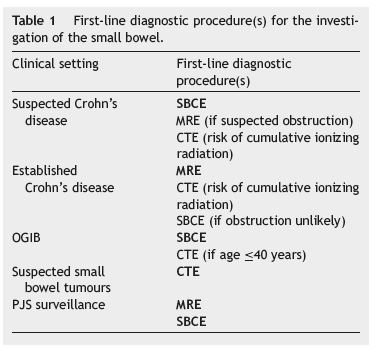
Finally, the importance of MRE in the study of CD is growing as a non-invasive non-ionizing technique with the possibility to characterize both mucosal injury and penetrating disease, and provides an alternative to SBCE in PJS patients. Nevertheless, local expertise and availability is asymmetric, and a limitation to the broad use of this technique. Table 1 summarizes the main indications for SBCE, CTE and MRE, as well as the first-line modalities for each clinical setting.
In clinical practice, SBCE, CTE and MRE are often not competitive but synergistic techniques; the knowledge of their characteristics, strengths and limitations, indications and contraindications, as well as the adaptation to local availability and expertise, is crucial to select the best sequence of examinations for each specific situation, in order to optimize diagnostic algorithms and ultimately clinical management and outcomes.
References
1. Raptopoulos V, Schwartz RK, McNicholas MM, Movson J, Pearlman J, Joffe N. Multiplanar helical CT enterography in patients with Crohns disease. Am J Roentgenol. 1997;169:1545-50. [ Links ]
2. Ilangovan R, Burling D, George A, Gupta A, Marshall M, Taylor SA. CT enterography: review of technique and practical tips. Br J Radiol. 2012;85:876-86. [ Links ]
3. Schmidt S, Felley C, Meuwly JY, Schnyder P, Denys A. CT enteroclysis: technique and clinical applications. Eur Radiol. 2006;16:648-60. [ Links ]
4. Dambha F, Tanner J, Carroll N. Diagnostic imaging in Crohns disease: what is the new gold standard. Best Pract Res Clin Gastroenterol. 2014;28:421-36. [ Links ]
5. Liu B, Ramalho M, AlObaidy M, Busireddy KK, Altun E, Kalubowila J, et al. Gastrointestinal imaging-practical magnetic resonance imaging approach. World J Radiol. 2014;6:544-66. [ Links ]
6. Cengic I, Tureli D, Aydin H, Bugdayci O, Imeryuz N, Tuney D. Magnetic resonance enterography in refractory iron deficiency anemia: a pictorial overview. World J Gastroenterol. 2014;20:14004-9. [ Links ]
7. Ladas SD, Triantafyllou K, Spada C, Riccioni ME, Rey JF, Niv Y, et al. European Society of Gastrointestinal Endoscopy (ESGE): recommendations (2009) on clinical use of video capsule endoscopy to investigate small-bowel, esophageal and colonic diseases. Endoscopy. 2010;42:220-7. [ Links ]
8. Kotwal VS, Attar BM, Gupta S, Agarwal R. Should bowel preparation, antifoaming agents, or prokinetics be used before videocapsule endoscopy? A systematic review and meta-analysis. Eur J Gastroenterol Hepatol. 2014;26:137-45. [ Links ]
9. Wu L, Cao Y, Liao C, Huang J, Gao F. Systematic review and meta-analysis of randomized controlled trials of Simethicone for gastrointestinal endoscopic visibility. Scand J Gastroenterol. 2011;46:227-35. [ Links ]
10. Rosa BJ, Barbosa M, Magalhaes J, Rebelo A, Moreira MJ, Cotter J. Oral purgative and simethicone before small bowel capsule endoscopy. World J Gastrointest Endosc. 2013;5:67-73. [ Links ]
11. Cotter J, de Castro FD, Magalhaes J, Moreira MJ, Rosa B. Finding the solution for incomplete small bowel capsule endoscopy. World J Gastrointest Endosc. 2013;5:595-9. [ Links ]
12. Ou G, Shahidi N, Galorport C, Takach O, Lee T, Enns R. Effect of longer battery life on small bowel capsule endoscopy. World J Gastroenterol. 2015;21:2677-82. [ Links ]
13. Dillman JR, Strouse PJ, Ellis JH, Cohan RH, Jan SC. Incidence and severity of acute allergic-like reactions to i v. nonionic iodinated contrast material in children. Am J Roentgenol. 2007;188:1643-7. [ Links ]
14. Wang CL, Cohan RH, Ellis JH, Caoili EM, Wang G, Francis IR. Frequency, outcome, and appropriateness of treatment of nonionic iodinated contrast media reactions. Am J Roentgenol. 2008;191:409-15. [ Links ]
15. Katayama H, Yamaguchi K, Kozuka T, Takashima T, Seez P, Matsuura K. Adverse reactions to ionic and nonionic contrast media. A report from the Japanese Committee on the Safety of Contrast Media. Radiology. 1990;175:621-8. [ Links ]
16. Pannu N, Wiebe N, Tonelli M, Alberta Kidney Disease N. Prophylaxis strategies for contrast-induced nephropathy. JAMA. 2006;295:2765-79. [ Links ]
17. Schild HH, Kuhl CK, Hubner-Steiner U, Bohm I, Speck U. Adverse events after unenhanced and monomeric and dimeric contrast-enhanced CT: a prospective randomized controlled trial. Radiology. 2006;240:56-64. [ Links ]
18. Sodickson A, Baeyens PF, Andriole KP, Prevedello LM, Nawfel RD, Hanson R, et al. Recurrent CT, cumulative radiation exposure,and associated radiation-induced cancer risks from CT of adults. Radiology. 2009;251:175-84. [ Links ]
19. Masselli G, Gualdi G. CT and MR enterography in evaluating small bowel diseases: when to use which modality. Abdom Imaging. 2013;38:249-59. [ Links ]
20. Liao Z, Gao R, Xu C, Li ZS. Indications and detection, completion, and retention rates of small-bowel capsule endoscopy: a systematic review. Gastrointest Endosc. 2010;71:280-6. [ Links ]
21. Committee AT, Wang A, Banerjee S, Barth BA, Bhat YM, Chauhan S, et al. Wireless capsule endoscopy. Gastrointest Endosc. 2013;78:805-15. [ Links ]
22. Gonzalez Carro P, Picazo Yuste J, Fernandez Diez S, Perez Roldan F, Roncero Garcia-Escribano O. Intestinal perforation due to retained wireless capsule endoscope. Endoscopy. 2005;37:684. [ Links ]
23. Tabib S, Fuller C, Daniels J, Lo SK. A symptomatic aspiration of a capsule endoscope. Gastrointest Endosc. 2004;60:845-8. [ Links ]
24. Stanich PP, Kleinman B, Porter KM, Meyer MM. Video capsule endoscopy after bariatric and gastric surgery: oral ingestion is associated with satisfactory completion rate. J Clin Gastroenterol. 2015;49:31-3. [ Links ]
25. Niv E, Fishman S, Kachman H, Arnon R, Dotan I. Sequential capsule endoscopy of the small bowel for follow-up of patients with known Crohns disease. J Crohns Colitis. 2014;8:1616-23. [ Links ]
26. Bandorski D, Holtgen R, Stunder D, Keuchel M. Capsule endoscopy in patients with cardiac pacemakers, implantable cardioverter defibrillators and left heart assist devices. Ann Gastroenterol. 2014;27:3-8. [ Links ]
27. Webb JA, Thomsen HS, Morcos SK, Members of Contrast Media Safety Committee of European Society of Urogenital R. The use of iodinated and gadolinium contrast media during pregnancy and lactation. Eur Radiol. 2005;15:1234-40. [ Links ]
28. Siddiki HA, Fidler JL, Fletcher JG, Burton SS, Huprich JE, Hough DM, et al. Prospective comparison of state-of-the-art MR enterography and CT enterography in small-bowel Crohns disease. Am J Roentgenol. 2009;193:113-21. [ Links ]
29. Tomas C, Soyer P, Dohan A, Dray X, Boudiaf M, Hoeffel C. Update on imaging of Peutz-Jeghers syndrome. World J Gastroenterol. 2014;20:10864-75. [ Links ]
30. Pola S, Santillan C, Levesque BG, Feagan BG, Sandborn WJ. An overview of magnetic resonance enterography for Crohns disease. Dig Dis Sci. 2014;59:2040-9. [ Links ]
31. Mako EK, Mester AR, Tarjan Z, Karlinger K, Toth G. Enteroclysis and spiral CT examination in diagnosis and evaluation of small bowel Crohns disease. Eur J Radiol. 2000;35:168-75. [ Links ]
32. Lee SS, Kim AY, Yang SK, Chung JW, Kim SY, Park SH, et al. Crohn disease of the small bowel: comparison of CT enterography,MR enterography, and small-bowel follow-through as diagnostic techniques. Radiology. 2009;251:751-61. [ Links ]
33. Fletcher JG, Fidler JL, Bruining DH, Huprich JE. New concepts in intestinal imaging for inflammatory bowel diseases. Gastroenterology. 2011;140:1795-806. [ Links ]
34. Dionisio PM, Gurudu SR, Leighton JA, Leontiadis GI, Fleischer DE, Hara AK, et al. Capsule endoscopy has a significantly higher diagnostic yield in patients with suspected and established small-bowel Crohns disease: a meta-analysis. Am J Gastroenterol. 2010;105:1240-8, quiz 9. [ Links ]
35. Jensen MD, Nathan T, Rafaelsen SR, Kjeldsen J. Diagnostic accuracy of capsule endoscopy for small bowel Crohns disease is superior to that of MR enterography or CT enterography. Clin Gastroenterol Hepatol. 2011;9:124-9. [ Links ]
36. Duque G, Almeida N, Figueiredo P, Monsanto P, Lopes S, Freire P, et al. Virtual chromoendoscopy can be a useful software tool in capsule endoscopy. Rev Esp Enferm Dig. 2012;104:231-6. [ Links ]
37. Tukey M, Pleskow D, Legnani P, Cheifetz AS, Moss AC. The utility of capsule endoscopy in patients with suspected Crohns disease. Am J Gastroenterol. 2009;104:2734-9. [ Links ]
38. Leighton JA, Gralnek IM, Cohen SA, Toth E, Cave DR, Wolf DC, et al. Capsule endoscopy is superior to small-bowel follow-through and equivalent to ileocolonoscopy in suspected Crohns disease. Clin Gastroenterol Hepatol. 2014;12:609-15. [ Links ]
39. Flamant M, Trang C, Maillard O, Sacher-Huvelin S, Le Rhun M, Galmiche JP, et al. The prevalence and outcome of jejunal lesions visualized by small bowel capsule endoscopy in Crohns disease. Inflamm Bowel Dis. 2013;19:1390-6. [ Links ]
40. Cotter J, Dias de Castro F, Moreira MJ, Rosa B. Tailoring Crohns disease treatment: the impact of small bowel capsule endoscopy. J Crohns Colitis. 2014;8:1610-5. [ Links ]
41. Niv Y, Ilani S, Levi Z, Hershkowitz M, Niv E, Fireman Z, et al. Validation of the Capsule Endoscopy Crohns Disease Activity Index (CECDAI or Niv score): a multicenter prospective study. Endoscopy. 2012;44:21-6. [ Links ]
42. Rosa B, Moreira MJ, Rebelo A, Cotter J. Lewis Score: a useful clinical tool for patients with suspected Crohns disease submi-ted to capsule endoscopy. J Crohns Colitis. 2012;6:692-7. [ Links ]
43. Cotter J, Dias de Castro F, Magalhaes J, Moreira MJ, Rosa B. Validation of the Lewis score for the evaluation of small-bowel Crohns disease activity. Endoscopy. 2015;47:330-5. [ Links ]
44. Gralnek IM, Defranchis R, Seidman E, Leighton JA, Legnani P, Lewis BS. Development of a capsule endoscopy scoring index for small bowel mucosal inflammatory change. Aliment Pharmacol Ther. 2008;27:146-54. [ Links ]
45. Solem CA, Loftus EV Jr, Fletcher JG, Baron TH, Gostout CJ, Petersen BT, et al. Small-bowel imaging in Crohns disease: a prospective, blinded, 4-way comparison trial. Gastrointest Endosc. 2008;68:255-66. [ Links ]
46. Van Assche G, Dignass A, Panes J, Beaugerie L, Karagiannis J, Allez M, et al. The second European evidence-based consensos on the diagnosis and management of Crohns disease: definitions and diagnosis. J Crohns Colitis. 2010;4:7-27. [ Links ]
47. Pennazio M, Spada C, Eliakim R, Keuchel M, May A, Mulder CJ, et al. Small-bowel capsule endoscopy and device-assisted enteroscopy for diagnosis and treatment of small-bowel disorders: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2015;47:352-86. [ Links ]
48. Annese V, Daperno M, Rutter MD, Amiot A, Bossuyt P, East J, et al. European evidence based consensus for endoscopy in inflammatory bowel disease. J Crohns Colitis. 2013;7:982-1018. [ Links ]
49. Raju GS, Gerson L, Das A, Lewis B. American Gastroenterological A. American Gastroenterological Association (AGA) Institute medical position statement on obscure gastrointestinal bleeding. Gastroenterology. 2007;133:1694-6. [ Links ]
50. Carey EJ, Leighton JA, Heigh RI, Shiff AD, Sharma VK, Post JK, et al. A single-center experience of 260 consecutive patients undergoing capsule endoscopy for obscure gastrointestinal bleeding. Am J Gastroenterol. 2007;102:89-95. [ Links ]
51. Hartmann D, Schmidt H, Bolz G, Schilling D, Kinzel F, Eickhoff A, et al. A prospective two-center study comparing wireless capsule endoscopy with intraoperative enteroscopy in patients with obscure GI bleeding. Gastrointest Endosc. 2005;61:826-32. [ Links ]
52. Mylonaki M, Fritscher-Ravens A, Swain P. Wireless capsule endoscopy: a comparison with push enteroscopy in patients with gastroscopy and colonoscopy negative gastrointestinal bleeding. Gut. 2003;52:1122-6. [ Links ]
53. Teshima CW, Kuipers EJ, van Zanten SV, Mensink PB. Double balloon enteroscopy and capsule endoscopy for obscure gastrointestinal bleeding: an updated meta-analysis. J Gastroenterol Hepatol. 2011;26:796-801. [ Links ]
54. Triester SL, Leighton JA, Leontiadis GI, Fleischer DE, Hara AK, Heigh RI, et al. A meta-analysis of the yield of capsule endoscopy compared to other diagnostic modalities in patients with obscure gastrointestinal bleeding. Am J Gastroenterol. 2005;100:2407-18. [ Links ]
55. Leung WK, Ho SS, Suen BY, Lai LH, Yu S, Ng EK, et al. Capsule endoscopy or angiography in patients with acute overt obscure gastrointestinal bleeding: a prospective randomized study with long-term follow-up. Am J Gastroenterol. 2012;107:1370-6. [ Links ]
56. Katsinelos P, Chatzimavroudis G, Terzoudis S, Patsis I, Fasoulas K, Katsinelos T, et al. Diagnostic yield and clinical impact of capsule endoscopy in obscure gastrointestinal bleeding during routine clinical practice: a single-center experience. Med Princ Pract. 2011;20:60-5. [ Links ]
57. Singh A, Marshall C, Chaudhuri B, Okoli C, Foley A, Person SD, et al. Timing of video capsule endoscopy relative to overt obscure GI bleeding: implications from a retrospective study. Gastrointest Endosc. 2013;77:761-6. [ Links ]
58. Boal Carvalho P, Rosa B, Moreira MJ, Cotter J. New evidence on the impact of antithrombotics in patients submitted to small bowel capsule endoscopy for the evaluation of obscure gastrointestinal bleeding. Gastroenterol Res Pract. 2014;2014:709217. [ Links ]
59. Cotter J, Magalhaes J, de Castro FD, Barbosa M, Carvalho PB, Leite S, et al. Virtual chromoendoscopy in small bowel capsule endoscopy: new light or a cast of shadow? World J Gastrointest Endosc. 2014;6:359-65. [ Links ]
60. Dias de Castro F, Magalhaes J, Boal Carvalho P, Curdia Goncalves T, Rosa B, Moreira MJ, et al. Improving diagnostic yield in obscure gastrointestinal bleeding - how virtual chromoendoscopy may be the answer. Eur J Gastroenterol Hepatol. 2015;27:735-40. [ Links ]
61. Sakai E, Endo H, Kato S, Matsuura T, Tomeno W, Taniguchi L, et al. Capsule endoscopy with flexible spectral imaging color enhancement reduces the bile pigment effect and improves the detectability of small bowel lesions. BMC Gastroenterol. 2012;12:83. [ Links ]
62. Min YW, Kim JS, Jeon SW, Jeen YT, Im JP, Cheung DY, et al. Long-term outcome of capsule endoscopy in obscure gastrointestinal bleeding: a nationwide analysis. Endoscopy. 2014;46:59-65. [ Links ]
63. Curdia Goncalves T, Dias de Castro F, Moreira MJ, Rosa B, Cotter J. Small bowel capsule endoscopy in obscure gastrointestinal bleeding: normalcy is not reassuring. Eur J Gastroenterol Hepatol. 2014;26:927-32. [ Links ]
64. Zhang BL, Jiang LL, Chen CX, Zhong BS, Li YM. Diagnosis of obscure gastrointestinal hemorrhage with capsule endoscopy in combination with multiple-detector computed tomography. J Gastroenterol Hepatol. 2010;25:75-9. [ Links ]
65. Milano A, Balatsinou C, Filippone A, Caldarella MP, Laterza F, Lapenna D, et al. A prospective evaluation of iron deficiency anemia in the GI endoscopy setting: role of standard endoscopy, videocapsule endoscopy, and CT-enteroclysis. Gastrointest Endosc. 2011;73:1002-8. [ Links ]
66. Liu K, Kaffes AJ. Review article: the diagnosis and investigation of obscure gastrointestinal bleeding. Aliment Pharmacol Ther. 2011;34:416-23. [ Links ]
67. Jain TP, Gulati MS, Makharia GK, Bandhu S, Garg PK. CT enteroclysis in the diagnosis of obscure gastrointestinal bleeding: initial results. Clin Radiol. 2007;62:660-7. [ Links ]
68. Huprich JE, Fletcher JG, Fidler JL, Alexander JA, Guimaraes LS,Siddiki HA, et al. Prospective blinded comparison of wireless capsule endoscopy and multiphase CT enterography in obscure gastrointestinal bleeding. Radiology. 2011;260:744-51. [ Links ]
69. Filippone A, Cianci R, Milano A, Pace E, Neri M, Cotroneo AR. Obscure and occult gastrointestinal bleeding: comparison of different imaging modalities. Abdom Imaging. 2012;37:41-52. [ Links ]
70. Wiarda BM, Heine DG, Mensink P, Stolk M, Dees J, Hazenberg HJ, et al. Comparison of magnetic resonance enteroclysis and capsule endoscopy with balloon-assisted enteroscopy in patients with obscure gastrointestinal bleeding. Endoscopy. 2012;44:668-73. [ Links ]
71. Pennazio M, Rondonotti E, de Franchis R. Capsule endoscopy in neoplastic diseases. World J Gastroenterol. 2008;14:5245-53. [ Links ]
72. Urbain D, De Looze D, Demedts I, Louis E, Dewit O, Macken E, et al. Video capsule endoscopy in small-bowel malignancy: a multicenter Belgian study. Endoscopy. 2006;38:408-11. [ Links ]
73. Ross A, Mehdizadeh S, Tokar J, Leighton JA, Kamal A, Chen A, et al. Double balloon enteroscopy detects small bowel mass lesions missed by capsule endoscopy. Dig Dis Sci. 2008;53:2140-3. [ Links ]
74. Hakim FA, Alexander JA, Huprich JE, Grover M, Enders FT. CT-enterography may identify small bowel tumors not detected by capsule endoscopy: eight years experience at Mayo Clinic Rochester. Dig Dis Sci. 2011;56:2914-9. [ Links ]
75. Serrano M, Mao-de-Ferro S, Pinho R, Marcos-Pinto R, Figueiredo P, Ferreira S, et al. Double-balloon enteroscopy in the management of patients with Peutz-Jeghers syndrome: a retrospective cohort multicenter study. Rev Esp Enferm Dig. 2013;105:594-9. [ Links ]
76. Beggs AD, Latchford AR, Vasen HF, Moslein G, Alonso A, Aretz S, et al. Peutz-Jeghers syndrome: a systematic review and recommendations for management. Gut. 2010;59:975-86. [ Links ]
77. Syngal S, Brand RE, Church JM, Giardiello FM, Hampel HL, Burt RW, et al. ACG clinical guideline: genetic testing and management of hereditary gastrointestinal cancer syndromes. Am J Gastroenterol. 2015;110:223-62, quiz 63. [ Links ]
78. Soares J, Lopes L, Vilas Boas G, Pinho C. Wireless capsule endoscopy for evaluation of phenotypic expression of small-bowel polyps in patients with Peutz-Jeghers syndrome and in symptomatic first-degree relatives. Endoscopy. 2004;36:1060-6. [ Links ]
79. Chong AK, Chin BW, Meredith CG. Clinically significant small-bowel pathology identified by double-balloon enteroscopy but missed by capsule endoscopy. Gastrointest Endosc. 2006;64:445-9. [ Links ]
80. Postgate A, Despott E, Burling D, Gupta A, Phillips R, OBeirne J, et al. Significant small-bowel lesions detected by alternative diagnostic modalities after negative capsule endoscopy. Gastrointest Endosc. 2008;68:1209-14. [ Links ]
81. Gupta A, Postgate AJ, Burling D, Ilangovan R, Marshall M, Phillips RK, et al. A prospective study of MR enterography versus capsule endoscopy for the surveillance of adult patients with Peutz-Jeghers syndrome. Am J Roentgenol. 2010;195:108-16. [ Links ]
82. Caspari R, von Falkenhausen M, Krautmacher C, Schild H, Heller J, Sauerbruch T. Comparison of capsule endoscopy and magnetic resonance imaging for the detection of polyps of the small intestine in patients with familial adenomatous polyposis or with Peutz-Jeghers syndrome. Endoscopy. 2004;36:1054-9. [ Links ]
83. Schulmann K, Hollerbach S, Kraus K, Willert J, Vogel T, Moslein G, et al. Feasibility and diagnostic utility of video capsule endoscopy for the detection of small bowel polyps in patients with hereditary polyposis syndromes. Am J Gastroenterol. 2005;100:27-37. [ Links ]
* Corresponding author.
E-mail addresses: pedroboalcarvalho@gmail.com, pedroboalcarvalho@chaa.min-saude.pt (P. Boal Carvalho).
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Confidentiality of data. The authors declare that no patient data appear in this article.
Conflict of interests
The authors declare no conflict of interests.
Received 5 June 2015; accepted 9 July 2015














