Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.23 no.5 Lisboa out. 2016
https://doi.org/10.1016/j.jpge.2015.12.005
IMAGES IN GASTROENTEROLOGY AND HEPATOLOGY
The Lymphoma Hidden in Actinomycosis
O Linfoma Escondido na Actinomicose
Liliana Carneiroa, * , Rute Ferreira a, João Pinto b
a Medicine Department, Hospital Pedro Hispano, Unidade Local de Saúde de Matosinhos, Matosinhos, Portugal
b Pathology Department, Hospital Pedro Hispano, Unidade Local de Saúde de Matosinhos, Matosinhos, Portugal
* Corresponding author.
Keywords: Actinomyces. Actinomycosis. Lymphoma, B-Cell, Marginal Zone. Stomach Neoplasms.
Palavras-chave: Actinomicose. Actinomyces. Linfoma de Zona Marginal Tipo Células B. Neoplasias do Estômago.
1. Case report
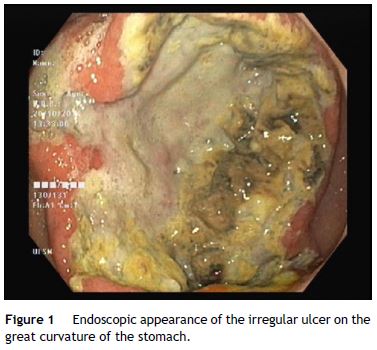
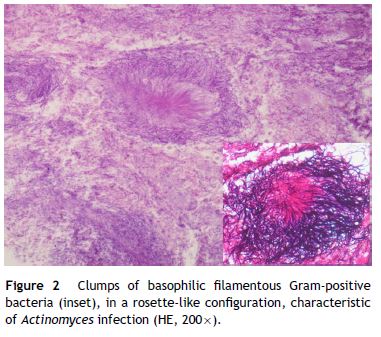
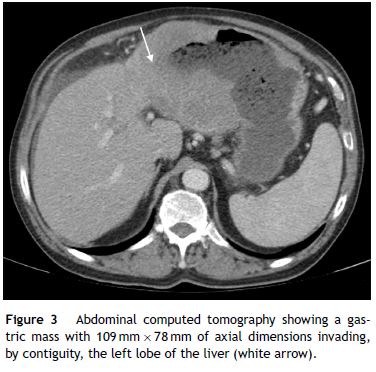
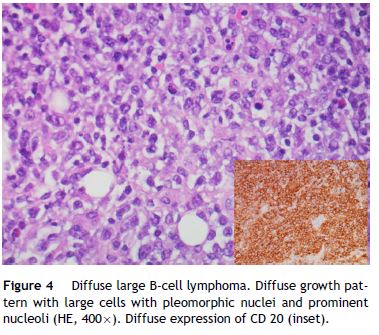
A 62-year-old man with a history of chronic alcoholism (200 g/day) was admitted to our hospital with persistent epigastric pain, anorexia, postprandial fullness, and significant weight loss (10% of body weight) for the previous four months. During hospitalization he presented with hematemesis associated with acute severe normocytic and normochromic anemia (Hb 7.7 g/dL). An upper endoscopy was performed and demonstrated a large ulcerated lesion suggestive of malignancy in the gastric greater curvature (Fig. 1). Endoscopic biopsies revealed numerous filamentous clusters with sulfur granules suggestive of Actinomyces infection, without changes suggesting malignancy (Fig. 2). Abdominal computed tomography revealed an extensive gastric mass and various celiac lymphadenopathies (Fig. 3). The patient was treated with intravenous amoxicillin and clavulanic acid for four weeks, followed by oral treatment for two months. Endoscopic revaluation showed persistence of the previous findings, with repeated isolation of Actinomyces in the tissue biopsy. Given the high suspicion of malignancy and absence of response to therapy, we opted for surgical removal of the lesion. Microscopic examination confirmed the diagnosis of diffuse large B-cell lymphoma (Fig. 4). The patient subsequently started adjuvant chemotherapy, with favorable evolution at six months and complete remission.
2. Discussion
Gastric actinomycosis is a rare clinical condition with only 25 cases reported to date. It is a chronic suppurative infection caused by the anaerobic Gram-positive filamentous bacteria Actinomyces, usually Actinomyces israelii.1,2
The rarity of gastric involvement by actinomycosis has been attributed to the high lumenal acidity of the stomach which inhibits bacterial growth. Predisposing factors such as gastrointestinal tract surgery or trauma, diabetes, lymphoma, extensive mucosal atrophy and medications such proton pump inhibitors facilitate this process.2,3 In the present case, we believe that actinomycosis was facilitated by gastric mucosal damage caused by lymphoma. Due to its propensity to mimic many other diseases including malignancy and the difficulty of obtaining bacteriological evidence, early diagnosis of actinomycosis can be challenging.1,4 In fact, we initially suspected of a non-infectious etiology in our patient such as adenocarcinoma or lymphoma, based on radiologic and endoscopic findings. Although endoscopic diagnosis of gastric actinomycosis is rare with only three cases reported in literature,5 the typical morphology of the bacteria obtained from endoscopic biopsies allowed the diagnosis of actinomycosis in this case. Sulfur granules are strongly suggestive but not pathognomonic of actinomycosis.3,4 Further development with persistence of malignant appearing ulcer despite antimicrobial therapy alerted us, once more, to the possibility of neoplasia. For this reason, we opted for surgical resection of the lesion without previous endoscopic ultrasound-guide biopsies. Open biopsy histology confirmed the diagnosis of diffuse large B-cell lymphoma, the most common type of primary gastric lymphoma (50% of cases). This is an aggressive lymphoma, usually appearing as infiltrating lesions with bizarre ulcerations at endoscopy, as was seen in the present case.
This case outlines the difficulties encountered in the diagnosis of actinomycosis and the indication for open biopsy when actinomycosis does not respond to antimicrobial therapy because of the possibility of concomitant malignancy.
References
1. Acevedo F, Baudrand R, Letelier LM, Gaete P. Actinomycosis: a great pretender. Case reports of unusual presentations and a review of the literature. Int J Infect Dis. 2008;12:358-62. [ Links ]
2. Ercolak V, Paydas S, Ergin M, Ates BT, Duman BB, Gunaldi M, et al. Abdominal actinomycosis with multiple myeloma: a case report. Oncol Lett. 2014;8:1876-8. [ Links ]
3. Wong VK, Turmezei TD, Weston VC. Actinomycosis. BMJ. 2011;343:d6099. [ Links ]
4. Valour F, Sénéchal A, Dupieux C, Karsenty J, Lustig S, Breton P, et al. Actinomycosis: etiology, clinical features, diagnosis, treatment, and management. Infect Drug Resist. 2014;7:183-97. [ Links ]
5. Al-Obaidy K, Alruwaii F, Al Nemer A, Alsulaiman R, Alruwaii Z, Shawarby MA. Primary gastric actinomycosis: report of a case diagnosed in a gastroscopic biopsy. BMC Clin Pathol. 2015;15:2. [ Links ]
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data.The authors declare that no patient data appear in this article.
Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interest
The authors have no conflicts of interest to declare.
* Corresponding author.
E-mail address: liliana.neto.carneiro@gmail.com (L. Carneiro).
Received 29 September, 2015; accepted 14 December 2015














