Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.23 no.6 Lisboa dez. 2016
https://doi.org/10.1016/j.jpge.2016.04.005
ENDOSCOPIC SNAPSHOT
Polidocanol Injection for the Treatment of Rectal Ulcer with Large Vessel After Hemorrhoidal Band Ligation
Injecção de Polidocanol no Tratamento de Úlcera Rectal com Vaso Visível Após Laqueação de Pedículo Hemorroidário
João Santos-Antunes, Armando Peixoto*, Fernando Azevedo, Margarida Marques, Andreia Albuquerque, Guilherme Macedo
Gastroenterology Department, Faculty of Medicine, Centro Hospitalar de São João, Porto, Portugal
* Corresponding author.
Keywords: Hemorrhoids; Hemostatic Techniques; Ligation/methods; Polidocanol; Rectum; Ulcer
Palavras-chave: Hemorróidas; Técnicas Hemostáticas; Ligadura/métodos; Polidocanol; Recto; Úlcera
A 68-year-old male was admitted due to severe rectal bleeding. His past medical history was remarkable for an endoscopic submucosal dissection of a rectal adenoma in 2010 and hemorrhoidal disease, being submitted to two rubber ligations 16 days before. He was not under anticoagulant or antiplatelet therapies. On admission, he was hypotensive (blood pressure 95/45 mmHg), with cardiac rate of 90 bpm. Blood analysis showed a 4 g/dL drop of hemoglobin (14.8–9.8 g/dL). After hemodynamic stabilization, endoscopy was performed, that revealed absence of blood in the rectal lumen, with fecal content of normal coloration. On retroflexion, 2 ulcers were visible. One of them had a large vessel, probably arterial (Fig. 1), that was certainly the origin of the rectal bleeding. Due to the presence of the ulcer, banding was not possible, and the localization was not suitable for hemoclips placement since its proximity to the anal verge. Injection on the vessel or around it was not possible due to the presence of the ulcer. Therefore, a total of 8cc of 1% polidocanol was injected in the submucosa, in the four quadrants of the ulcer (Fig. 2). Patient was discharged 72 h later, with normal blood pressure, bowel transit and no recurrence of rectal bleeding.
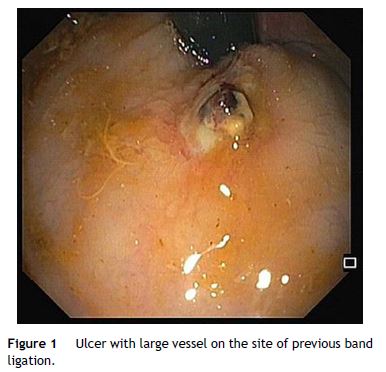
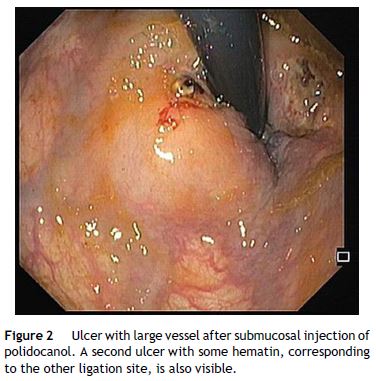
The risk of bleeding after hemorrhoidal band ligation is about 1–2%,1 and it usually occurs immediately after the procedure or 3–10 days, after the rubber band and the ligated tissue fall. The presence of rectal ulcers after banding is rare, and there are a few case reports of massive bleeding in patients taking antiplatelet agents.2 Our patient was not under antiplatelets, and massive rectal bleeding occurred after 16 days. The ulcer consequent to ligation exposed a large vessel, and due to the inability of other more conventional treatments and high risk of bleeding, polidocanol injection around the ulcer was attempted, with an excellent outcome.
References
1. Nelson RS, Ewing BM, Ternent C, Shashidharan M, Blatchford GJ, Thorson AG. Risk of late bleeding following hemorrhoidal banding in patients on antithrombotic prophylaxis. Am J Surg. 2008;196:994-9. [ Links ]
2. Patel S, Shahzad G, Rizvon K, Subramani K, Viswanathan P, Mustacchia P. Rectal ulcers and massive bleeding after hemorrhoidal band ligation while on aspirin. World J Clin Cases. 2014;16:86-9. [ Links ]
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that no patient data appear in this article.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Conflicts of interest
The authors have no conflicts of interest to declare.
* Corresponding author.
E-mail address: armandoafp5@gmail.com (A. Peixoto).
Received 13 February 2016; accepted 3 April 2016














