Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.23 no.6 Lisboa dez. 2016
https://doi.org/10.1016/j.jpge.2016.05.003
IMAGES IN GASTROENTEROLOGY AND HEPATOLOGY
Unusual Endoscopic Removal of a Curious Foreign Body
Remoção Endoscópica Incomum de Corpo Estranho Invulgar
Ana Torres Oliveiraa,*, Nuno Almeidaa, Mónica Martinsb, Carlos Sofiaa
aGastroenterology Department, Centro Hospitalar e Universitário de Coimbra, Coimbra, Portugal
bSurgical Department, Centro Hospitalar e Universitário de Coimbra, Coimbra, Portugal
* Corresponding author.
Keywords: Foreign Bodies; Endoscopy, Gastrointestinal
Palavras-chave: Corpos Estranhos; Endoscopia Gastrointestinal
1. Clinical case
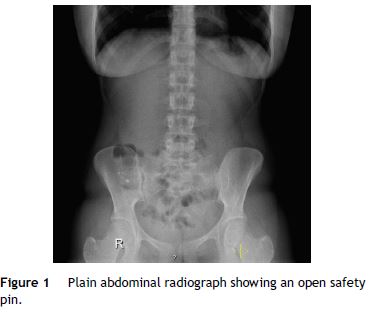
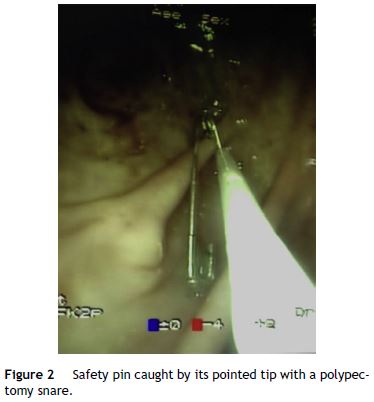
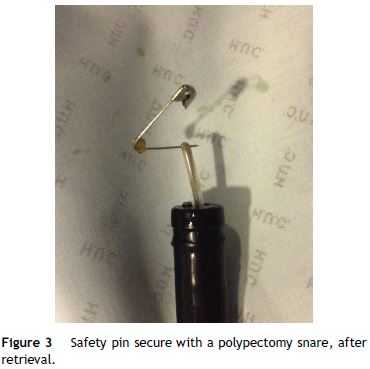
A 19 years-old female patient was admitted to the emergency department after accidental ingestion of a foreign body (safety pin). No relevant past medical history neither concomitant medication was reported. She had no complaints and the physical examination was normal. The abdominal radiograph showed an open safety pin in the upper left quadrant and no signs of pneumoperitoneum. An upper endoscopy with deep duodenal intubation was performed 6 h after ingestion, but the pin was not seen. The patient was admitted to the surgical department for surveillance and remained asymptomatic. She was maintained on a clear liquid diet. At the fifth day of hospitalization and after consecutive abdominal radiographs performed each day, the safety pin was persistently located at the right iliac fossa (Fig. 1). Because of the suspicion that the pin was impacted at the ileocecal valve and after retrograde preparation, a colonoscopy was performed. Adjacent to the valve it was observed a free and open pin that was carefully caught by its pointed tip with a polipectomy snare (SnareMaster Olympus®, 10 mm). Then it was gently removed under direct visualization (Figs. 2–3). The procedure occurred without immediate complications and no evidence of pneumoperitoneum in the control X-ray.
Ingestion of true foreign bodies is common in children and adults with psychiatric disorders. In 80–90% of cases they will pass through the gastrointestinal tract without medical intervention or complications.1 The main complications are obstruction and perforation but these are more common when the objects have sharpen or pointed edges (35%).2 The occurrence of foreign bodies in the cecum is rare due to anatomical strictures present in the digestive tract, such as the pylorus and the ileocecal valve.3 Their presence in the colon occurs generally as a retained rectal foreign body due to self introduction, or in relation with a previously undiagnosed colonic neoplasm.4,5 Endoscopic extraction from the cecum is challenging due to its technical difficulty and probability of perforation. This case demonstrates an unusual technique to remove an open pin from a difficult location of the gastrointestinal tract.
References
1. Frossard JL, Peyer R. An unusual digestive foreign body. Case Rep Gastroenterol. 2011;5:201-5. [ Links ]
2. Somani SK, Ghosh A, Awasthi G. Endoscopic removal of a coin impacted at the ileocecal valve with small bowel obstruction. Trop Gastroenterol. 2009;30:149-50. [ Links ]
3. Macedo JL, Castro EG, Tamura S, Mendes MB. Foreign body of the cecum withdrawn by colonoscopy. Rev Col Bras Cir. 1998;25:61-3. [ Links ]
4. Ponte A, Pinho R, Ribeiro I, Silva J, Rodrigues J, Carvalho J. Impacted foreign body causing acute malignant colonic obstruction. GE Port J Gastroenterol. 2016;23:42-5. [ Links ]
5. Peixoto A, Azevedo F, Macedo G. Unusual retained rectal foreign body. GE Port J Gastroenterol. 2015;22:280-2. [ Links ]
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Conflicts of interest
The authors declare that there is no conflict of interests regarding the publication of this paper.
* Corresponding author.
E-mail address: ana_t_oliveira@hotmail.com (A. T. Oliveira).
Received 7 April 2016; accepted 11 May 2016














