Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.24 no.3 Lisboa jun. 2017
https://doi.org/10.1159/000450900
CLINICAL CASE STUDY
Solitary Rectal Ulcer Syndrome: A Paediatric Case Report
Síndrome da Úlcera Retal Solitária: Relato de um Caso Pediátrico
Marlene Abreua, Raquel Azevedo Alvesa, João Pintob, Miguel Camposc, Sofia Arosoa
aPediatric Department and bDepartment of Pathology, Local Health Unit of Matosinhos, Matosinhos, and cPediatric Surgery Department, São João Hospital Centre, Porto, Portugal
* Corresponding author.
ABSTRACT
Introduction: Solitary rectal ulcer syndrome (SRUS) is an uncommon benign rectal disease. Mostly young adults are affected, and it is rare in paediatric populations. Clinical Case: We present a 12-year-old girl with a 6-month history of tenesmus, frequent defaecation, and bloody stools with mucus. There was no previous history of constipation or other symptoms. At the first visit, physical examination and routine laboratory test results were normal. A stool examination for bacteria and parasites was negative. Colonoscopy revealed a single ulcer in the distal rectum 6 cm from the anal margin. SRUS was confirmed by biopsy. Despite conservative measures, the symptoms persisted. A defaecation proctography showed a small rectocele with no rectal mucosal prolapse. Because of its proximity to the anal sphincter, no surgical intervention was performed. Conclusion: The present case illustrates how difficult the management of SRUS is. Multicentre studies are needed to establish treatment protocols for children.
Keywords: Child; Gastrointestinal haemorrhage; Rectal diseases; Syndrome; Ulcer
RESUMO
Introdução: O Síndrome da Úlcera Retal Solitária (SRUS) é uma doença benigna incomum que afeta predominantemente jovens adultos, sendo rara na população pediátrica. Caso Clínico: Rapariga de 12 anos com história de 6 meses de evolução de tenesmo, aumento da frequência defecatória e retorragias com muco. Sem antecedentes de obstipação ou outras queixas. Na observação inicial, o exame físico e o estudo analítico eram normais. O exame bacteriológico e virológico das fezes foi negativo. A colonoscopia realizada revelou uma úlcera única no reto distal, a 6 cm da margem anal. As biópsias confirmaram o diagnóstico de SRUS. Apesar do tratamento conservador, os sintomas persistiram. A defecografia mostrou um pequeno retocelo, sem prolapso da mucosa. Devido à proximidade com o esfíncter anal, não foi efectuado tratamento cirúrgico. Conclusão: O presente caso ilustra o quão difícil é a abordagem do SRUS. São necessários estudos multicêntricos para estabelecer protocolos de tratamento na idade pediátrica.
Palavras-Chave: Criança; Doenças do recto; Hemorragia gastrointestinal; Síndrome; Úlcera
Introduction
Solitary rectal ulcer syndrome (SRUS) is a rare disorder in children with a benign chronic evolution that is characterized by a combination of symptoms, endoscopic findings, and histological abnormalities [1]. The condition was first described by Cruveilhier in 1830, and detailed clinical and histopathological features were reported by Madigan and Morson in 1969 [see 2–4].
The estimated incidence of SRUS is 1 in 100,000 adults, and the syndrome predominates in young adults. It occurs most commonly in the 3rd decade in men and in the 4th in women, with only a few reported paediatric cases [1, 5, 6]. The aetiopathogenesis of SRUS is not well understood. It is supposed to be due to secondary ischaemia and trauma to the rectal mucosa and paradoxical contraction of the pelvic floor. The excessive straining generates a high intrarectal pressure which pushes the anterior rectal mucosa into the contracting puborectalis muscle, resulting in pressure necrosis of the rectal mucosa. The anterior rectal mucosa is frequently forced into the closed anal canal, causing congestion, oedema, and ulceration [5, 7, 8].
Clinical symptoms include rectal bleeding, mucus discharge, prolonged excessive straining, perineal and lower abdominal pain, tenesmus, feelings of incomplete defaecation, constipation, and, rarely, rectal prolapse [1, 2]. Some children present with apparent diarrhoea [5–7], probably because of prolonged visits to the bathroom [5] and/or frequent passage of mucus [4]. Up to 26% of patients are asymptomatic, and bleeding is discovered incidentally while investigating other diseases [2, 5, 9].
Diagnosis is usually delayed due to clinical variability and symptoms which tend to be similar to those of other rectal diseases such as inflammatory bowel disease, infectious proctocolitis, intussusception, haemorrhoids, or juvenile polyps [2, 3, 5–7]. It is based on a high index of suspicion, combined with typical endoscopic and histological findings. The term SRUS is a misnomer, and is occasionally referred to as the three-lie disease, since the lesion is not always solitary (it may be multiple), is not ulcerative (it may be polypoidal/nodular or affecting the erythematous mucosa only), and is not restricted to the rectum (it may also involve the sigmoid colon) [1, 5–7].
Histological examination is the gold standard for establishing the diagnosis of SRUS. The lamina propria is replaced by smooth muscle and collagen, leading to hypertrophy and disorganization of the muscularis mucosa. These characteristics are also called fibromuscular obliteration [5–7] and are helpful in distinguishing SRUS from Crohn disease, ulcerative colitis, and chronic ischaemic colitis [10, 11].
Until today there has been no other treatment than the use of enemas containing sucralfate, salicylate, corticosteroid, sulphasalazine, mesalazine, and topical fibrin sealant [2, 5]. Surgery is indicated in cases not responding to conservative treatment [7]. The therapeutic experience in children is limited, and it has shown that most therapeutic regimens are inadequate. Therefore, we describe a teenager with an early diagnosis of SRUS and difficult disease management as a way to discuss therapeutic options in paediatric patients.
Clinical Case
A 12-year-old girl, referred by primary medical care, presented with a 6-month history of tenesmus, frequent defaecation and stools, and fresh blood on the stools surface. There was no previous history of constipation, regular laxative use, weight loss, fever, arthralgia, skin rash, abdominal pain, anorexia, or antibiotic use. At the first visit, physical examination (including digital rectal examination) results were normal. Her anthropometric measurements were at the 50th percentile for weight and the 75th percentile for height.
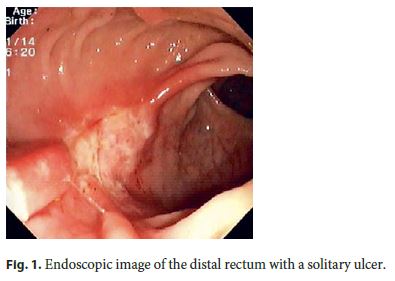
Routine laboratory test results including blood cell counts, coagulation, hepatic function, C-reactive protein levels, and the erythrocyte sedimentation rate were normal. A stool examination for bacteria and parasites was negative, with a normal calprotectin level. Colonoscopy revealed a single ulcer, 20–25 mm in diameter and well delimited, on the anterior rectal wall 6 cm from the anus (Fig. 1). The rest of the colonoscopic examination up to the distal ileum was completely normal, and so was the upper endoscopy performed at the same time.
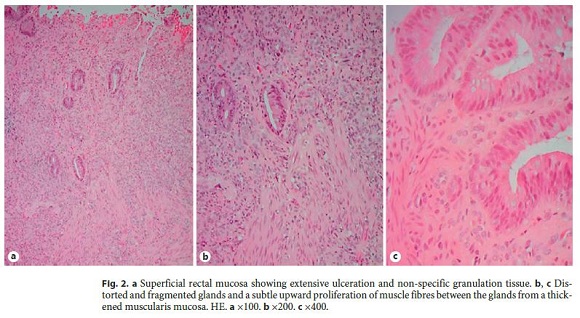
Several biopsies were obtained from both the lesion and the ileal mucosa. A histopathological examination revealed an ulcer with non-specific, inflamed granulation tissue at its base and distorted and fragmented glands. It also showed a subtle upward proliferation of muscle fibres between the glands coming from a thickened muscularis mucosa. The ileal mucosa was normal (Fig. 2). Thus, combining the clinical signs and both the macroscopic and the microscopic findings, we considered a diagnosis of SRUS. An increase in dietary fibre, regular use of laxatives, and sulfasalazine enema were started. The symptoms resolved during the first few months.
Six months later, rectal bleeding was seen in most stools and tenesmus recurred, despite the passage of soft stools. Corticosteroid enemas were tried, with no significant improvement. At that time, 1 year after the diagnosis, colonoscopy was repeated and a single ulcer in the same position persisted, with no other alterations. The examination was completed with dynamic MRI, which showed 2 anterior rectoceles, the largest 10 × 16 mm, with no rectal mucosal prolapse. Despite the administration of oral and topical sulfasalazine during 3 months, the symptoms persisted, with a detrimental impact on daily life. The patient was therefore referred to a paediatric surgeon.
In the paediatric surgery department, the patient underwent defaecation proctography, which showed the small rectocele already known, normal pelvic floor descent during defaecation, complete stool evacuation, and no mucosal prolapse. Rectopexy was therefore not indicated. Excision of the ulcer was not an option either, as it could have caused incontinence due to the ulcers proximity to the anal sphincter. Thus, it was decided not to perform any surgical treatment.
During this last year, our patient still had intermittent bloody stools but experienced no pain and no significant impact on her daily life. The conservative measures were therefore maintained. Until now, there has been no impact on her growth, nor were there any analytical repercussions from the blood loss via defaecation. Endoscopic treatment of the ulcer was also discussed with the patient and her parents, but as there is no sufficient evidence for the utility of any of these techniques, this option was left to be re-discussed in the future.
Discussion
SRUS is a benign rectal disorder of defaecation which is a well-recognized entity in adults but often misdiagnosed or underdiagnosed in children [1, 3, 5–8]. In the literature there are only few case reports, and the largest paediatric series included 22 cases [8]. The youngest reported patient with SRUS was a 1.5-year-old child [5, 8], but the majority of cases are children older than 8 years.
The average time from the onset of symptoms to diagnosis is 5 years, ranging from 1.2 to 5.5 years [1, 5]. Therefore, we highlight the early diagnosis in our patient, made within 7 months only. In fact, high index of suspicion of both a clinician and a pathologist is necessary for early recognition and management of these patients. With this some of the chronic long-term morbidity often associated with this condition may be avoided in adulthood [5, 12].
In our patient, macroscopy revealed a typical ulcerative lesion, described to be present in only 20% of cases as a solitary ulcer [5]. The location and dimension of the ulcer were consistent with descriptions in the literature. In fact, ulcerating lesions are mostly located on the anterior wall of the rectum 5–10 cm from the anal verge; they may range from 0.5 to 4 cm in diameter, but usually are 1–1.5 cm [1, 5, 7].
Although, microscopically, the presence of fibromuscular obliteration of the lamina propria with disorientation of muscle fibres is a pathognomonic finding [2, 3, 5], there are other histological features that can be observed in SRUS, such as thickening of the muscularis mucosa and regenerative changes with distortion of the crypt architecture [5–7]. The 2 latter characteristics, combined with the subtle upward proliferation of muscle fibres between the glands and the absence of other features (such as crypt abscess and granuloma), allowed us to make the diagnosis of SRUS.
Despite being a benign condition in children, morbidity may be significant. Indeed, some symptoms persist over long periods of time – especially bleeding per the rectum, which requires multiple admissions [5, 13]. The initial clinical approach to SRUS in children should be to reassure both the children and the parents about the benign nature of the disease and to suggest conservative measures. These include a high intake of fluids and fibres, laxatives, avoidance of straining at stooling, regulation of toilet habits, and attempts to discuss any psychosocial factors [2, 3, 5]. In most paediatric case series reported, active intervention using enemas and surgical approaches have been used rather than biofeedback therapy, as in adults [5].
Our patient was treated with different conservative measures (diet, laxatives, and enemas of sulfasalazine and corticosteroid), but with little improvement and frequent relapses. In fact, treatments such as with sulfasalazine and corticosteroids – used in inflammatory bowel disease – have been tried in SRUS, but they are suggested only by empirical and non-controlled studies, with varying responses and no knowledge about their long-term benefits [2]. In 1 study, oral salicylate was not effective [14], but considering the unresponsiveness of our patient to the enema treatments, we decided to try that option too. Sucralfate enemas and human fibrin sealant were effective in short studies only [5, 15].
Surgery is indicated in failure of conservative treatment to control severe symptoms such as persistent bleeding. Surgical treatments include rectal prolapse correction, ulcer excision, and, rarely, colostomy [2, 5]. In paediatric patients rectopexy seems to be effective in cases in which rectal prolapse is implicated [3, 8, 16, 17]. Resection proctectomy may be reserved for patients with intractable rectal pain and bleeding who do not respond to other surgical treatments [2]. As our patient did not present with rectal mucosal prolapse, rectopexy was not indicated. Therefore, it was decided to use a conservative approach before a more aggressive surgical option was considered.
Endoscopic techniques have also been used in the treatment of SRUS. Rau et al. [18] reported the use of neodymium-doped yttrium aluminium garnet laser therapy to excise solitary rectal ulcers in the absence of rectal prolapse in 14 cases. Thirteen of the patients (93%) were relieved of their symptoms after a mean of 2.3 sessions of laser treatment, with a mean follow-up of 14.2 months without symptoms (2–25 months). Argon plasma coagulation has been used to treat haemorrhage from SRUS. Somani et al. [19] showed that combined dietary therapy, biofeedback, and argon plasma coagulation allowed bleeding control in 100%, complete healing of ulcers in 75%, and a reduction in ulcer size in the remaining 25% of their patients. Among the 24 patients, paediatric patients were included. Despite promising results with these endoscopic techniques, further trials are required to establish their efficacy and safety for SRUS treatment in a paediatric population.
Although most patients with SRUS in childhood have a satisfactory outcome using simple conservative measures [5, 8], it is difficult to deal with recurrence, as in the case of our patient. Thus, further multicentre studies with larger series of patients and long-term follow-up are required for the establishment of conservative and invasive treatment protocols in paediatric populations.
To our knowledge, this is the second paediatric case report of SRUS in Portugal [20]; thereby we intend to contribute to raising clinicians awareness of this entity, which is often underdiagnosed.
References
1 Zhu QC, Shen RR, Qin HL, Wang Y: Solitary rectal ulcer syndrome: clinical features, pathophysiology, diagnosis and treatment strategies. World J Gastroenterol 2014;20:738–744. [ Links ]
2 Keshtgar AS: Solitary rectal ulcer syndrome in children. Eur J Gastroenterol Hepatol 2008;20:89–92. [ Links ]
3 Ertem D, Acar Y, Karaa EK, Pehlivanoglu E: A rare and often unrecognized cause of hematochezia and tenesmus in childhood: solitary rectal ulcer syndrome. Pediatrics 2002;110:e79. [ Links ]
4 Chiang JM, Changchien CR, Chen JR: Solitary rectal ulcer syndrome: an endoscopic and histological presentation and literature review. Int J Colorectal Dis 2006; 21:348–356. [ Links ]
5 Dehghani SM, Malekpour A, Haghighat M: Solitary rectal ulcer syndrome in children: a literature review. World J Gastroenterol 2012;18:6541–6545. [ Links ]
6 Perito ER, Mileti E, Dalal DH, Cho SJ, Ferrell LD, McCracken M, Heyman MB: Solitary rectal ulcer syndrome in children and adolescents. J Pediatr Gastroenterol Nutr 2012;54:266–270. [ Links ]
7 Urgancı N, Kalyoncu D, Eken KG: Solitary rectal ulcer syndrome in children: a report of six cases. Gut Liver 2013;7:752–755. [ Links ]
8 Suresh N, Ganesh R, Sathiyasekaran M: Solitary rectal ulcer syndrome: a case series. Indian Pediatr 2010;47:1059–1061. [ Links ]
9 Al-Brahim N, Al-Awadhi N, Al-Enezi S, Alsurayei S, Ahmad M: Solitary rectal ulcer syndrome: a clinicopathological study of 13 cases. Saudi J Gastroenterol 2009; 15:188–192. [ Links ]
10 Abid S, Khawaja A, Bhimani SA, Ahmad Z, Hamid S, Jafri W: The clinical, endoscopic and histological spectrum of the solitary rectal ulcer syndrome: a single-center experience of 116 cases. BMC Gastroenterol 2012;12:72. [ Links ]
11 Levine DS: Solitary rectal ulcer syndrome. Are solitary rectal ulcer syndrome and localized colitis cystica profunda analogous syndromes caused by rectal prolapse? Gastroenterology 1987;92:243–253. [ Links ]
12 Blackburn C, McDermott M, Bourke B: Clinical presentation of and outcome for solitary rectal ulcer syndrome in children. J Pediatr Gastroenterol Nutr 2012;54:263–265. [ Links ]
13 Chong VH, Jalihal A: Solitary rectal ulcer syndrome: characteristics, outcomes and predictive profiles for persistent bleeding per rectum. Singapore Med J 2006;47:1063–1068. [ Links ]
14 Felt-Bersma RJ, Cuesta MA: Rectal prolapse, rectal intussusception, rectocele, and solitary rectal ulcer syndrome. Gastroenterol Clin North Am 2001;30:199–222. [ Links ]
15 Zargar SA, Khuroo MS, Mahajan R: Sucralfate retention enemas in solitary rectal ulcer. Dis Colon Rectum 1991;34:455–457. [ Links ]
16 Bonnard A, Mougenot JP, Ferkdadji L, Huot O, Algrain Y, De Lagausie P: Laparoscopic rectopexy for solitary ulcer of rectum syndrome in a child. Surg Endosc 2003; 17:1156–1157. [ Links ]
17 Tweedie DJ, Varma JS: Long-term outcome of laparoscopic mesh rectopexy for solitary rectal ulcer syndrome. Colorectal Dis 2005;7:151–155. [ Links ]
18 Rau BK, Harikrishnan KM, Krishna S: Laser therapy of solitary rectal ulcers: a new concept. Ann Acad Med Singapore 1994;23:27–28. [ Links ]
19 Somani SK, Ghosh A, Avasthi G, Goyal R, Gupta P: Healing of solitary rectal ulcers with multiple sessions of argon plasma coagulation. Dig Endosc 2010;22:107–111. [ Links ]
20 Pereira F: Caso endoscópico. Nascer e Crescer 2008;17:41–42. [ Links ]
Statement of Ethics
This study did not require informed consent or review/approval by the appropriate ethics committee.
Disclosure Statement
The authors have no conflicts of interest to declare.
* Corresponding author.
Dr. Raquel Alves
Serviço de Pediatria, Unidade Local de Saúde de Matosinhos
Rua Dr. Eduardo Torres
PT–4464-513 Senhora da Hora (Portugal)
E-Mail raquelazevedoalves@gmail.com
Received: May 18, 2016; Accepted after revision: September 4, 2016
Acknowledgements
Thanks are due to Teresina Amaro, pathologist, Department of Pathology, and to Carla Cardoso, gastroenterologist, Gastroenterology Unit, Local Health Unit of Matosinhos, Matosinhos, Portugal.














