Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.24 no.4 Lisboa ago. 2017
https://doi.org/10.1159/000452695
CLINICAL CASE STUDY
Splenic Rupture as a Complication of Colonoscopy
Rotura Esplénica Como Complicação da Colonoscopia
Sandra Barbeiroa, Catarina Atalaia-Martinsa, Pedro Marcosa, João Nobreb, Cláudia Gonçalvesa, Cristina Anicetob
Departments of aGastroenterology and bSurgery, Centro Hospitalar de Leiria/Pombal, Leiria, Portugal
* Corresponding author.
ABSTRACT
Splenic rupture is a rare but serious complication after colonoscopy, with high global mortality (5%). Diagnosis requires a high index of suspicion because presentation can be subtle, nonspecific, and delayed from hours to days and then not easily attributed to a recent endoscopy. Urgent splenectomy is the most common treatment option. A 73-year-old woman was admitted to the emergency department 8 h following a diagnostic colonoscopy. She presented abdominal pain and syncope. The diagnosis of splenic rupture was made and a splenectomy was urgently performed. The patients postoperative recovery was uneventful. Splenic rupture is a rare complication of colonoscopy which cannot be underestimated in the differential diagnosis of abdominal pain after this procedure. Splenic injuries may occur in apparently uncomplicated, easy colonoscopies performed by experienced endoscopists, with no risk factors identified, as in this case.
Keywords: Colonoscopy/adverse effects; Splenectomy; Splenic rupture/etiology
RESUMO
A rotura esplénica é uma complicação rara da colonoscopia mas potencialmente fatal, apresentando uma mortalidade global de 5%. O diagnóstico desta entidade requer um alto índice de suspeição uma vez que a apresentação clínica pode ser subtil, inespecífica e com início tardio, horas ou dias após o exame, dificultando a associação dos sintomas a uma possível complicação da colonoscopia recente. A primeira opção terapêutica é a esplenectomia urgente. Apresentamos o caso de uma mulher com 73 anos que foi admitida no serviço de urgência 8 h após a realização de uma colonoscopia por dor abdominal e síncope. O diagnóstico de rotura esplénica foi feito e a doente foi submetida de forma urgente a uma esplenectomia. Não ocorreram intercorrências no período pós-operatório. A rotura esplénica é uma complicação rara da colonoscopia e não deve ser esquecida como um diagnóstico diferencial de dor abdominal com início após a colonoscopia. A rotura esplénica pode ocorrer em colonoscopias aparentemente fáceis, realizadas por gastrenterologistas experientes e em doentes sem fatores de risco identificados, como o caso que se apresenta.
Palavras-Chave: Colonoscopia/efeitos adversos; Esplenectomia; Rotura esplénica/etiologia
Introduction
Colonoscopy is a safe, well-tolerated and low-risk diagnostic and therapeutic procedure [1]. The most frequent complications are bleeding and perforation, with estimated incidences of 1.8–2.5% and 0.34–2.14%, respectively [1]. Splenic rupture is a rare complication, with 103 cases published until the end of 2012 [1]. Its true incidence remains unknown, but some series describe it in 0.0001–0.004% of colonoscopies [1–3]. The real incidence of splenic rupture may probably be higher and the number of published cases clearly reflects underreporting or is due to a bias toward the publication of severe cases [1, 3, 4]. These patients are mainly female (71.5%), have a mean age of 63 years as well as a previous history of abdominal surgery (50.8–65%) [1]. Diagnosis requires a high suspicion because the clinical presentation is unspecific and the timing of the symptoms is variable. Sometimes, the patients complaints begin several days after colonoscopy, hardly being related to it [3, 5].
Due to the elevated morbidity and mortality, it is essential to identify this complication and to treat it as soon as possible [2, 4, 5].
The authors present a case of splenic rupture after colonoscopy in a patient without risk factors for this complication and a review about the management of this complication.
Clinical Case
A 73-year-old female was admitted to the emergency department due to syncope and abdominal pain. Her pain started in the left upper quadrant, gradually becoming constant and diffuse. She had no history of previous abdominal surgery or trauma and was not under any kind of antiplatelet or anticoagulant medication. However, the patient reported being submitted to a colonoscopy 8 h earlier for screening purposes. The colonoscopy was performed by an experienced endoscopist, without sedation and did not involve therapeutic procedures. The intestinal preparation was appropriate and progression towards the cecum was not difficult. The patient had mild discomfort during the insertion time and was discharged with mild abdominal pain after the examination. The time of postcolonoscopy recovery was less than 30 min. On admission, the patient had a pulse of 86 beats/min and a blood pressure of 81/50 mm Hg. Abdomen palpation revealed distension and diffuse tenderness without signs of peritonism. Digital rectal examination was normal. Laboratory analysis demonstrated normal leukocyte and platelet count, hemoglobin of 9.6 g/dL (11.5–16.0 g/dL), INR of 1.04 and C-reactive protein of 246 mg/L (<5.0 mg/L).
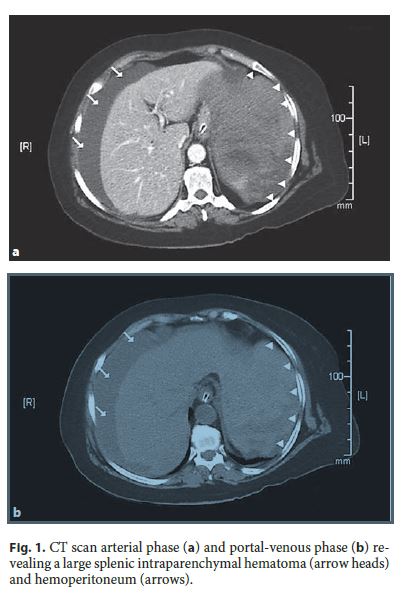
Plain abdomen radiography did not reveal pneumoperitoneum. Abdominal ultrasound demonstrated moderated peritoneal effusion and an echoic, heterogeneous area, occupying the left subphrenic space, suggestive of splenic hematoma. A contrastenhanced abdominal CT scan was performed, revealing a large splenic intraparenchymal hematoma measuring 155 × 106 mm (Spleen Injury Scale, grade III) and moderate hemoperitoneum (Fig. 1).
An urgent laparotomy was undertaken and detected a large splenic laceration, involving the hilus and active bleeding, with approximately 1,000 mL of blood inside the peritoneal cavity. There were neither splenic adhesions nor lesions in the splenic angle of the colon. A total splenectomy was performed and the patient needed blood transfusion in the postoperative period (2 units of packed red blood cells).
The recovery was uneventful and the patient was discharged home on day 13 after admission. Histopathological examination of her spleen revealed no major abnormalities.
Discussion
Splenic rupture is a rare complication of colonoscopy and its pathogenesis is not well clarified. Retrospective data concluded that in the absence of trauma or previous splenic disease, colonoscopy is the most frequent procedure associated with splenic rupture (14.2%) [6]. Three mechanisms were described: direct trauma when the endoscope crosses the splenic angle or when biopsies are taken in this location; rupture of the splenic capsule due to excessive traction on the splenocolic ligament; and rupture of the splenic capsule due to traction of adhesions between the spleen and the colon, which can be a result of prior operations, inflammation or infection [2, 5, 7].
Thus, known risk factors for splenic rupture after colonoscopy are: previous splenic disease or splenomegaly; therapeutic colonoscopy; intra-abdominal adhesions; redundant colon; deep sedation with propofol; oral anticoagulation; and inappropriate intestinal preparation [1, 7]. A review of 77 cases did not associate splenomegaly, anticoagulation and a technically difficult procedure with greater risk [7]. A recent populationbased study concluded that colonoscopy under deep sedation does not increase the risk of splenic rupture [8]. Many of the splenic injuries occurred in apparently uncomplicated, easy colonoscopies performed by experienced endoscopists, and often with no risk factors identified [1, 4]. Left lateral position was considered a protective factor, as the spleen and the splenic angle of the colon approximate in the left side, reducing the excessive traction of the splenocolic ligament or possible adhesions [1, 5].
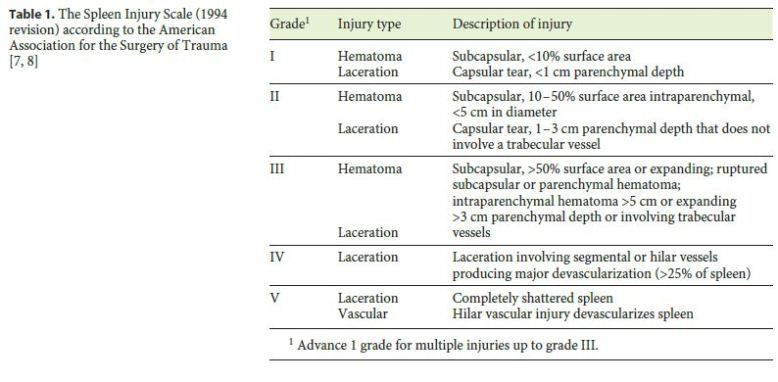
Splenic rupture can be intraparenchymal, subcapsular or with intraperitoneal extension [9]. Lesions can be classified into 5 degrees (I–V) according to the Spleen Injury Scale (organ injury scale of the American Association for the Surgery of Trauma), represented in Table 1 [7, 10]. In its simplified form, lacerations with less than 1 cm are grade I injuries, 1–3 cm are grade II, and more than 3 cm grade III; hilar injuries are grade IV and shattered spleens are grade V [7, 10].
Clinical presentation is unspecific and variable [1, 5]. Abdominal discomfort is common after colonoscopy due to air inflation; some cases of mild splenic rupture can be misdiagnosed as postcolonoscopy discomfort [1, 5]. In most cases, symptoms ensue in the first 24 h after colonoscopy [1, 5]. More rarely, the signs and symptoms of a splenic rupture may be delayed and it must be kept in mind that an interval of up to 8 days between colonoscopy and the beginning of symptoms has been described [9, 11]. The most frequent symptoms are abdominal pain, which can be diffuse or located in the left upper quadrant or referred to the left shoulder (Kehrs sign, 27%) [1, 9].
Less frequently, syncope, hemodynamic instability or hemorrhagic shock can occur [1, 11]. Laboratory tests reveal anemia and leukocitosis [1, 11], but hemoglobin levels can be normal at presentation and do not reflect the real impact of bleeding in the 6–24 h after rupture.
The gold standard diagnostic examination is the contrast-enhanced CT scan of the abdomen, which enables the identification and characterization of splenic and hilar lesions (hematoma, pseudoaneurism, laceration or rupture) and identification of hemoperitoneum [1, 9]. Ultrasound (conventional and contrast-enhanced) is effective in the diagnosis and characterization of splenic injuries. This technique should not be considered as a replacement of CT scan but provides a good alternative in patients with contraindications to CT contrast agents (renal failure or severe allergy) and in hemodynamically compromised patients (focused assessment with sonography for trauma – FAST) [7].
There are 3 therapeutic options: conservative, surgery, or embolization of the splenic artery [7]. Treatment decision depends on the clinical presentation, imaging findings and patients comorbidities. Urgent laparotomy with splenectomy is the most common treatment option [1, 2], recommended when there is active bleeding, hemodynamic instability and/or hemoperitoneum [1, 7]. Splenectomy by laparoscopic approach has been efficiently used in selected patients [1, 5].
Nonoperative management is considered the treatment of choice in hemodynamically stable patients with splenic rupture [11]. This approach included observation alone or those complemented by splenic artery embolization [11].
In some cases of limited subcapsular bleeding, absence of hemoperitoneum and hemodynamic stability, an option for conservative treatment can be taken, with close surveillance, intravenous fluids, antibiotics and blood transfusion support [1, 3, 11]. However, up to 44% of patients initially treated conservatively will eventually need a splenectomy or embolization [7]. Therefore, patients with decreasing systolic blood pressure despite adequate resuscitation measures, transfusion with more than 4 units of packed red blood cells, signs of peritonism or evidence of intra-abdominal hypertension should be submitted to a surgical procedure as soon as possible.
Embolization of the splenic artery, which preserves splenic organ function, is an efficient therapeutic option in hemodynamically stable patients with grade I–IV lacerations and no past history of splenic disease [7, 11].
In spite of what has been previously stated, global mortality after splenic rupture related to colonoscopy is high (5%) [3, 7].
After splenectomy, there is a risk of developing lifethreatening infections due to encapsulated organisms, and the Centers for Disease Control and Prevention recommend immunizations for Streptococcus pneumoniae, Haemophilus influenzae type b, Neisseria meningitides, and influenza [12, 13]. Vaccination should occur at least 2 weeks before the surgery to ensure that an optimal humoral response is achieved. However, in the case of emergent splenectomy, the optimal timing of vaccination after surgery is not clear, but should be performed until 2 weeks after surgery [12, 13].
In our case, we admit that excessive traction of the splenocolic ligament was the most likely cause of rupture since this was a screening colonoscopy in a patient with no previous abdominal surgery or disease and there were no observed splenic adhesions in the surgery. Splenectomy by urgent laparotomy was decided to be the best treatment due to hemodynamic instability and the presence of a grade III spleen injury with hemoperitoneum.
References
1 Piccolo G, Di Vita M, Cavallaro A, Zanghì A, Lo Menzo E, Cardì F, et al: Presentation and management of splenic injury after colonoscopy: a systematic review. Surg Laparosc Endosc Percutan Tech 2014;24:95–102. [ Links ]
2 García-García MJ, Castañera-González R, Martín-Rivas B, Gómez Ruiz M, Rivero Tirado Ml: Splenic rupture after colorectal cancer screening. Rev Esp Enferm Dig 2015;107:705–706. [ Links ]
3 Rex DK: Colonoscopic splenic injury warrants more attention. Gastrointest Endosc 2013;77:941–943. [ Links ]
4 Herreros de Tejada A, Giménez-Alvira L, Van den Brule E, Sánchez-Yuste R, Matallanos P, Blázquez E, et al: Severe splenic rupture after colorectal endoscopic submucosal dissection. World J Gastroenterol 2014;20:9618–9620. [ Links ]
5 Abunnaja S, Panait L, Palesty JA, Macaron S: Laparoscopic splenectomy for traumatic splenic injury after screening colonoscopy. Case Rep Gastroenterol 2012;6:624–628. [ Links ]
6 Aubrey-Bassler FK, Sowers N: 613 cases of splenic rupture without risk factors or previously diagnosed disease: a systematic review. BMC Emerg Med 2012;12:11. [ Links ]
7 Corcillo A, Aellen S, Zingg T, Bize P, Demartines N, Denys A: Endovascular treatment of active splenic bleeding after colonoscopy: a systematic review of the literature. Cardiovasc Intervent Radiol 2013;36:1270–1279. [ Links ]
8 Cooper GS, Kou TD, Rex DK: Complications following colonoscopy with anesthesia assistance: a population-based analysis. JAMA Intern Med 2013;173:551–556. [ Links ]
9 Fishback SJ, Pickhardt PJ, Bhalla S, Menias CO, Congdon RG, Macari M: Delayed presentation of splenic rupture following colonoscopy: clinical and CT findings. Emerg Radiol 2011;18:539–544. [ Links ]
10 Moore EE, Cogbill TH, Jurkovich GJ, Shackford SR, Malangoni MA, Champion HR: Organ injury scaling: spleen and liver (1994 revision). J Trauma 1995;38:323–324. [ Links ]
11 Brennan IM, Faintuch S, Sacks B: Superselective splenic artery embolization for the management of splenic laceration following colonoscopy. Acta Radiol Short Rep 2014;3:2047981614524199. [ Links ]
12 Kealey GP, Dhungel V, Wideroff MJ, Liao J, Choi K, Skeete DA, et al: Patient education and recall regarding postsplenectomy immunizations. J Surg Res 2015;199:580–585. [ Links ]
13 Hammerquist RJ, Messerschmidt KA, Pottebaum AA, Hellwig TR: Vaccinations in asplenic adults. Am J Health Syst Pharm 2016;73:e220–e228. [ Links ]
Disclosure Statement
The authors have no conflicts of interest to declare.
Statement of Ethics
This study did not require informed consent nor approval by the appropriate ethics committee.
* Corresponding author.
Dr. Sandra Barbeiro
Department of Gastroenterology, Centro Hospitalar de Leiria/Pombal
Rua das Olhalvas
PT–2410-197 Leiria (Portugal)
E-Mail sandrabarbeiro@gmail.com
Received: July 13, 2016; Accepted after revision: October 9, 2016














