Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.24 no.4 Lisboa ago. 2017
https://doi.org/10.1159/000452696
CLINICAL CASE STUDY
Mediastinal Mass in a Patient with Colorectal Cancer: A Diagnostic Challenge
Massa Mediastínica em Doente com Cancro Colorretal: Um Desafio Diagnóstico
Cláudio Martinsa, Paula Sousab, Tarcísio Araújoc, Fernando Castro-Poçasc, d, Isabel Pedrotoc, d
aGastroenterology Department, Hospital de São Bernardo, Centro Hospitalar de Setúbal, Setúbal,
bGastroenterology Department, Hospital de São Teotónio, Centro Hospitalar de Tondela/Viseu, Viseu, and
cGastroenterology Department, Hospital Geral de Santo António, Centro Hospitalar do Porto, and
dInstitute of Biomedical Sciences Abel Salazar, University of Porto, Porto, Portugal
* Corresponding author.
ABSTRACT
The differential diagnosis of mediastinal masses involves many benign and malignant conditions, such as lymphadenopathies and cystic lesions. Metastatic mediastinal adenopathies are usually due to lung, esophagus, and stomach cancer and, rarely, due to colorectal cancer. Gastrointestinal duplication cysts are uncommon inherited lesions usually diagnosed during childhood and may involve the esophagus in 20% of cases. In adults, they are usually asymptomatic and diagnosed incidentally. We report the case of a 54-year-old male who recently underwent sigmoidectomy due to an obstructive colon adenocarcinoma. Staging computed tomography scan showed a hypodense lesion in the posterior mediastinum suggestive of metastatic adenopathy. Endoscopic ultrasound revealed a homogeneous and hypoechogenic lesion with intramural location in the upper esophagus, suggestive of a duplication esophageal cyst. Given the oncologic background and to exclude metastatic disease, endoscopic ultrasound-guided fine needle aspiration was performed, and a mucinous fluid was aspirated. The cytologic examination supported the ultrasonographic diagnostic hypothesis. This case highlights the role of endoscopic ultrasound in the differential diagnosis of mediastinal masses, particularly in oncologic patients, in order to rule out more ominous lesions.
Keywords: Endosonography; Esophageal cyst, diagnosis; Colorectal neoplasms; Lymphatic metastasis; Mediastinum
RESUMO
O diagnóstico diferencial das massas mediastínicas inclui diversas patologias benignas e malignas, tais como linfadenopatias e lesões císticas. As adenopatias mediastínicas metastáticas são habitualmente devidas ao cancro do pulmão, esófago e estômago, e mais raramente ao cancro colorretal. Os cistos de duplicação gastrointestinais são lesões congénitas diagnosticadas habitualmente durante a infância e podem envolver o esófago em cerca de 20% dos casos. Nos adultos, são frequentemente assintomáticos e diagnosticadas acidentalmente. Apresentamos o caso de um homem de 54 anos recentemente submetido a sigmoidectomia por adenocarcinoma estenosante do sigmóide. A tomografia computorizada de estadiamento mostrou uma lesão hipodensa no mediastino posterior, sugestiva de adenopatia metastática. A ultrassonografia endoscópica revelou uma lesão homogénea e hipoecogénica na dependência da parede do esófago torácico, sugestiva de um cisto de duplicação esofágico. Dado o contexto oncológico e para excluir doença metastática, foi realizada punção aspirativa com agulha fina tendo-se aspirado um fluido mucinoso. O exame citológico confirmou a hipótese diagnóstica ultrassonográfica. Este caso destaca o papel da ultrassonografia endoscópica no diagnóstico diferencial das massas mediastínicas, particularmente em doentes oncológicos, no sentido de excluir lesões mais graves.
Palavras-Chave: Endossonografia; Mediastino; Metástase linfática;·Neoplasias colorrectais; Quisto esofágico
Introduction
The differential diagnosis of mediastinal masses is wide and management of individual cases can be challenging. The location and composition of the lesions are critical to narrowing the diagnosis. The most common lesions in the posterior mediastinum are lymphadenopathies, neurogenic tumors, and cystic lesions.
There are a few reports of solitary metastatic mediastinal lymph node of colorectal cancer (CRC) without any other organ involvement [1, 2]. Posterior mediastinal cystic lesions represent 15–20% of all primary posterior mediastinal masses and include bronchogenic, pericardial, neuroenteric, and duplication esophageal cysts (DEC) [3].
Gastrointestinal duplication cysts are rare congenital malformations that arise during early embryonic development. Most of them are found in the small bowel (44%), the esophagus (20%), or in the large bowel (15%) [4]. They are usually attached to the gastrointestinal tract, are lined by gastrointestinal epithelium (squamous epithelium in DEC), have smooth muscle cells in the wall, and contain a mucoid fluid.
The majority of DEC are diagnosed during childhood and are found in the lower third of the posterior mediastinum. In adults, the cysts are usually asymptomatic and typically discovered incidentally on endoscopy or radiologic imaging. The symptoms of esophageal cyst are caused by compression or displacement of surrounding mediastinal structures. The diagnosis of a DEC can usually be made based on the endoscopic and endosonographic characteristics. Endoscopic ultrasound (EUS)-guided fine needle aspiration (FNA) has been used to establish a diagnosis despite an infection risk as high as 14% reported in the literature [5].
Clinical Case
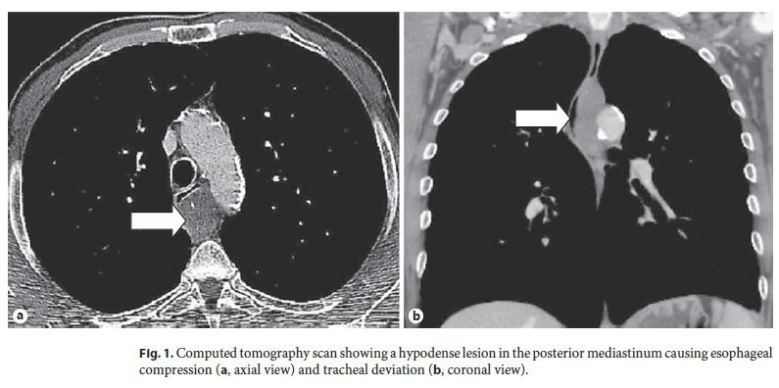
We present a 54-year-old Caucasian male who recently underwent sigmoidectomy due to obstructive sigmoid colon neoplasia and whose histology revealed a moderately differentiated adenocarcinoma, stage pT3N1a. During the preoperative staging, a thoracoabdominopelvic computed tomography (CT) scan was performed, revealing a hypodense lesion in the posterior mediastinum measuring 6 cm of greater diameter and causing esophageal compression and tracheal deviation (Fig. 1). A probable diagnosis of mediastinal metastatic adenopathy was made. His past medical history was unremarkable and he reported no history of upper gastrointestinal or respiratory symptoms.
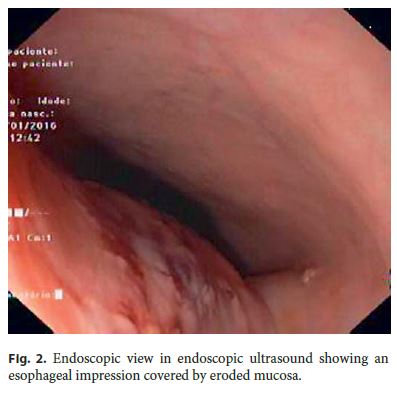
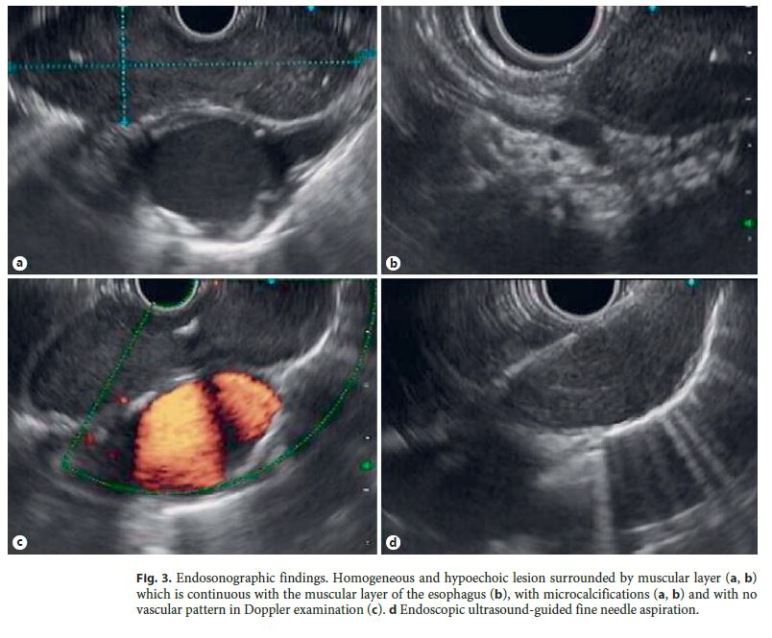
In order to clarify the nature of the referred lesion, an upper EUS was performed. In the endoscopic view, an esophageal impression, between 22 and 27 cm from the incisor teeth, covered by eroded mucosa, was evident (Fig. 2). EUS showed a homogeneous and hypoechogenic lesion, measuring 70 by 30 mm, in the dependence of the esophageal wall and surrounded by muscular layer (Fig. 3a, b). This lesion contained focal microcalcifications and showed no vascular pattern on Doppler examination (Fig. 3c). Given the oncologic context and to exclude metastatic disease, EUS-guided FNA was performed with a 22-gauge needle (Fig. 3d) under antibiotic prophylaxis (intravenous infusion of 200 mg ciprofloxacin pre-procedure followed by oral 500 mg ciprofloxacin q12h for 5 days). A mucinous fluid was aspirated. The ultrasonographic appearance was suggestive of a DEC and the cytology revealed clusters of squamous cells with no atypia compatible with this diagnosis. The case was discussed with a multidisciplinary team and, as the patient remained asymptomatic, it was decided to schedule him for follow-up EUS within 1 year.
Discussion
CRC is the second most common type of cancer in females and the third in males, worldwide. The most prevalent sites of metastasis are liver, lung, bone, and brain [6]. Mediastinal involvement in CRC is usually seen in patients with previous liver or lung metastasis. Direct colon metastasis to the mediastinal lymph nodes without any other organ involvement has been reported in only two single case reports. In both cases, CT scan revealed pathological mediastinal adenopathies. In the case reported by El-Halabi et al. [1], the definitive diagnosis was made by EUS-guided FNA, which revealed multiple, enlarged, rounded, homogeneous, and hypoechogenic subcarinal lymph nodes. Musallam et al. [2] presented a patient with solitary enlarged right paratracheal lymph node, positive on fluor-18-deoxyglucose positron emission tomography scan, who underwent mediastinoscopic biopsy, which revealed metastatic adenocarcinoma. We reported a case of a patient with CRC whose staging CT scan revealed a probable metastatic mediastinal adenopathy.
DEC have been estimated to occur in 1 out of 8,000 live births and 80% are diagnosed during childhood. Lower intrathoracic esophagus is the most common location and normally they are found on the right side due to the dextrorotation of the stomach during embryogenesis. DEC can be tubular or cystic and 80% of them do not communicate with the lumen; the others run parallel to and communicate with the esophageal lumen.
The majority of DEC become symptomatic during childhood and will be removed for that reason. As a consequence, these types of cysts are rarely seen in adults. If they are found during adulthood, they are usually asymptomatic and most reports are, therefore, based on an incidental finding during endoscopic or radiological procedures. Because of compression of adjacent structures, they can cause dysphagia (70%), epigastric or retrosternal pain (30%), and respiratory symptoms [7]. Uncommonly, DEC can complicate with gastrointestinal bleeding, perforation, and infection. Malignant degeneration is very rare. Traditionally, in asymptomatic adult patients, the diagnosis is suspected during endoscopy, which shows an esophageal submucosal lesion, or based on CT scan, which reveals a homogeneous hypodense lesion with regular margins originating from the esophagus, as found in the present case. EUS plays an important role in the evaluation of mediastinal masses and helps distinguish solid from cystic lesions. EUS usually reveals an anechoic homogeneous lesion with smooth margins in the submucosal wall, surrounded by a muscular layer which is continuous with the muscularis propria of the esophagus. The presence of peristalsis and the ciliary tufts inside are highly specific features of a duplication cyst, while the presence of cartilage in the wall favors the diagnosis of a bronchogenic cyst. It is important to consider the possibility of a DEC even in patients with hypoechoic lesions as in our case because the presence of pus, blood, or thick contents may modify the EUS features and result in confusion with other soft-tissue lesions like stromal tumors and malignant adenopathies. In the present case, although we noted a well-defined wall structure supporting a benign condition, the nature of the content resulted in a high attenuation on CT scan, causing doubts in the diagnosis. Therefore, when there is concern about more serious lesions or if the nature of the lesion is in doubt, EUS provides a gold opportunity to perform FNA to get material for cytology. The risk of cyst infection should be taken into account when EUS-guided FNA is performed despite the use of pre- and post-procedure prophylactic antibiotics [8]. Araújo et al. [9] studied eight patients with DEC who underwent EUS-guided FNA under antibiotic prophylaxis and no infectious complications were reported.
In this case, the patient underwent EUS and the ultrasonographic features were suggestive of a DEC. However, given the neoplastic history and the diagnostic hypothesis of metastatic adenopathy, EUS-FNA was performed. The cytology supported the diagnosis of a DEC.
Once the diagnosis of DEC is established, treatment depends on the presence of symptoms. Surgical resection is generally required for symptomatic cysts. Some reports of endoscopic management of duplication cysts are available. Endoscopic fenestration of noncommunicating cyst has been successfully done and a step-by-step incision of the septum between the esophageal lumen and the communicating DEC has also been reported [10]. Treatment of asymptomatic DEC is controversial with no clear guidelines. While some authors advocate for resection due to possible malignant degeneration, others have advocated for observation. Since there have been case reports of stable DEC on EUS surveillance, this may be a suitable method of outpatient follow-up. As our patient remained asymptomatic, we decided to schedule him for EUS surveillance within a year.
In conclusion, this report describes an uncommon entity in an adult patient, highlighting the challenge in the differential diagnosis of mediastinal lesions and the role of EUS in this process. We aim to alert clinicians to consider DEC in the differential diagnosis of a mediastinal mass. The question of whether or not to perform EUSguided FNA on a lesion suspected of being a DEC is controversial as these lesions can become infected, although this procedure is often required to obtain a definitive diagnosis and to rule out more ominous lesions.
References
1 El-Halabi MM, Chaaban SA, Meouchy J, Page S, Salyers WJ: Colon cancer metastasis lymph nodes without liver and lung involvement: a case report. Oncol Lett 2014;8:2221–2224. [ Links ]
2 Musallam KM, Taher AT, Tawil AN, Chackenchiro ZI, Halbal MZ, Shamseddine AI: Solitary mediastinal lymph node metastasis in rectosigmoid carcinoma: a case report. Cases J 2008;1:69. [ Links ]
3 Jeung MY, Gasser B, Gangi A, Bogorin A, Charneau D, Wihlm JM, et al: Imaging of cystic masses of the mediastinum. Radiographics 2002;22:79–93. [ Links ]
4 Pujar VC, Kurbet S, Kaltari DK: Laparoscopic excision of intra-abdominal oesophageal duplication cyst in a child. J Minim Access Surg 2013;9:34–36. [ Links ]
5 Roy L, Adler G: Duplication cysts: diagnosis, management, and the role of endoscopic ultrasound. Endosc Ultrasound 2014;3:152–160. [ Links ]
6 Hess KR, Varachachary GR, Taylor SH, Wei W, Raber MN, Lenzi R, et al: Metastatic patterns in adenocarcinoma. Cancer 2006;106:1624–1633. [ Links ]
7 Cioffi U, Bonavina L, De Simone M, Santambrogio L, Pavoni G, Testori A, et al: Presentation and surgical management of bronchogenic and esophageal duplication cysts in adults. Chest 1998;113:1492–1496. [ Links ]
8 Trojan J, Mousset S, Caspary WF, Hoepffner N: An infected esophageal duplication cyst in a patient with non-Hodgkins lymphoma mimicking persistent disease. Dis Esophagus 2005;18:287–289. [ Links ]
9 Araújo T, Castro-Poças F, Magalhães MJ, Pedroto I: Punção aspirativa guiada por ecoendoscopia em lesões císticas da parede esofágica. Available at: http://www.sociedadesmedicas.pt/semanadigestiva/lista_artigos.asp?Pag=106&Crit=1&VR=424. [ Links ]
10 Will U, Meyer F, Bosseckert H: Successful endoscopic treatment of an esophageal duplication cyst. Scand J Gastroenterol 2005;40:995–999. [ Links ]
Statement of Ethics
The authors declare that no experiments were performed on humans or animals for this study. The authors declare that they have followed the protocols of their work center on the publication of patient data. The authors have obtained written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Disclosure Statement
The authors have no conflict of interests to declare.
* Corresponding author.
Dr. Cláudio Martins
Gastroenterology Department, Hospital de São Bernardo
Rua Camilo Castelo Branco
PT–2910-446 Setúbal (Portugal)
E-Mail cmartins1@campus.ul.pt
Received: August 16, 2016; Accepted after revision: October 10, 2016














