Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.24 no.5 Lisboa out. 2017
https://doi.org/10.1159/000455155
IMAGES IN GASTROENTEROLOGY AND HEPATOLOGY
Spontaneous Recurrent Pneumoperitoneum in Systemic Sclerosis
Pneumoperitoneu Espontâneo Recorrente na Esclerodermia
Sandra Barbeiro, Catarina Atalaia-Martins, Cláudia Gonçalves
Department of Gastroenterology, Centro Hospitalar de Leiria, Leiria, Portugal
* Corresponding author.
Keywords: Recurrent pneumoperitoneum; Systemic sclerosis; Abdominal distention; Constipation
Palavras-Chave: Pneumoperitoneu recorrente; Esclerodermia; Distensão abdominal; Obstipação
Case Report
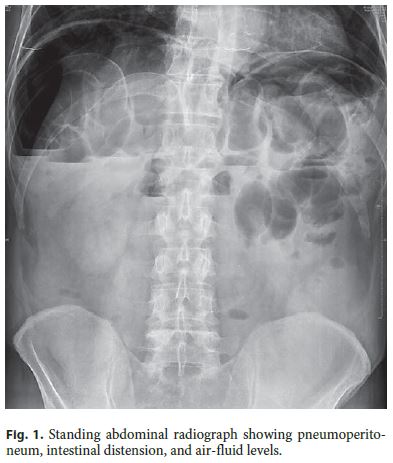
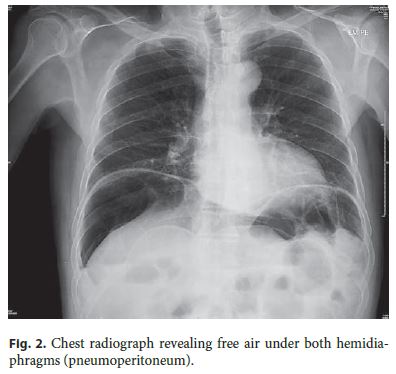
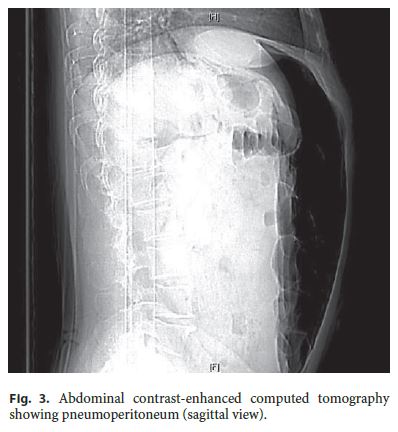
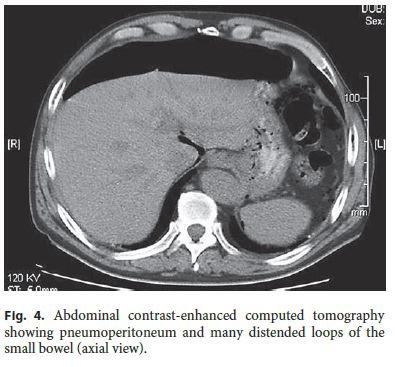
A 72-year-old male presented with intermittent painful abdominal distension and constipation. He explained that the symptoms occurred during the past 2 years, with variable intervals (>4 episodes per year) characterized by diffuse abdominal pain, abdominal distention, vomiting, and diarrhea, followed by constipation; these episodes had variable duration, between 5 and 15 days, and resolved spontaneously. The patient denied dysphagia, fecaloid vomiting, weight loss, or hemorrhage. Recent upper gastrointestinal endoscopy and ileocolonoscopy were normal. His past medical history included systemic sclerosis diagnosed at 56 years of age and treated with methotrexate for the past 7 years with improvement of cutaneous and articular symptoms and an exploratory laparotomy when he was 71 years old due to pneumoperitoneum with no identifiable cause. Other regular medications, smoking, or alcohol consumption were also denied. Family history was irrelevant. On admission, the patient was stable and without fever; the abdomen was markedly distended, with decreased bowel sounds, diffuse tympanism, and tenderness but without peritoneal signs. Blood tests showed no significant abnormalities. Standing chest and abdominal radiographs revealed free air under both hemidiaphragms, distension of the small and large intestine, and air-fluid levels (Fig. 1, 2). Abdominal and pelvic contrast-enhanced computed tomography confirmed the presence of pneumoperitoneum and showed many distended loops of the small bowel, but no cause of the free air was identified (Fig. 3, 4).
The patients general condition was stable, and antibiotics, analgesics, and promotility agents were started. Despite the absence of other causes and due to the chronic presentation, pneumoperitoneum was considered a manifestation of systemic sclerosis. The patient was discharged on day 7 with symptomatic medication (butylscopolamine, domperidone, and simethicone).
Six months later, abdominopelvic computed tomography was repeated and revealed a smaller pneumoperitoneum and the presence of small air bubbles in the colonic wall; no obstructive lesion was identified. The symptoms improved with oral medication. One year later, magnetic resonance enterocolonography showed mild pneumoperitoneum, normal contrast progression, and distension of the small intestine; there were no stenotic lesions, fistulas, or contrast extravasation into the pneumoperitoneum. At outpatient follow-up 24 months later, the patient had recurrent mild abdominal distension but remained clinically well. In this case, the most suitable cause of the nonsurgical recurrent pneumoperitoneum was systemic sclerosis.
Discussion
Pneumoperitoneum is often caused by visceral perforation, with symptoms of peritonitis, and requires an emergent surgical intervention [1]. Nonsurgical spontaneous pneumoperitoneum is a rare entity not associated with organ perforation and usually treated conservatively [1, 2].
Nonsurgical pneumoperitoneum is associated with postoperatively retained air, ventilatory support, spontaneous rupture of pulmonary blebs, cardiopulmonary resuscitation, endoscopy, diverticulosis, pneumatosis cystoides intestinalis, pneumocholecystitis, collagen vascular diseases, gynecologic causes, iatrogenic, and idiopathic causes [2]. In our case, systemic sclerosis was the apparent etiology [1, 3]. There are few reports of chronic scleroderma-related pneumoperitoneum [1–3]. The excessive fibrosis, inflammation, and vascular dysfunction characteristic of systemic sclerosis can affect any site within the gastrointestinal tract [1]. In the small intestine, it causes hypomotility, pseudo-obstructions, and luminal distension [1]. Nevertheless, the pathogenesis of this condition is uncertain, and treatment is usually supportive (promotility and probiotic agents, laxatives, and rifaximin) [1].
Most patients with nonsurgical pneumoperitoneum have clinical clues or associated conditions that may indicate the possibility of this diagnosis. When signs of peritoneal irritation, fever, and leukocytosis are absent, nonsurgical causes of pneumoperitoneum should be considered, and conservative management with supportive care and careful observation is indicated [1–3]. Thus, recognized, nonsurgical pneumoperitoneum allows avoidance of an unnecessary laparotomy and its associated morbidity [1–3].
References
1 ONeill SB, McLaughlin PD, Kelly D, Quigley E, Maher MM: Chronic pneumoperitoneum in systemic sclerosis. Can Assoc Radiol J 2013;64:154–155. [ Links ]
2 Mularski RA, Ciccolo ML, Rappaport WD: Nonsurgical causes of pneumoperitoneum. West J Med 1999;170:41–46. [ Links ]
3 London NJM, Bailey RG, Hall AW: Spontaneous benign pneumoperitoneum complicating scleroderma in the absence of pneumatosis cystoides intestinalis. Postgrad Med J 1990;66:61–62. [ Links ]
Statement of Ethics
This study did not require informed consent or review/approval by the appropriate ethics committee.
Disclosure Statement
The authors have no conflicts of interest to declare.
* Corresponding author.
Dr. Sandra Barbeiro
Department of Gastroenterology, Centro Hospitalar de Leiria
Rua das Olhalvas
PT–2410-197 Leiria (Portugal)
E-Mail sandrabarbeiro@gmail.com
Received: October 10, 2016; Accepted after revision: December 7, 2016














