Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.24 no.5 Lisboa out. 2017
https://doi.org/10.1159/000478941
ENDOSCOPIC SNAPSHOT
Elastography and Contrast-Enhanced Endoscopic Ultrasound Findings in a Pseudo-Solid Variant of a Pancreatic Serous Cystadenoma
Achados em Ecoendoscopia com Elastografia e Contraste na Variante Pseudo-Sólida do Cistadenoma Seroso do Pâncreas
Joana Carmoa, Pedro Moutinho-Ribeirob, Miguel Bispoa, Cristina Chagasa
aDepartment of Gastroenterology, Hospital de Egas Moniz, Centro Hospitalar de Lisboa Ocidental, Lisbon, and
bDepartment of Gastroenterology, Centro Hospitalar de São João, Porto, Portugal
* Corresponding author.
Keywords: Endoscopic ultrasonography; Elastography;·Contrast-enhanced endoscopic ultrasonography;·Pancreatic cysts; Serous cystadenoma
Palavras-Chave: Ecoendoscopia; Elastografia; Ecoendoscopia com contraste; Lesões quísticas do pâncreas; Cistadenoma seroso
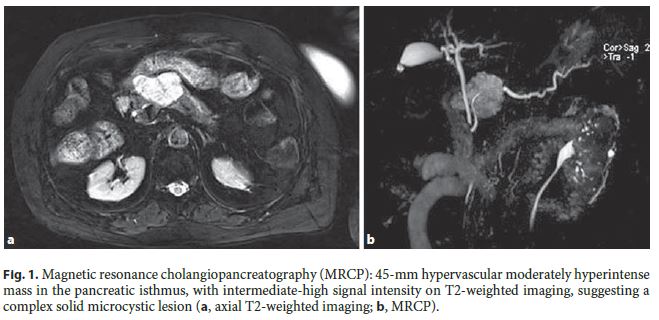
An 80-year-old female was referred to the Gastroenterology Department due to a 40-mm solid mass in the pancreatic isthmus, incidentally found on a computed tomography (CT) scan. Her past medical history was significant for hypertension and coronary artery disease. Magnetic resonance cholangiopancreatography (MRCP), performed 4 months after the CT, showed a 45-mm hypervascular mass in the pancreatic isthmus, with intermediate-high signal intensity on T2-weighted images, suggesting a complex solid microcystic lesion (Fig. 1).
Endoscopic ultrasound (EUS) showed a well-circumscribed, 45-mm, predominantly hypoechogenic complex mass in the pancreatic isthmus, with scattered cystic areas. EUS-guided fine-needle aspiration with a 25-gauge needle was performed (3 passes) and cytology was suspicious, although not definitive, for malignancy. In a multidisciplinary team meeting, surveillance was decided based on MRCP/EUS morphologic findings, compatible with a pseudo-solid variant of a serous cystadenoma (SCA) and equivocal findings for malignancy on cytology, besides the location of the lesion (pancreatic isthmus) and the patients age and comorbidities. EUS was repeated 12 months later, with stable morphologic findings. Additional evaluation with Doppler-EUS showed increased color-Doppler signal (Fig. 2a), real-time elastography presented a soft pattern (strain ratio 3.1) (Fig. 2b) and, in the dynamic study with contrast (Sonovue ® ), the pseudosolid areas presented intense enhancement with slow washout (Fig. 2c). No suspicious lymph nodes were found.
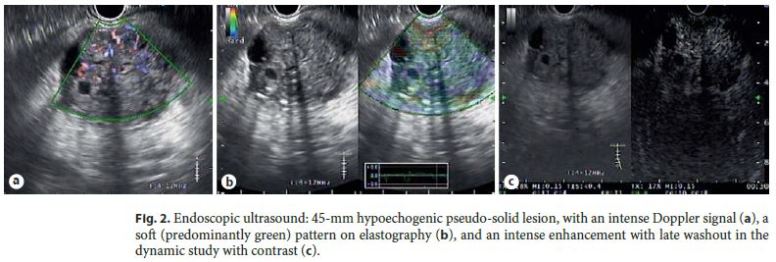
The differential diagnosis of complex pancreatic lesions is often challenging, and EUS morphology alone cannot provide a diagnosis in the majority of cases. EUS-guided fine-needle aspiration, EUS real-time elastography (EUS-E), and contrast-enhanced EUS (CE-EUS) can add valuable information and prevent unnecessary surgeries. Serous cystic neoplasms comprise 1–2% of pancreatic neoplasms and 10–15% of pancreatic cystic lesions [1]. SCA can be classified into 4 morphologic patterns: microcystic (which comprises more than half of the cases), macrocystic (30%), mixed (11%), and solid, resulting from the coalescence of multiple 1- to 2-mm cysts (7%) [2]. SCA has a very low risk of malignant transformation: size >10 cm and head location are independently associated with aggressive behaviour [3]. Thus, in patients with suspected SCA, surgical resection should be considered (1) when differentiation from other neoplasms cannot be assured; (2) the patient is symptomatic; and (3) when the tumor is rapidly increasing in size (with no defined cutoff value, taking into account that reported growth rates for SCA range from 1 to 6 mm/year) [2–5]. The differential diagnosis between the solid variant of SCA and other solid pancreatic neoplasms, including adenocarcinoma and neuroendocrine tumors, is crucial. Both pancreatic adenocarcinoma and neuroendocrine tumors typically present a hard pattern on EUS-E, whilst neuroendocrine tumors are typically hyperenhanced lesions with rapid washout on CE-EUS and adenocarcinoma is typically a hypoenhanced mass [6, 7]. On CE-EUS, SCA has hyperenhancement in 86% of the cases, with slow washout in 78% [8]. The pseudo-solid variant of SCA is a rare lesion, and this case emphasizes the relevance of EUS-E and CEEUS in the differential diagnosis of this challenging pancreatic lesion.
References
1 Horvath KD, Chabot JA: An aggressive resectional approach to cystic neoplasms of the pancreas. Am J Surg 1999;178:269–274. [ Links ]
2 Kimura W, Moriya T, Hanada K, Abe H, Yanagisawa A, Fukushima N, Ohike N, et al: Multicenter study of serous cystic neoplasm of the Japan Pancreas Society. Pancreas 2012;41:380–387. [ Links ]
3 Khashab MA, Shin EJ, Amateau S, Canto MI, Hruban RH, Fishman EK, Cameron JL, et al: Tumor size and location correlate with behaviour of pancreatic serous cystic neoplasms. Am J Gastroenterol 2011;106:1521–1526. [ Links ]
4 van der Waaij LA, van Dullemen HM, Porte RJ: Cyst fluid analysis in the differential diagnosis of pancreatic cystic lesions: a pooled analysis. Gastrointest Endosc 2005;62:383–389. [ Links ]
5 Malleo G, Bassi C, Rossini R, Manfredi R, Butturini G, Massignani M, Paini M, et al: Growth pattern of serous cystic neoplasms of the pancreas: observational study with long-term magnetic resonance surveillance and recommendations for treatment. Gut 2012;61:746–751. [ Links ]
6 Andrada Seicean A, Mosteanu O, Seicean R: Maximizing the endosonography: The role of contrast harmonics, elastography and confocal endomicroscopy. World J Gastroenterol 2017;23:25–41. [ Links ]
7 Iglesias-García J, Lariño-Noia J, Abdulkader I, Forteza J, Dominguez-Muñoz E: Quantitative endoscopic ultrasound elastography: an accurate method for the differentiation of solid pancreatic masses. Gastroenterology 2010;139:1172–1180. [ Links ]
8 Fusaroli P, Serrani M, de Giorgio R, DErcole MC, Ceroni L, Lisotti A, Caletti G: Contrast harmonic-endoscopic ultrasound is useful to identify neoplastic features of pancreatic cysts (with videos). Pancreas 2016;45:265–268. [ Links ]
Statement of Ethics
This study did not require informed consent or review/approval by the appropriate ethics committee.
Disclosure Statement
The authors have no conflicts of interest to declare.
* Corresponding author.
Dr. Joana Carmo
Gastroenterology Department, Hospital de Egas Moniz
Centro Hospitalar Lisboa Ocidental
Rua da Junqueira n° 126, PT–1349-019 Lisbon (Portugal)
E-Mail joanavcarmo@gmail.com
Received: February 21, 2017; Accepted after revision: May 12, 2017














