Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.25 no.1 Lisboa fev. 2018
https://doi.org/10.1159/000478988
ORIGINAL ARTICLE
Acute-on-Chronic Liver Failure: A Portuguese Single-Center Reference Review
Doença Hepática Crónica Agudizada: Revisão da Experiência de um Centro Português de Referenciação
Miguel Verdelhoa, Rui Perdigotob, João Machadob, Élia Mateusb, Paulo Marcelinoc, Rui Pereirac, Philip Fortunac, Luís Bagulhoc, Luís Bentoc, Francisco Ribeiroa, Fernando Nolascoa, Américo Martinsb, Eduardo Barrosob
aDepartment of Nephrology, bDepartment of Transplantation, and cIntensive Care Unit, Hospital Curry Cabral, Centro Hospitalar Lisboa Central, Lisbon, Portugal
* Corresponding author.
ABSTRACT
Acute-on-chronic liver failure (ACLF) is a syndrome characterized by an acute deterioration of a patient with cirrhosis, frequently associated with multi-organ failure and a high short-term mortality rate. We present a retrospective study that aims to characterize the presentation, evolution, and outcome of patients diagnosed with ACLF at our center over the last 3 years, with a comparative analysis between the group of patients that had ACLF precipitated by infectious insults of bacterial origin and the group of those with ACLF triggered by a nonbacterial infectious insult; the incidence of acute kidney injury and its impact on the prognosis of ACLF was also analyzed. Twenty-nine patients were enrolled, the majority of them being male (89.6%), and the mean age was 53 years. Fourteen patients (48.3%) developed ACLF due to a bacterial infectious event, and 9 of them died (64.2%, overall mortality rate 31%); however, no statistical significance was found (p < 0.7). Of the remaining 15 patients (51.7%) with noninfectious triggers, 11 died (73.3%, overall mortality rate 37.9%); again there was no statistical significance (p < 0.7). Twenty-four patients (83%) developed acute kidney injury (overall mortality rate 65.5%; p < 0.022) at the 28-day and 90-day follow-up. Twelve patients had acute kidney injury requiring renal replacement therapy (41.37%; overall mortality rate 37.9%; p < 0.043). Hepatic transplant was performed in 3 patients, with a 100% survival at the 28-day and 90-day follow-up (p < 0.023). Higher grades of ACLF were associated with increased mortality (p < 0.02; overall mortality 69%). Conclusions: ACLF is a heterogeneous syndrome with a variety of precipitant factors and different grades of extrahepatic involvement. Most cases will have some degree of renal dysfunction, with an increased risk of mortality. Hepatic transplant is an efficient form of therapy for this syndrome.
Keywords: Acute-on-chronic liver failure, Acute kidney injury, Multi-organ failure, Hepatic transplant
RESUMO
A Doença Hepática Crónica Agudizada/Falência é um síndrome caracterizado por uma deterioração aguda de um doente com cirrose, frequentemente associada com falência multiorgânica e elevada mortalidade a curto prazo. Apresentamos estudo retrospetivo que teve como objetivo caracterizar a apresentação, evolução e prognóstico de doentes diagnosticados com Doença Hepática Crónica Agudizada/Falência no nosso Centro nos últimos 3 anos, comparando o grupo de doentes que tiveram Doença Hepática Crónica provocada por infeções bacterianas e os doentes com Doença Hepática Crónica Agudizada/Falência desencadeada por precipitantes que não a infeção bacteriana; foi também analisada a incidência de lesão renal aguda e o seu impacto no prognóstico na Doença Hepática Crónica Agudizada/Falência. Vinte e nove doente foram incluídos no estudo, a maioria do género masculino (89.6%), idade media de 53 anos. Catorze doentes (48.3%) desenvolveram Doença Hepática Crónica Agudizada devido a infeção bacteriana, 9 dos quais faleceram (64.2%, mortalidade global 31%), contudo, sem significado estatístico (p < 0.7); dos restantes 15 (51.7%) sem infeção bacteriana, 11 faleceram (73.3%, mortalidade global 37.9%), também sem significado estatístico (p < 0.7%). Vinte e quatro doentes (83%) desenvolveram lesão renal, mortalidade global de 65.5% (p < 0.022) aos 28 e 90 dias de seguimento. Doze doentes desenvolveram lesão renal aguda com necessidade de terapêutica de substituição da função renal (41.37%), mortalidade global de 37.9% ( p < 0.043). O transplante hepático foi realizado em 3 doentes, com uma sobrevida de 100% aos 28 e 90 dias de seguimento (p < 0.023); Graus elevados de Doença Hepática Crónica Agudizada estão associadas a mortalidade mais elevada (p < 0.02); mortalidade global de 69%. Conclusions: A Doença Hepática Crónica Agudizada é um síndrome heterogéneo, com uma variedade de fatores precipitantes e diferentes graus de envolvimento extra-hepático; a maioria das situações estará associada a disfunção renal, com aumento do risco de mortalidade; O transplante hepático será uma eficaz de tratamento deste síndrome.
Palavras-Chave: Doença hepática crónica agudizada, Lesão renal aguda, Falência multiorgânica, Transplante hepático
Introduction
Acute-on-chronic liver failure (ACLF) is a recently recognized entity defined by an acute deterioration of a patient with cirrhosis, either compensated or at least relatively stable decompensated [1]. ACLF is frequently associated with multi-system organ failure, consequent requirement of organ supports, and a high short-term mortality rate [1, 2].
Recently, the World Gastroenterology Organisation, the European Association for the Study of Liver Diseases (EASL), the American Association for the Study of Liver Diseases (AASLD), and the Asian-Pacific Association for the Study of the Liver (APASL) defined ACLF as a syndrome that occurs in patients with known chronic liver disease, with or without cirrhosis, characterized by acute decompensation of the liver (ascites, encephalopathy, gastrointestinal bleeding, and/or bacterial infection), and one or more extrahepatic organ dysfunction (kidney, brain, coagulation, circulation, and/or lung), with a high 28-day mortality rate (at least 15%) and up to 3 months from the onset [2–6].
The CANONIC (Acute-on-Chronic Liver Failure in Cirrhosis) study is currently the largest prospective multicenter study made on ACLF; it documented a prevalence of ACLF of 30.9%, with a high short-term mortality of 33% at 28 days and 51% at 90 days. The study also suggested an important role of dysregulated inflammation in the pathophysiology of this syndrome, since the degree of inflammatory reaction, which was estimated by leukocyte and C-reactive protein levels, was found to be an important parameter regarding the severity and outcome of ACLF. It was found that all patients with ACLF had leukocytosis and elevated levels of C-reactive protein, which was due to an inflammatory trigger such as bacterial infections and severe alcoholic hepatitis in 57% of the patients, or to yet unidentified mechanisms in the remaining 43%, which suggests an altered response to injury and immune dysfunction that leads to an inappropriate inflammatory response. In the CANONIC trial, the sequential organ failure assessment was used to identify organ failure; however, it was modified so that specific features of cirrhosis were taken into consideration. A 4-grade score was used to stratify patients with ACLF in accordance to the number of organ failures, grade 0 being the absence of organ failure and grades 1–3 those for patients with 1, 2, and >3 organ failures. Moreover, another important data from the CANONIC study was that kidney dysfunction alone (defined as serum creatinine [Scr] ranging from 1.5 to 1.9 mg/dL) is associated with a 28-day mortality greater than the predefined limit required for the diagnosis of ACLF. Contrariwise, any other single-organ failure was only associated with a 28-day mortality >15% when it occurred with concomitant renal injury [3].
ACLF can be triggered by intrahepatic or extrahepatic insults. Nonetheless, extrahepatic insults can be linked to a different outcome [7]. A potential precipitating event of the syndrome may not be identifiable [3]. Due to the growing recognition of ACLF as a distinct syndrome, we performed a retrospective study where we characterize the clinical presentation, evolution, and outcome of a population of patients with the diagnosis of ACLF at our center over the last 3 years, with a comparative analysis between the group of patients that had ACLF precipitated by infectious insults of bacterial origin and the group of those in whom a nonbacterial infectious insult was responsible for the development of the syndrome; the study also had the objective to analyze the incidence of acute kidney injury (AKI) and its impact on the prognosis of ACLF.
Materials and Methods
ACLF was diagnosed in accordance with the Chronic Liver Failure-Sequential Organ Failure Assessment (CLIF-SOFA) [3].
AKI was diagnosed using the adaptation of the Acute Kidney Injury Network (AKIN) criteria to define AKI in patients with cirrhosis, as proposed by the Acute Dialysis Quality Initiative (ADQI) along with members of the International Club of Ascites (ICA). According to these criteria, AKI is defined as an increase in the Scr level of ≥ 0.3 mg/dL within 48 h or an increase in the Scr level by≥ 50% from baseline that is known or presumed to have occurred within the prior 7 days [8, 9].
Inclusion criteria were known cirrhosis in patients admitted to the intensive care unit (ICU) of our center with the diagnosis of ACLF confirmed by clinical and analytical data between 2013 and 2015.
Exclusion criteria were patient ages <18 and >85 years; prior liver and/or kidney transplant; end-stage renal disease already on a regular dialysis program; pregnancy; hepatocellular carcinoma outside the Milan criteria, and known human immunodeficiency virus infection.
The model for end-stage liver disease (MELD) scoring system was used to estimate the severity of the hepatic dysfunction [10].
The outcome of patients was evaluated 28 and 90 days after ICU admission.
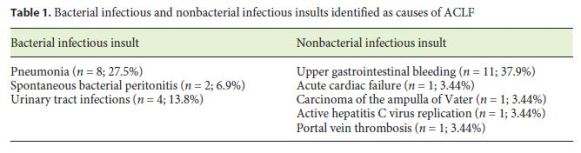
Different causes of decompensation were categorized into bacterial infectious insults, such as pneumonia, spontaneous bacterial peritonitis (SBP), and urinary tract infections, and nonbacterial infectious insults, such as active hepatitis C virus replication (HCV), upper gastrointestinal bleeding, portal vein thrombosis, acute cardiac failure, and carcinoma of the ampulla of Vater.
Statistical analysis was performed with SPSS, and the Kruskal-Wallis test and the Exact Fisher test were used.
A comparative analysis was made between the groups of patients that had ACLF precipitated by intrahepatic insults and those in whom an extrahepatic insult was responsible for the development of the syndrome.
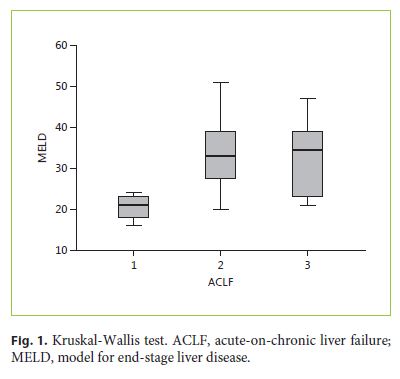
We also compared the MELD score with the different grades of ACLF that were estimated in this series to establish a possible association between the severity of chronic liver disease and the progression of ACLF.
The incidence of AKI and the need of renal replacement therapy (RRT) were determined to analyze its impact on the prognosis of ACLF.
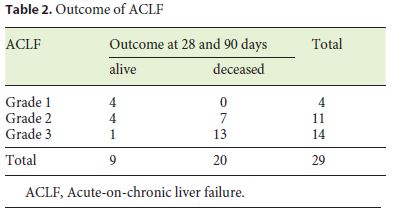
A comparative analysis between survival and liver transplant was made; we also compared the outcome of patients in the different grades of ACLF to determine the impact of the increasing systemic involvement on the prognosis of the syndrome.
Results
Sixty-two patients were admitted in the ICU with a new episode of acute decompensation of cirrhosis; a total of 29 patients met the inclusion criteria.
Of these 29 patients, 89.6% were male (n = 26), the mean age was 53 years (47.99 ± 58.01), the median age was 50 years, the minimum age was 18 years, and the maximum age was 81 years.
Regarding the etiology of cirrhosis, 12 patients had alcoholic liver cirrhosis (41.4%); 7 (24.1%) had cirrhosis due to both HCV infection and alcoholic liver cirrhosis; 6 patients had liver disease due to HCV infection alone(20.7%); 1 case (3.44%) had cirrhosis due to primary sclerosing cholangitis; 1 patient (3.44%) due to cryptogenic hepatic cirrhosis; 1 patient (3.44%) had hepatocellular carcinoma, and the final case had cirrhosis due to both hemochromatosis and alcoholic liver diseases.
ACLF was triggered by a bacterial infectious insult in 14 (48.3%) patients, and nonbacterial infectious insults were responsible for the development of ACLF in the remaining 15 (51.7%) patients, as demonstrated in Table 1.
The Kruskal-Wallis test (Fig. 1) was used to study a possible association with the increase of the MELD score and the different grades of ACLF; we observed that the MELD distribution varied in accordance with the ACLF grades 1, 2, and 3; however, this was more evident by comparing ACLF grade 1 with 2 and grade 1 with 3 ( p < 0.037) and less notorious when comparing ACLF grades 2 and 3.
Twenty-four patients (83%) developed AKI, and this was associated with an overall mortality rate of 65.5% at the 28-day and 90-day of follow-up (n = 19; p < 0.022).
AKI requiring RRT was verified in 12 patients (41.37%), with an overall mortality rate of 37.9 % (p < 0.043) at 28 90 days.
Fifteen patients (51.7%) had ACLF due to a nonbacterial infectious injury, 11 (73%) of whom died (overall mortality rate of 37.9%), but without statistical significance (p < 0.7). Of the remaining 14 patients with bacterial infectious insults, 9 died (64.3%, overall mortality rate 31%), again without statistical significance (p < 0.7%). The results were identical at 28 and 90 days in both groups. However, all patients with ACLF due to infectious insults developed AKI and ACLF, and statistical significance was found (n = 14; p < 0.042).
Hepatic transplant was performed in 3 patients, with a 100% survival at the 28-day and 90-day follow-up. Despite the reduced number of patients, statistical significance was noted (p < 0.023).
Higher grades of ACLF were associated with increased mortality (p < 0.02), as illustrated in Table 2. Identical results were noted at 28 and 90 days; and the overall mortality was 69%.
Discussion
The authors present the first series in Portugal of patients diagnosed with ACLF, and a heterogeneous population was identified. This syndrome can develop in patients with cirrhosis with variable etiologies, although most of those observed had alcoholic liver cirrhosis, which was in accordance with other series [3].
ACLF is considered a dynamic process, which may be reversible in approximately half of the cases or it can progress to a life-threatening condition [7]. Nevertheless, patients with a diagnosis of ACLF remain a diverse population, with different types of precipitating events and variations in the etiology of cirrhosis and presentation of organ failure [3, 11].
A variety of insults can precipitate ACLF, both of hepatic or extrahepatic origin; the main cause of acute decompensation of cirrhosis in this study was bacterial infection, which is described as the leading cause of hospitalization, decompensation, and mortality in cirrhosis [12].
The MELD score varied significantly between grade 1, grade 2, and grade 3 ACLF but less significantly between grade 2 and grade 3 ACLF. This may be due to the fact that ACLF is a systemic disorder, and the MELD is an indicator of hepatic dysfunction. As the syndrome progresses, its outcome may be associated more with the degree of multi-organ failure than with the severity of the hepatic disease.
We were not able to establish a difference between the outcome of ACLF caused by bacterial infectious insults ACLF triggered by nonbacterial infectious mechanisms. However, all patients with ACLF caused by infections developed AKI; this may be due to an increased systemic inflammation triggered by the infection, which has been suggested to contribute to the pathophysiological hallmarksresponsible for the development of structural AKI in patients with ACLF [13].
AKI was detected in most cases (n = 24; 83%), with a high 28-day and 90-day mortality; half of them (n = 12) required RRT, with a mortality rate of 92% in this subgroup of patients.
AKI in patients with cirrhosis may be due to functional changes, which are induced by renal hypoperfusion, accounting for approximately two-thirds of all cases; this is mostly due to diuretic therapy and lactulose-associated diarrhea, reversible in almost half of the situations. The remaining cases are classified as hepatorenal syndrome or volume non-responsive AKI. Structural changes, such as glomerulonephritis, acute tubular necrosis, and other forms of tubular dysfunction or parenchymal disease account for the remaining one-third of the cases of AKI in cirrhosis.
Contrariwise, in patients with ACLF, AKI secondary to structural changes is more common, this being due to the presence of inflammation and infection in the pathophysiological mechanisms of renal dysfunction in ACLF [13]. A recent report in the histological findings of 43 post-mortem kidney biopsies of patients with ACLF and decompensated cirrhosis showed that the bile cast nephropathy, an entity characterized by renal tubular injury secondary to direct toxic damage caused by the elevated levels of bilirubin and bile acids, is significantly more common in ACLF than in patients with cirrhosis [14].
The distinction between functional and structural AKI is of paramount importance when the hypothesis of hepatic transplant is being considered: functional AKI will probably solve with hepatic transplant alone; however, structural AKI may require simultaneous liver-kidney transplant [7, 15].
Conclusions
ACLF is a heterogeneous syndrome with a variety of etiologies for cirrhosis, precipitant factors, and different grades of extrahepatic organ involvement. Early diagnosis and quick reference to a hepatic transplant center could be crucial in the management and success of this clinical situation. Most cases will have some degree of renal dysfunction, with an increased risk of mortality. Hepatic transplant is an efficient form of therapy for this syndrome.
References
1 Jalan R, Gines P, Olson JC, et al: Acute-onchronic liver failure. J Hepatol 2012;52:1336–1348. [ Links ]
2 Gustot T, Fernandez J, Garcia E, et al: Clinical course of acute-on-chronic liver failure syndrome and effects on prognosis. Hepatology 2015;62:243–252. [ Links ]
3 Moreau R, Jalan R, Gines P, et al: Acute-onchronic liver failure is a distinct syndrome that develops in patients with acute decompensation of cirrhosis. Gastroenterology 2013;144:426–437. [ Links ]
4 Bajaj JS, OLeary JG, Reddy KR, et al: Survival in infection-related acute-on-chronic liver failure is defined by extrahepatic organ failures. Hepatology 2014;60:250–256. [ Links ]
5 Sarin SK, Kumar A, Almeida JA, et al: Acuteon-chronic liver failure: consensus recommendation of the Asian Pacific Association for the Study of the Liver (APASL). Hepatol Int 2009;3:269–282. [ Links ]
6 Jalan R, Yurdaydin C, Bajaj JS, et al: Toward an improved definition of acute-on-chronic liver failure. Gastroenterology 2014;147:4–10. [ Links ]
7 Shi Y, Yang Y, Hu Y: Acute-on-chronic liver failure precipitated by hepatic injury is distinct from that precipitated by extrahepatic insults. Hepatology 2015;62:232–242. [ Links ]
8 Nadim MK, Kellum JA, Davenport A, et al: Hepatorenal syndrome: the 8th International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care 2012;16:R23. [ Links ]
9 Wong F, Nadim MK, Kellum JA, et al: Working Party proposal for a revised classification system of renal dysfunction in patients with cirrhosis. Gut 2011;60:702–709. [ Links ]
10 Kamath PS, Wiesner RH, Malinchoc M, et al: A model to predict survival in patients with end-stage liver disease. Hepatology 2001;33:464. [ Links ]
11 Moreau R, Arroyo V: Acute-on-chronic liver failure: a new clinical entity. Clin Gastroenterol Hepatol 2015;13:836–841. [ Links ]
12 Jalan R, Stadlbauer V, Sen S, Chesshire L, Chang YM, Mookerjee RP: Role of predisposition, injury, response and organ failure in the prognosis of patients with acute-onchronic liver failure: a prospective cohort study. Crit Care 2012;16:R227. [ Links ]
13 Maiwall R, Sarin SK, Moreau R: Acute kidney injury in acute on chronic liver failure. Hepatol Int 2016;10:245–257. [ Links ]
14 Nayak S, Mathur RP, Ramanarayanan S, et al: Bile pigment nephropathy and acute tubular necrosis in decompensated cirrhotics and acute on chronic liver failure. Hepatology 2014;60(4 suppl):325A. [ Links ]
15 Durand F, Graupera I, Ginès P, Olson JC, Nadim MK: Pathogenesis of hepatorenal syndrome: implications for therapy. Am J Kidney Dis 2016;67:318–328. [ Links ]
Statement of Ethics
This study did not require informed consent or review/approval by the appropriate ethics committee.
Disclosure Statement
The authors have no conflicts of interest to disclose.
* Corresponding author.
Dr. Miguel Verdelho
Department of Nephrology, Hospital Curry Cabral
Rua da Beneficência 8
PT–1069-166 Lisbon (Portugal)
E-Mail miguelverdelhocosta@gmail.com
Received: January 24, 2017; Accepted after revision: May 2, 2017














