Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.25 no.1 Lisboa fev. 2018
https://doi.org/10.1159/000477769
CLINICAL CASE STUDY
Pelvic Catastrophe after Elastic Band Ligation in an Irradiated Rectum
Catástrofe Pélvica após Laqueação Elástica Hemorroidária em Recto Irradiado
Inês Pita, Pedro Bastos, Mário Dinis-Ribeiro
Serviço de Gastroenterologia, Instituto Português de Oncologia Francisco Gentil, Porto, Portugal
* Corresponding author.
ABSTRACT
Chronic radiation proctopathy is a frequent complication after both pelvic external radiation therapy and brachytherapy and most commonly presents as rectal bleeding. Deep rectal ulcers and fistulae are much rarer and more clinically challenging consequences. We present the case of a 72-year-old male with a history of prostate adenocarcinoma treated with brachytherapy, who was referred to our institution due to a deep painful rectal ulcer refractory to medical treatment. The ulcer presented shortly after a haemorrhoid elastic band ligation and progressed to rectourethral fistulisation despite both faecal and urinary diversion. Our case demonstrates the importance of favouring a conservative approach when dealing with an irradiated rectum.
Keywords: Brachytherapy, Radiation proctitis, Rectal ulcer, Rectal fistulae
RESUMO
A proctopatia rádica crónica é uma complicação frequente tanto após radioterapia pélvica externa como após braquiterapia e a apresentação mais comum são rectorragias. Úlceras rectais profundas e fístulas são consequências muito mais raras e clinicamente mais difíceis. Apresentamos o caso de um homem de 72 anos, com um adenocarnicoma prostático tratado com braquiterapia, referenciado à nossa instituição por uma úlcera rectal profunda e dolorosa, refractária a tratamento médico. A úlcera surgiu pouco tempo após a laqueação elástica de uma hemorróida e progrediu para uma fístula rectouretral apesar de derivação fecal e urinária. Este caso ilustra a necessidade de uma abordagem conservadora ao lidar com mucosa rectal irradiada.
Palavras-Chave: Braquiterapia, Proctite rádica, Úlcera rectal, Fístula rectal
Introduction
Rectal injury after radiation therapy for pelvic neoplasms is a well-described complication and can be divided into acute and chronic forms. It occurs both after external beam radiation therapy and brachytherapy; in the latter case, the anterior rectal wall is especially affected due to its close anatomical relation to the prostate and thus the radioactive seeds [1].
Chronic radiation proctopathy presents most commonly as rectal bleeding, and medical and/or endoscopic treatments are usually successful [2]. Severe complications such as rectal ulceration and rectourinary fistulisation are much rarer. Their management is challenging, most often requiring surgical measures. Both the symptoms and the treatment options cause significant morbidity and loss of quality of life.
Our case demonstrates the devastating consequences of these severe complications and their treatment.
Clinical Case
We describe the case of a 72-year-old male referred to our institution due to a painful radiogenic rectal ulcer refractory to medical therapy.
One year before referral, he was diagnosed with prostate adenocarcinoma treated with transurethral prostatectomy and brachytherapy. He also had a history of hypertension, dyslipidaemia, and ischaemic heart disease with angioplasty 20 years before and was medicated with a statin, a calcium channel blocker, an angiotensin receptor antagonist, and clopidogrel.
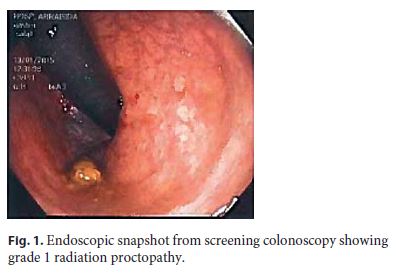
Six months before referral, the patient underwent a screening colonoscopy which documented only a grade 1 radiation proctopathy and no other rectal lesions (Fig. 1).
Three months later, due to complaints of passage of bright blood and clots per rectum, the patient underwent a rectosigmoidoscopy that revealed bleeding haemorrhoids, one of which was treated with elastic band ligation.
Rectal bleeding persisted, and shortly after the procedure, he developed intense, constant, and progressive anal pain, which worsened with walking, straining, and defecation and was only partially relieved by oral opioid and antineuropathic medication.
Several rectosigmoidoscopies documented an excavated ulcer on the anterior wall of the distal rectum, adjacent to the pectineal line, which increased in size (up to 30 mm across) (Fig. 2). The ulcer was biopsied in one of the examinations, and histology revealed an acute inflammatory infiltrate with extensive ulceration superimposed on chronically inflamed mucosa and no signs of malignancy.

The patient was medicated with topic sucralfate, with resolution of haematochezia, but with persistent debilitating pain and worsening endoscopic appearance. He was then referred to our institution, and a terminal colostomy for faecal diversion was proposed and performed.
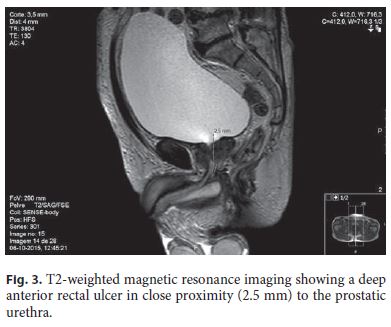
In the postoperative period, the patient experienced no relief in pain intensity (rated as 8 of 10 on the numerical pain scale), and a ganglion impar block was performed. A pelvic magnetic resonance showed the ulcer in close proximity to the urethra (Fig. 3); due to the risk of fistulisation, a cystostomy catheter was placed.
The procedures were effective in diminishing pain intensity, which the patient rated as 4 of 10 on follow-up consultations. He regained some quality of life, reporting an improved sleep pattern and resuming some of his previous daily activities.
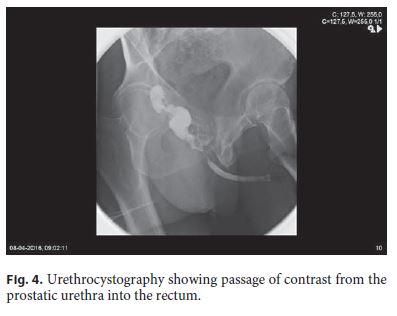
However, 5 months after colostomy, the patient developed mucus discharge from the urethra and passage of urine per rectum. A retrograde urethrography confirmed rectourethral fistulisation (Fig. 4). The complaints persisted despite continuous suprapubic cystostomy drainage. He is currently scheduled for exploratory laparotomy and intraoperative decision between continent vesicostomy and pelvic exenteration.
Discussion
Rectal injury after radiation therapy for pelvic neoplasms is a well-described complication and can be divided into acute and chronic forms.
Acute radiation proctitis occurs in up to 75% of patients after external beam radiation [3] and in 30–35% undergoing brachytherapy [2]. The most common symptom is diarrhoea; less typically it presents with pain, urgency, constipation, bleeding, and mucous discharge. Endoscopically, the mucosa is inflamed, friable, and oedematous, and on histopathology only the superficial mucosa is affected [2]. It occurs shortly after treatment and usually resolves within 3–6 months with conservative measures [4].
Chronic radiation proctopathy incidence peaks between 2 and 5 years after radiation therapy but has been described decades later [3]. It affects 5–20% of patients treated with radiation [5]. The most typical clinical presentation is rectal bleeding, but functional symptoms such as urgency, tenesmus, pain, incontinence, and mucous discharge can be present. In the most severe cases, ulceration or fistula can develop. Histologically, there is both mucosal and submucosal involvement [2] and severe vascular and fibrotic changes, characterised by progressive lamina propria fibrosis and obliterative endarteritis leading to epithelial atrophy, chronic mucosal ischaemia, and compensatory neovascularisation [3].
Radiation dose clearly plays a role in late rectal toxicity, as patients with late proctopathy have higher irradiated rectal volumes. However, a safe rectal radiation dose cutoff is difficult to establish as most studies find marked rectal radiation dose overlap between symptomatic and asymptomatic patients, and some patients with exceedingly high rectal doses develop no complications [6–8], suggesting individual susceptibility factors. Some patient characteristics that have been associated with increased risk of late radiation toxicity include vascular disease, diabetes, connective tissue disease, inflammatory bowel disease, HIV infection, smoking, and genetic variations [5].
The severity of chronic radiation proctopathy is commonly graded according to the Organization for Research and Treatment of Cancer/Radiation Therapy Oncology Group (EORTC/RTOG) toxicity scale [9]. This classification does not originally include ulceration, but most studies assign it a grade 3, while fistulae are considered a grade 4.
Grade 1–2 radiation proctopathy usually responds to medical and endoscopic treatments. First-line medical therapy is sucralfate enemas, which have shown better results than a combination of previously common treat ments: oral 5-ASA and topical steroids [10]. There is some evidence for the benefit of metronidazole [11] and vitamin A [12, 13]. The use of hyperbaric oxygen therapy has been gathering compelling evidence in the treatment of late radiation toxicity, including proctopathy [14, 15] ; however, availability and need for repeated lengthy treatments may limit its use. Endoscopically, the use of argon plasma coagulation is the more widespread treatment method for bleeding telangiectasia due to a perceived better safety profile [16]. There is also reported improvement after formalin application and heater or bipolar laser coagulation [2, 17] ; however, comparative studies between different endoscopic techniques are lacking.
The development of rectal ulcers and fistulae is a rare complication of radiation. A 2015 review by Kishan and Kupelian [2] on late rectal complications of low-dose brachytherapy places the incidence of serious toxicity (grade 3 or higher) at <1%. Due to their low prevalence, evidence on their prevention and optimal management is scarce.
A recent study by Leong et al. [7], on a large cohort of 4,690 patients who underwent brachytherapy for prostate cancer, found crude rates of rectal ulcer and recto-fistula of 0.19 and 0.26%, respectively, during a median followup of 53 months. Wallner et al. [8] reported a similar rate of rectal fistula (0.25%) in 3,126 brachytherapy patients over a median follow-up of 6 years.
In the first study, 8 out of 15 (53%) rectal ulcers healed with medical management; 6 progressed to fistula despite hyperbaric oxygen treatment in 2 and faecal diversion in 1.
Out of the 20 total fistulae reported in both studies, none healed without surgical intervention and only 5 had a successful surgical repair with maintenance of both bowel and bladder function after the procedure. Twelve patients had previous rectal or urinary interventions: 7 rectal biopsies, 4 urinary interventions, and 1 argon plasma coagulation treatment. Several previous studies have associated the development of rectal ulcer and fistulae with manipulation of an irradiated rectal mucosa [18–20].
Our case illustrates the cautiousness with which an irradiated rectum must be approached – a haemorrhoid elastic band ligation meant to alleviate moderate symptoms precipitated a far more challenging and disabling complication.
Due to the risks of manipulating irradiated mucosa, the unpredictability of complicated disease, and the poor functional outcomes after deep ulceration or fistulisation, treatment of radiation proctopathy should, whenever possible, rely on conservative measures, as suggested in an algorithm by Vanneste et al. [5]. Rectal biopsies are not helpful in its management and can only be justified if the suspicion of malignancy is high. Any endoscopic interventions (for radiation proctopathy or otherwise) should be reserved for intractable and incapacitating symptoms.
References
1 Grodsky MB, Sidani SM: Radiation proctopathy. Clin Colon Rectal Surg 2015;28:103–111. [ Links ]
2 Kishan AU, Kupelian PA: Late rectal toxicity after low-dose-rate brachytherapy: incidence, predictors, and management of side effects. Brachytherapy 2015;14:148–159. [ Links ]
3 Hayne D, Vaizey CJ, Boulos PB: Anorectal injury following pelvic radiotherapy. Br J Surg 2001;88:1037–1048. [ Links ]
4 Phan J, Swanson DA, Levy LB, et al: Late rectal complications after prostate brachytherapy for localized prostate cancer: incidence and management. Cancer 2009;115:1827–1839. [ Links ]
5 Vanneste BG, Van De Voorde L, de Ridder RJ, et al: Chronic radiation proctitis: tricks to prevent and treat. Int J Colorectal Dis 2015;30:1293–1303. [ Links ]
6 Keyes M, Spadinger I, Liu M, et al: Rectal toxicity and rectal dosimetry in low-dose-rate (125)I permanent prostate implants: a longterm study in 1,006 patients. Brachytherapy 2012;11:199–208. [ Links ]
7 Leong N, Pai HH, Morris WJ, et al: Rectal ulcers and rectoprostatic fistulas after (125)I low dose rate prostate brachytherapy. J Urol 2016;195:1811–1816. [ Links ]
8 Wallner K, Sutlief S, Bergsagel C, et al: Severe rectal complications after prostate brachytherapy. Radiother Oncol 2015;114:272–275. [ Links ]
9 Cox JD, Stetz J, Pajak TF: Toxicity criteria of the Radiation Therapy Oncology Group (RTOG) and the European Organization for Research and Treatment of Cancer (EORTC). Int J Radiat Oncol Biol Phys 1995;31:1341–1346. [ Links ]
10 Kochhar R, Patel F, Sharma SC, et al: Radiation-induced proctosigmoiditis. Dig Dis Sci 1991;36:103–107. [ Links ]
11 Cavcic J, Turcic J, Martinac P, et al: Metronidazole in the treatment of chronic radiation proctitis: clinical trial. Croat Med J 2000;41:314–318. [ Links ]
12 Ehrenpreis ED, Jani A, Levitsky J, et al: A prospective, randomized, double-blind, placebocontrolled trial of retinol palmitate (vitamin A) for symptomatic chronic radiation proctopathy. Dis Colon Rectum 2005;48:1–8. [ Links ]
13 van de Wetering FT, Verleye L, Andreyev HJ, et al: Non-surgical interventions for late rectal problems (proctopathy) of radiotherapy in people who have received radiotherapy to the pelvis. Cochrane Database Syst Rev 2016;4:CD003455. [ Links ]
14 Bennett MH, Feldmeier J, Hampson NB, et al: Hyperbaric oxygen therapy for late radiation tissue injury. Cochrane Database Syst Rev 2016;4:CD005005. [ Links ]
15 Clarke RE, Tenorio LM, Hussey JR, et al: Hyperbaric oxygen treatment of chronic refractory radiation proctitis: a randomized and controlled double-blind crossover trial with long-term follow-up. Int J Radiat Oncol Biol Phys 2008;72:134–143. [ Links ]
16 Silva RA, Correia AJ, Dias LM, et al: Argon plasma coagulation therapy for hemorrhagic radiation proctosigmoiditis. Gastrointest Endosc 1999;50:221–224. [ Links ]
17 Lenz L, Rohr R, Nakao F, et al: Chronic radiation proctopathy: a practical review of endoscopic treatment. World J Gastrointest Surg 2016;8:151–160. [ Links ]
18 Theodorescu D, Gillenwater JY, Koutrouvelis PG: Prostatourethral-rectal fistula after prostate brachytherapy. Cancer 2000;89:2085–2091. [ Links ]
19 Chrouser KL, Leibovich BC, Sweat SD, et al: Urinary fistulas following external radiation or permanent brachytherapy for the treatment of prostate cancer. J Urol 2005;173:1953–1957. [ Links ]
20 Thornhill JA, Long RM, Neary P, et al: The pitfalls of treating anorectal conditions after radiotherapy for prostate cancer. Ir Med J 2012;105:91–93. [ Links ]
Statement of Ethics
This study did not require informed consent or review/approval by the appropriate ethics committee.
Disclosure Statement
The authors have no conflict of interest to declare.
* Corresponding author.
Dr. Inês Pita
Serviço de Gastroenterologia, Instituto Português de Oncologia Francisco Gentil
Rua Dr. António Bernardino de Almeida
PT–4200-072 Porto (Portugal)
E-Mail neispita@hotmail.com
Received: March 14, 2017; Accepted after revision: May 23, 2017














