Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.25 no.3 Lisboa jun. 2018
https://doi.org/10.1159/000481175
CLINICAL CASE STUDY
Endoscopic Ultrasound-Guided Choledochoduodenostomy as Palliative Treatment: A Challenging Case Report
Coledocoduodenostomia guiada por ecoendoscopia como tratamento paliativo: um caso clínico desafiante
Helena Ribeiro, Richard Azevedo, Ana Caldeira, Rui Sousa, Eduardo Pereira, António Banhudo
Gastroenterology Department, Amato Lusitano Hospital, Castelo Branco, Portugal
* Corresponding author.
ABSTRACT
We report the case of an 88-year-old female with obstructive jaundice due to a periampullary tumor. The patient developed acute cholangitis and consequent clinical deterioration, so it was decided to perform palliative biliary drainage. Due to duodenal tumor invasion, it was not possible to perform endoscopic retrograde cholangiopancreatography. A different approach was attempted and it was decided to carry out an endoscopic ultrasound-guided choledochoduodenostomy. This procedure was performed with a linear echoendoscope, and using a duodenal bulbar approach, a fistula was created between the bulb and the common bile duct. A self-expandable fully covered metal biliary stent was placed in the common bile duct under endoscopic and fluoroscopic guidance, allowing biliary drainage. The patient presented clinical improvement. However, 3 weeks after being discharged, she was readmitted to our department with hematemesis associated with the migration of the biliary stent to the duodenal bulb. Endoscopic hemostasis was performed but the patient had multiple bleeding relapses that were controlled through arterial embolization. Despite the migration of the biliary stent, the fistula between the duodenum and the common bile duct remained patent, allowing a successful palliation of the obstructive jaundice. Therefore, despite the occurred complication, we admitted a technical and clinical success of the endoscopic ultrasound-guided choledochoduodenostomy. This is an emerging technique and a valuable alternative for palliative biliary drainage in cases of malignant distal obstruction. This clinical report supports this finding, reporting technical aspects of the procedure, associated complications and their management as well as the clinical outcomes.
Keywords: Endoscopic ultrasound-guided choledochoduodenostomy,·Periampullary tumors, Obstructive jaundice, Palliative biliary drainage
RESUMO
Apresentamos o caso de uma doente do sexo feminino, de 88 anos de idade, com icterícia obstrutiva devido a um tumor periampular, complicada com colangite aguda. Foi proposta drenagem biliar paliativa através da colocação de uma prótese biliar por colangiopancreatografia retrógrada endoscópica. No entanto, devido a invasão tumoral do duodeno, não foi possível realizar esta abordagem e como alternativa foi efetuada uma coledocoduodenostomia guiada por ecoendoscopia. Este procedimento foi realizado com um ecoendoscópio linear e, utilizando uma abordagem através do bulbo duodenal, foi criada uma fístula entre o bulbo e a via biliar principal. Uma prótese metálica auto-expansível totalmente coberta foi colocada na via biliar principal com apoio endoscópico e fluoroscópico, permitindo a drenagem biliar. A doente apresentou melhoria do estado clínico com resolução do quadro de colangite aguda. No entanto, três semanas após a alta, ela foi novamente internada no nosso serviço por hematemeses associadas à migração da prótese biliar para o bulbo. Foi realizada hemostase endoscópica, no entanto, por apresentar várias recidivas da hemorragia optou-se pela embolização arterial, verificando-se controlo definitivo da hemorragia. Apesar da migração da prótese biliar, a fístula entre o duodeno e o a via biliar principal permaneceu patente, permitindo uma paliação da icterícia obstrutiva. Portanto, admitimos o sucesso técnico e clínico da coledocoduodenostomia guiada por ecoendoscopia. Esta é uma técnica emergente e uma alternativa valiosa para a drenagem biliar paliativa em casos de obstrução distal maligna. O presente caso clínico é representativo desse valor, relatando os aspetos técnicos do procedimento efetuado, complicações associadas e a sua abordagem, bem como a evolução clinica da doente.
Palavras-Chave: Coledocoduodenostomia guiada por ecoendoscopia,·Tumores periampulares,·Icterícia obstrutiva, Drenagem biliar paliativa
Introduction
Periampullary carcinomas are tumors developed near the ampulla of Vater. They include lesions originated from the ampulla of Vater, head and neck of the pancreas, distal common bile duct (CBD) and from the second part of the duodenum. Usually, periampullary tumors are diagnosed in advanced stages due to infiltration of local structures or disseminated disease. Malignant obstructive jaundice is the most common presentation and its management can be complex [1, 2]. In patients who do not qualify for surgical treatment, palliative biliary tract drainage must be considered as it improves quality of life and prevents associated complications, such as cholangitis, pruritus, nausea, and anorexia [3, 4]. The preferred procedure to relieve biliary obstruction is endoscopic retrograde cholangiopancreatography (ERCP) with stent placement, with a success rate of 90% [5]. However, in some situations, it is not possible to perform ERCP, for example, in cases of inaccessible papilla due to periampullary or duodenal tumor invasion [6]. In such circumstances, percutaneous transhepatic biliary drainage (PTBD) is conventionally the alternative procedure, but it is associated with substantial morbidity. Recently, interventional procedures using endoscopic ultrasound (EUS) have been developed as an alternative technique, namely EUS-guided choledochoduodenostomy (EUS-CD), a transduodenal approach for CBD drainage [6–8].
Clinical Case
An 88-year-old female presented to the emergency department due to an episode of hematochezia, abdominal pain for the last 2 days, jaundice, and progressive asthenia. She had a past medical history of chronic renal disease, arterial hypertension, cardiac insufficiency, a cardiac pacemaker, and atrial fibrillation, medicated with oral anticoagulant. On admission, she was afebrile and hemodynamically stable. Laboratory tests revealed: hemoglobin 10 g/dL, leukocytes 10,740/mm3, normal C-reactive protein, aspartate transaminase 179 U/L, alanine transaminase 301 U/L, alkaline phosphatase 539 U/L, total bilirubin 7.2 mg/dL (conjugated bilirubin 6.0 mg/dL), serum creatinine 2.2 mg/dL, prolonged prothrombin time, and international normalized ratio. Transabdominal ultrasound and computed tomography demonstrated dilation of the intrahepatic biliary ducts, CBD and Wirsung. A periampullar mass was identified compressing the distal portion of the CBD and invading the second part of the duodenum. There were no metastatic lesions or vascular involvement and it was not possible to exclude peripancreatic lymphadenopathies. An upper endoscopy was performed revealing a deformed and stenotic transition from the bulb to the second portion of the duodenum. Distally, an apparent villous and friable tissue was visualized, which was difficult to assess. No other potential bleeding lesions were identified. The examination was interrupted due to patient intolerance. Coagulation status was corrected and the patient started taking enoxaparin. A colonoscopy was performed and lesions were excluded.
Further laboratory tests revealed a CA 19.9 level of 177.89 U/L that, in the presence of a periampullar mass with duodenal invasion, can be indicative of malignant CBD stenosis, despite the concomitant biliary obstruction. The patient experienced clinical deterioration with evidence of acute cholangitis and increasing of the total bilirubin level (18.6 mg/dL). Considering the clinical situation, age, and comorbidities of the patient, it was decided (together with the patient and her family) to perform a palliative biliary drainage. The duodenal deformation made it impossible to carry out ERCP; therefore, it was decided to perform EUS-CD.
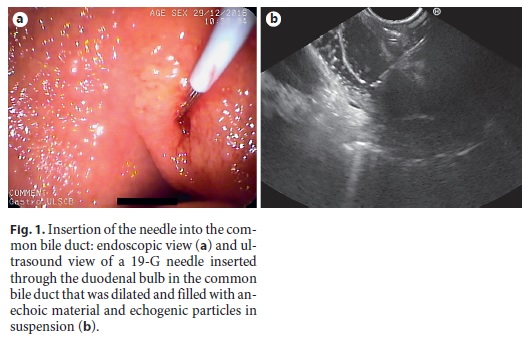
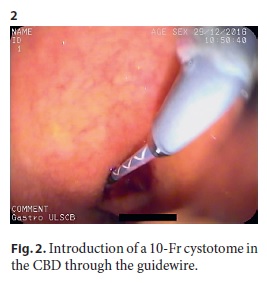
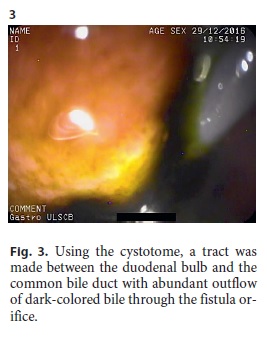
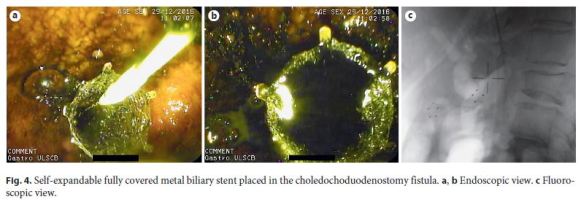
The EUS-CD was performed with a linear echoendoscope. Through a duodenal bulbar approach, with the echoendoscope placed upstream of the duodenal stenosis, a dilated CBD was identified, up to 20 mm, filled with anechoic material and some echogenic particles in suspension. An avascular path for needle introduction was determined with color Doppler. A 19-G needle was inserted into the CBD, followed by aspiration of 40 mL of dark-colored bile. A 0.035-inch diameter straight tip guidewire was introduced through the needle channel and advanced to the right branch of the intrahepatic bile duct, confirmed on fluoroscopy (Fig. 1). The needle was removed and the guidewire was left in place allowing the introduction of a 10-Fr cystotome. Using this cystotome, a tract was made between the duodenal bulb and the CBD (Fig. 2). An abundant outflow of black bile through the fistula orifice was immediately observed (Fig. 3). The cystotome was then removed and a self-expandable fully covered metal biliary stent, 60 × 10 mm, was placed in the bile duct under endoscopic and fluoroscopic guidance (Fig. 4). The positioning of the stent was confirmed on fluoroscopy and with ultrasound. During the procedure, no complications occurred.
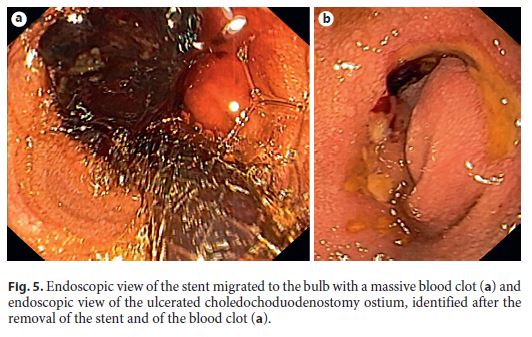
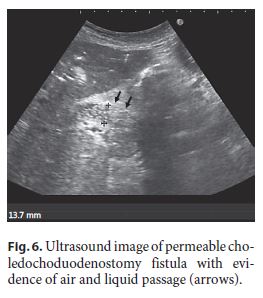
The patients acute cholangitis was resolved, with considerable decrease in the total bilirubin. It was decided to continue the administration of enoxaparin instead of oral anticoagulation. One week after discharge, the abdominal ultrasound confirmed the correct position of the biliary stent. However, 5 days later, she was readmitted due to hematemesis. Upper endoscopy revealed that the stent had migrated in the bulb and a massive duodenal blood clot was visible. It was possible to observe the choledochoduodenostomy ostium with circumferential ulceration with a small visible vessel and evidence of hemobilia (Fig. 5a, b). Adrenalin injections followed by polidocanol injections were performed in the ulcerated areas. However, the patient experienced recurrent hemorrhage with the need for several red blood cell transfusions. In order to control the bleeding, it was necessary to perform embolization of the branch of the superior mesenteric artery that anastomoses with the gastroduodenal artery with polyvinyl alcohol foam embolization particles and microcoil embolization of the gastroduodenal artery. There were no more bleeding relapses. Abdominal ultrasound performed prior to discharge confirmed the patency of the duodenal CBD fistula (Fig. 6).
The patient did not experience other episodes of acute cholangitis or increased bilirubin. Three months later, a palliative duodenal stent was placed due to gastrointestinal obstructive symptoms. Despite this episode, the patient remained clinically well for almost 6 months after the CBD palliative drainage, until she presented clinical deterioration and died of acute-onset chronic renal failure.
Discussion
In cases of malignant obstructive jaundice and when ERCP is not a possible procedure, endoscopic ultrasound-guided biliary drainage (EUS-BD) can be considered as a minimal invasive alternative to PTBD or surgical interventions [5, 8]. EUS-BD was described for the first time in 2001 by Giovannini [9] and since then multiple studies regarding the techniques, indications, safety, and efficacy have been published. Extrahepatic and intrahepatic routes may be used and biliary drainage may be achieved transmurally by an anterograde approach, bridging the bile duct stricture, or by a retrograde approach, using a transpapillary rendezvous maneuver. Therefore, the drainage route depends on the indication, obstruction level, and anatomical circumstances [5, 7, 10]. EUS-CD is an anterograde transduodenal approach for the drainage of the CBD [7]. This procedure has an overall weighted technical success rate of 93% and clinical success rate of 98% [5, 7]. The overall adverse event rate reported for EUS-CD is 16% [7]. Most adverse events are classified as mild to moderate and can be treated conservatively. They include pneumoperitoneum (the most frequent complication), infection (cholangitis, peritonitis, cholecystitis), bile leakage, bleeding, abdominal pain, perforation, and stent migration [7, 8].
In this case report, the EUS-CD was the procedure of choice after taking into account the comorbidities of the patient, the obstructive process of the CBD and the EUS expertise of our department. Other interventional options, like the surgical approaches, are associated with a high frequency of adverse events and procedure-related mortality [5]. PTBD and EUS-CD have comparable efficiency; however, PTBD is associated with a higher rate of adverse events and a higher cost due to the need for more reinterventions [5, 7]. In fact, Khashab et al. [8] concluded that in patients with distal biliary obstruction after failed ERCP successful biliary drainage was similar in EUS-CD and PTBD (86.4 vs. 92.2%, p = 0.40). Furthermore, they concluded that EUS-CD was associated with lower rates of adverse events compared to PTBD (15.7 vs. 80.4%) and that health care costs for PTBD were twice that of the EUS-BD group.
Our patient experienced bleeding 3 weeks after the procedure. Bleeding is an expected adverse event related to EUS-CD. In this case, hemorrhage was associated with the stent migration and probably also with the periampullary tumor and facilitated by the anticoagulation therapy [7]. Concerning the types of stents, both plastic and self-expandable metal stents (SEMS) have been used for EUS-CD. There are no comparative studies between metallic and plastic stents in terms of the efficacy and safety. However, SEMS has some advantages, for example, a larger diameter, better visibility, higher flexibility, and a longer patency [5]. Stent migration is still a problem of the technique, even using SEMS. In fact, the lack of specific devices, like tailored stents with antimigration properties, is a current challenge for endosonographers who perform EUS-CD [8]. In this patient, despite the displacement of the SEMS, the duodenal CBD fistula remained patent, allowing the palliation of the obstructive jaundice. Therefore, despite the complications, we admitted a technical and clinical success of the EUS-CD.
References
1 Blechacz B, Gores GJ: Tumors of the bile ducts, gallbladder, and ampulla; in Feldman M, Friedman LS, Brandt LJ (eds): Sleisenger and Fordtrans Gastrointestinal and Liver Disease, ed 10. Philadelphia, Elsevier Inc, 2017, pp 1184–1200.e5. http://dx.doi.org/10.1016/B978-1-4557-4692-7.00069-7. [ Links ]
2 Lai ECH, Lau SHY, Yee W: The current status of preoperative biliary drainage for patients who receive pancreaticoduodenectomy for periampullary carcinoma: a comprehensive review. http://dx.doi.org/10.1016/j.surge.2014.02.004. [ Links ]
3 Abraham NS, Barkun JS, Barkun AN: Palliation of malignant biliary obstruction: a prospective trial examining impact on quality of life. Gastrointest Endosc 2002;56:835–841. [ Links ]
4 Perone JA, Olino K, Riall TS: Palliative care for pancreatic and periampullary cancer. Surg Clin North Am 2017; 96: 1415–1430. http://dx.doi.org/10.1016/j.suc.2016.07.012. [ Links ]
5 Fusaroli P, Jenssen C, Hocke M, Burmester E, Buscarini E, Havre RF, et al: EFSUMB Guidelines on Interventional Ultrasound (INVUS), Part V: EUS-Guided Therapeutic Interventions (Long Version). Ultraschall Med 2016;37:412–420. [ Links ]
6 Ali M, Ali K, Todd A, Sobia HB, Sofi A, Artifon ELA, et al: Endoscopic ultrasound-guided biliary drainage: a systematic review and meta-analysis. Dig Dis Sci 2016;61:684–703. [ Links ]
7 Ogura T, Higuchi K: Technical tips of endoscopic ultrasound-guided choledochoduodenostomy. World J Gastroenterol 2015;21: 820–828. [ Links ]
8 Khashab MA, Valeshabad AK, Afghani E, Singh VK, Kumbhari V, Messallam A, et al: A comparative evaluation of EUS-guided biliary drainage and percutaneous drainage in patients with distal malignant biliary obstruction and failed ERCP. Dig Dis Sci 2015;60:557–565. http://link.springer.com/10.1007/s10620-014-3300-6. [ Links ]
9 Giovannini M: Endoscopic ultrasound-guided bilioduodenal anastomosis: a new technique for biliary drainage. Endoscopy 2001;33:898–900. [ Links ]
10 Ogura T, Higuchi K: Technical tips for endoscopic ultrasound-guided hepaticogastrostomy. World J Gastroenterol 2016;22:3945– 3951. [ Links ]
Statement of Ethics
This study did not require informed consent nor review/approval by the appropriate ethics committee.
Disclosure Statement
The authors declare no conflicts of interest.
* Corresponding author.
Dr. Helena Sofia Brito Ribeiro
Gastroenterology Department, Hospital Amato Lusitano
Avenida Pedro Álvares Cabral
PT–6000-085 Castelo Branco (Portugal)
E-Mail helena.britoribeiro@gmail.com
Received: May 25, 2017; Accepted after revision: September 1, 2017
Author Contributions
Helena Ribeiro: drafting of the manuscript, literature search, patient care, first author. Richard Azevedo: drafting of the manuscript, patient care. Ana Caldeira and Eduardo Pereira: patient care and critical revision of the manuscript. Rui Sousa and António Banhudo: critical revision of the manuscript and final approval.














