Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.26 no.2 Lisboa abr. 2019
https://doi.org/10.1159/000487820
ORIGINAL ARTICLE
Endoscopic Submucosal Dissection for the Treatment of Superficial Epithelial Gastric Neoplasia in a Portuguese Centre
Disseção endoscópica da submucosa no tratamento da neoplasia epitelial gástrica num centro Português
Rita Seara Costaa, Aníbal Ferreiraa, Tiago Leala, Dalila Costaa-c, Carla Rolandaa-c, Raquel Gonçalvesa
aDepartment of Gastroenterology, Braga Hospital, Braga, Portugal; bLife and Health Sciences Research Institute (ICVS), School of Medicine, University of Minho, Braga, Portugal; cICVS/3B’s – PT Government Associate Laboratory, Guimarães/Braga, Portugal
* Corresponding author.
ABSTRACT
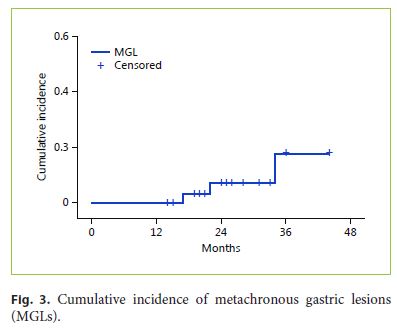
Background: The emergence of endoscopic submucosal dissection (ESD) made possible en bloc resection of neoplastic gastric lesions, regardless of lesion size, with reduced rates of complications and recurrence. This technique has become the preferred method for curative resection, instead of conventional endoscopic mucosal resection and surgery, when distant metastases have negligible risk. In Western countries experience with this technique has evolved quickly, with an increasing number of case series reported in the literature. This study aims to report the short- and long-term outcomes of ESD in gastric epithelial neoplastic lesions by a single operator in a Portuguese centre. Methods: A retrospective analysis of all gastric ESDs in a tertiary specialised unit during a 5-year period, between May 2012 and September 2017, was performed. Results: A total of 114 ESDs of gastric epithelial lesions were performed during this period; 96.5% of them were removed en bloc and 87.6% with R0 resection. A curative treatment was achieved in 83.2% of the cases. Complications occurred in 13.2% of the procedures, including early and delayed bleeding in 12 patients (10.5%) and one perforation (0.9%). With a median follow-up period of 12 months (interquartile range [IQR] = 18), 6 cases of recurrence at the previous ESD site were diagnosed: 4 residual lesions and 2 local recurrences in previous R0 resections. Residual lesions occurred more often in patients with larger lesions (median = 40.0 mm, IQR = 26 vs. median = 20.0 mm, IQR = 15, p = 0.008) and with positive horizontal margins (HMs) after resection (50.0 vs. 0.0%, Fisher exact test, p < 0.001). The cumulative incidence of metachronous gastric lesions at 34 months was 16.1%. All new lesions were effectively treated using an endoscopic technique. The disease-specific survival at 12 months was 100%. Conclusion: This study showed that ESD is an effective resection technique for gastric lesions with a good safety profile, confirming other European series. Regardless, high en bloc resection positive HM is still a problem in some specimens resected by ESD. Endoscopic surveillance can detect local recurrence and new lesions during early stages, potentially treatable by endoscopy.
Keywords: Endoscopic resection, Submucosal dissection, Upper endoscopy, Gastric epithelial neoplasia, Early gastric cancer, Low-grade intraepithelial neoplasia, High-grade intraepithelial neoplasia
RESUMO
Introdução: O aparecimento da dissecção endoscópica da submucosa (ESD) tornou possível a resseção em bloco de lesões neoplásicas superficiais do estômago, independentemente da sua dimensão, com reduzidas taxas de complicações e recorrência. Esta técnica tem evoluído como método preferencial face à mucosectomia convencional e cirurgia, quando a metastização à distância tem risco negligenciável. No mundo ocidental a experiência nesta técnica tem evoluído de forma rápida surgindo um número crescente de séries na literatura. Este estudo tem como objetivo reportar os resultados a curto e longo prazo da ESD de lesões epiteliais gástricas realizadas por um único operador num centro Português. Metodologia: Análise retrospetiva unicêntrica dos casos de ESD de lesões epiteliais gástricas, realizadas durante um período de 5 anos, entre maio de 2012 e setembro de 2017. Resultados: Foram realizadas 114 ESDs de neoplasias epiteliais gástricas durante o período em estudo, com uma taxa de resseção em bloco de 96.5% e R0 de 87.6%. A resseção curativa confirmou-se em 83.2% dos casos. Ocorreram complicações em 13.2% dos procedimentos, incluindo hemorragia em 12 doentes (10.5%) e 1 perfuração (0.9%). Com uma mediana de follow-up de 12 meses (variação interquartil [IQR] 18), verificaram-se 6 casos de recorrência local: 4 lesões residuais e 2 recorrências em resseções R0 prévias. Observaram-se mais frequentemente lesões residuais de ESD de lesões de maiores dimensões (mediana = 40.0 mm, IQR = 26 vs. mediana = 20.0 mm, IQR = 15, p = 0.008) e com margens horizontais (HM) positivas após a resseção (50.0% vs. 0.0%, Teste exato de Fisher, p < 0.001). A incidência cumulativa de lesões gástricas metácronas aos 34 meses foi de 16.1%. Todas as novas lesões foram eficazmente tratadas por endoscopia. A sobrevivência específica aos 12 meses de follow-up foi de 100%. Conclusão: Este estudo mostra que a ESD gástrica é uma técnica eficaz e segura para o tratamento de lesões neoplásicasprecoces confirmando a maioria das séries europeias. Embora a ESD permita geralmente uma resseção em bloco as HM positivas continuam a ser um problema em alguns doentes. A vigilância endoscópica pode detetar recorrência local e novas lesões, em estádios precoces, potencialmente tratáveis por endoscopia.
Palavras-Chave: Resseção endoscópica, Disseção submucosa, Endoscopia digestiva alta, Neoplasia epitelial gástrica, Cancro gástrico precoce, Neoplasia intraepitelial de baixo grau, Neoplasia intraepitelial de alto grau
Introduction
Endoscopic submucosal dissection (ESD) is now widely accepted as the first approach in the treatment of early gastric cancer (EGC), if suitable for en bloc resection, and with a very low risk of lymph node metastasis [1, 2]. According to the Japanese Gastric Cancer Association and the European Society of Gastrointestinal Endoscopy, there are two different types of indications for ESD in the treatment of EGC (limited to the mucosa or the mucosa and submucosa): absolute and expanded indications [2, 3]. The absolute criteria (differentiated mucosal cancers ≤20 mm, without ulcerative findings and without lymphatic vascular invasion) for ESD in EGC were adapted from the endoscopic mucosal resection (EMR) indications, with higher rates of en bloc and complete resections with ESD [3, 4]. With the data from two large Japanese cancer centres, expanded indications were added to the Japanese guidelines in 2010 (differentiated mucosal cancers, without ulcerative findings and without lymphatic vascular invasion, regardless of tumour size; differentiated mucosal cancers, with ulcerative findings ≤30 mm and without lymphatic vascular invasion; differentiated minute (5 years did not show differences in survival rates between patients undergoing curative ESD for absolute and expanded indications of EGC. The 5-year overall survival rates of the EGC patients with curative ESD for absolute indications and for expanded indications of differentiated-type EGC were 93.0 and 92.2%, respectively, and the 5-year disease-specific survival rates of the EGC patients with curative ESD for absolute indications and for expanded indications of differentiated-type EGC were both 99.9% [9].
This study aims to report the short- and long-term outcomes of ESD in the treatment of gastric superficial epithelial neoplastic lesions in a Portuguese endoscopy unit, and to evaluate the risk factors for early local recurrence.
Patients and Methods
Patients and Study Design
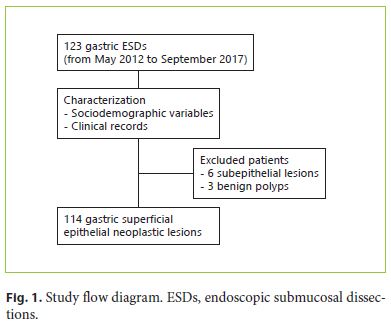
All consecutive patients who underwent ESD for gastric neoplasia between May 2012 and September 2017 at Braga Hospital were analysed. Data from electronic patient files were collected, including demographic and clinical characteristics, endoscopies, treatments, and histology reports. Patients submitted to ESD with subepithelial lesions or large polyps and whose histopathology showed hyperplasia were excluded from this study (Fig. 1).
Description of the ESD Technique
Lesions were evaluated with a high-definition endoscope with virtual chromoendoscopy (narrow-band imaging) before the procedures, in order to establish the feasibility of endoscopic resection, the characterisation and delimitation of the lesion, and the decision on the best strategy. As a general rule, no additional complementary procedures such as endoscopic ultrasound or computed tomography were done before the endoscopic treatment.
The morphology of the lesions was described according to the Paris classification. The location was assumed dividing the stomach’s long axis into three segments – upper (cardia and fundus), middle (body and angle), and lower (antrum and prepylorus) – and the circular axis into four segments – lesser curvature, greater curvature, anterior wall, and posterior wall. The size was defined as the maximum diameter of the lesion.
Antiplatelet (clopidogrel/ticlopidine) and anticoagulant agents were always stopped according to the guidelines. Low-dose acetysalicylic acid was only maintained in high-risk patients when indicated by the cardiologist or vascular surgeon.
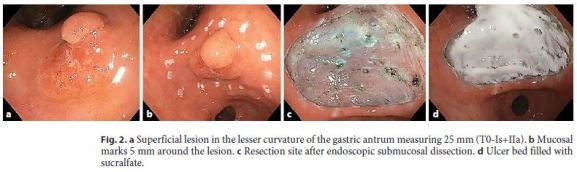
All ESDs were performed by a single operator with prior animal model experience and a 6-month period of training in a Portuguese endoscopy unit specialised in advanced endoscopic resection techniques. All procedures were done with a standard singlechannel scope (usually GIF-H180 or GIF-H185, and between 2012 and 2015 episodically GIF-Q165; Olympus), an Erbe electrosurgical system (VIO 300 D), and under carbon dioxide insufflation. Most of the patients underwent general anaesthesia with orotracheal intubation and the others were sedated with propofol. After identifying the target lesion, marks were made 5 mm laterally to the margin using argon plasma coagulation (Disposable EndoProbe, 2.3 mm, 600K0200; ARCO Söring) or a needle knife (KD10Q-1; Olympus). The submucosal injection was performed with a very dilute epinephrine solution (1:250,000) in normal saline and a few drops of methylene blue. The initial mucosal incision was done with the needle knife (Endo Cut I mode, 60 W, effect 2) followed by a circumferential mucosal incision with an insulated tip knife 2 (KD-611L; Olympus, Endo Cut I mode, 60 W, effect 3) and, finally, submucosal dissection using the same knife and settings. Endoscopic haemostasis was done with a Coagrasper (FD-410LR; Olympus, soft coagulation mode, 50 W, effect 4) and performed as needed during and after the procedure. A cap was only used in some difficult procedures to increase stability and help in endoscopic haemostasis. Finally, the resection site was covered with sucrose sulfate-aluminium complex (sucralfate) (Fig. 2).
The patients were hospitalised under pantoprazole intravenous infusion (8 mg/h) for the first 48 h (which was then switched to oral intake, 40 mg twice a day for a total of 2 weeks) plus sucralfate. They usually started oral liquid diet 36–48 h after the procedure and were discharged on the next day (day 3 after the ESD) in the absence of complications.
Regarding complications, immediate bleeding was considered if there was intraoperative bleeding that required blood transfusion or modification/suspension of the endoscopic treatment. Early (24 h) bleeding was considered if, during the postoperative period, haemorrhage (haematemesis, melena, or haematochezia) occurred or if there was a decrease in the haemoglobin level >2 g/dL, with need for blood transfusion or endoscopic/surgical intervention. Minimal bleeding during the procedures was not accounted for and was managed with epinephrine injection or coagulation with the tip of the knife or a coagulation forceps. Perforation was considered if it was endoscopically visible or if, under clinical indication, it was radiologically confirmed.
Histopathological Evaluation
The resected specimens were stretched and pinned to a polystyrene plate before being embedded in formaldehyde for fixation. Fragmented specimens were reconstituted to the greatest extent possible. Histology specimens were classified according to the World Health Organization classification of gastric epithelial neoplasia [10]. Cases showing both low-grade intraepithelial neoplasia (LGIN) and high-grade intraepithelial neoplasia (HGIN) were classified as HGIN. The diagnosis of intramucosal carcinoma was based on invasion of the lamina propria or muscularis mucosae by neoplastic epithelium.
Resection was defined as en bloc if the lesion was resected in one piece and as piecemeal if it was fragmented into two or more pieces. A complete resection (R0) was considered if the resection was en bloc and both horizontal margins (HMs) and vertical margins (VMs) were negative (HM0 and VM0, respectively). Incomplete resection (R1) was considered if the lesion was intercepted in at least one of the margins or in cases of piecemeal resection.
Resection was considered curative if all the following conditions were fulfilled: R0 resection, no lymphovascular infiltration, and (1) tumours, irrespective of size, differentiated type, pT1a, without ulcerative findings, or (2) tumours < 3 cm, differentiated type, pT1b (SM1 < 500 μm).
The patients with submucosal invasive cancers, regardless of curative resection, and all patients who did not fulfil the criteria for endoscopic curative resection were discussed in a multidisciplinary meeting, and surgical treatment (gastrectomy with lymph node dissection) was proposed eventually. In the cases of non-curative ESD where surgery was not considered the best option, new endoscopic treatment or stringent follow-up was the subsequent approach.
Follow-Up Schedule and Definitions
Surveillance endoscopy was performed 3 and/or 6 months after the ESD and every 12 months thereafter. Biopsies of the previous ESD site or suspicious areas in search for synchronous gastric lesions (SGLs) or metachronous gastric lesions (MGLs) were performed during endoscopic surveillance. The follow-up period was defined as the period between the ESD and the last surveillance endoscopy.
In surveillance endoscopies, dysplasia or cancer found at the previous ESD site within 1 year was defined as residual disease and after more than 1 year as local recurrence. SGL and MGL were defined as a new gastric neoplastic lesion that was detected during the first year and more than 1 year after ESD, respectively. Patients who did not undergo surveillance endoscopy were not considered for residual disease/local recurrence evaluation.
Statistical Analysis
Quantitative variables were presented as mean ± standard deviation or median and interquartile range (IQR) according to the presence of normal or non-normal distribution, respectively. Normality assessment was performed with the Shapiro-Wilk test (n < 50) and the Kolmogorov-Smirnov test (n ≥ 50). Categorical variables were analysed using the χ2 test or the Fisher exact test, while numerical variables were analysed with the Student t test or the Mann-Whitney test, according to the presence or not of normality in the sample. The cumulative incidence of MGL development and overall survival rate were plotted using the Kaplan-Meier method. The confidence level was 95% and statistical significance was set at p < 0.05. All statistical analyses were performed with SPSS (version 20.0; SPSS Inc., Chicago, IL, USA).
Results
A total of 105 patients with 114 gastric superficial epithelial neoplastic lesions underwent ESD during the 5-year period (from May 2012 to September 2017).
Baseline Characteristics
The patients’ demographic and clinicopathological characteristics are described in Table 1. Most lesions were flat (95.6%), specifically types 0-IIa and 0-IIa+IIc of the Paris classification, and were located in the antrum (54.4%), followed by middle (38.6%) and proximal stomach (7.0%). The median size of the lesions was 20.0 mm (IQR = 15; range, 5–60 mm). No ESD was performed for local recurrence of previous EMR.
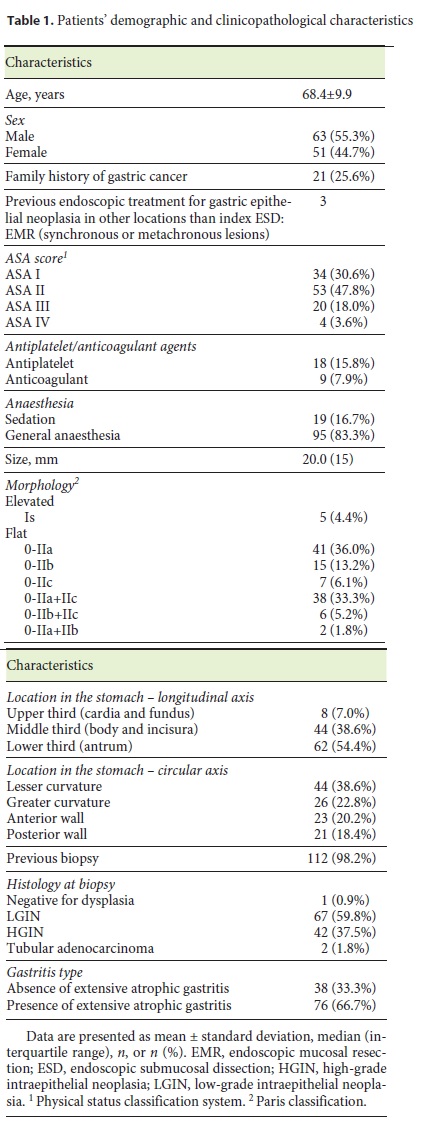
Two patients were submitted to ESD without a previous biopsy, all type 0-IIa lesions that fulfilled the absolute indication criteria, and the decision was based on the certainty of the endoscopic diagnosis with magnification and narrow-band imaging. Moreover, in one ESD of a lesion whose previous biopsy had been negative for dysplasia, the posterior histopathology analysis of the resected specimen showed differentiated mucosal adenocarcinoma.
Histological Features
En bloc resection was feasible in 96.5% (110/114), three were piecemeal resections (one of these in two pieces) and one ESD was not finished due to perforation (Table 2). R0 was achieved in 87.6% (99/113): 96.6% (60/62) in the absolute indication group and 79.1% (34/43) in the expanded indication group. One ESD specimen was lost due to distal migration, therefore complete resection could not be evaluated and it was excluded from R0/R1 assessment.
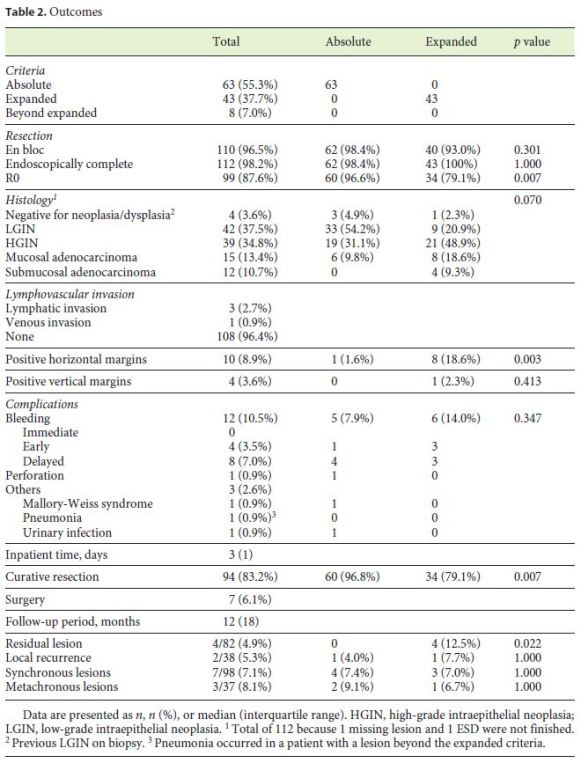
Eight resected lesions were classified beyond the expanded criteria. All of them were differentiated submucosal invasive cancers in which submucosal invasion was >500 µm or SM invasion was impossible to measure. Six of the lesions had a previous biopsy that showed only dysplasia and did not have morphologic features suggesting endoscopic unresectability. The other two were adenocarcinomas (on biopsy),
Adverse Events
Bleeding occurred in 12 procedures (10.5%): 4 cases of early bleeding (24 h) (Table 2). No significant immediate bleeding occurred during the procedures. All haemorrhages were treated endoscopically: single injection of a dilute solution of epinephrine (1:10,000) was used in 2 cases (16.7%); placement of endoclips with or without a previous epinephrine injection was performed in 8 cases (66.7%); 1 bleeding vessel was treated with adrenaline plus polidocanol injections (8.3%); and in 1 case (8.3%) the bleeding was controlled only after the use of haemostatic powder (Hemospray®; Cook Medical). Three patients needed blood transfusions, and 1 patient was admitted to the intensive care unit for 1 day because of haemorrhagic shock after ESD of a lesion located in the cardia. One perforation (0.9%) occurred during an ESD of a lesion in the cardia. The defect was successfully closed with endoclips, but the procedure was stopped since en bloc resection was compromised due to technical difficulties. The patient was subsequently referred for surgical treatment (gastrectomy). No procedure-related death was observed.
Short-Term Outcomes
Curative endoscopic resection was achieved in 83.2% of all patients. A positive HM was observed in 10 specimens (8.9%) and occurred more often in patients who did not fulfil the absolute indication criteria (Table 2). Dividing the study time into two periods, 2012–2015 and 2016–2017, a tendency towards improvement in HM results was found, although without statistical significance (11.9% [7/59] positive HM in 2012–2015 vs. 5.7% [3/53] in 2016–2017, Fisher exact test, p = 0.328). In a total of 10 patients with adenocarcinoma and non-curative endoscopic resection, 6 underwent surgical treatment with total or partial gastrectomy, but only 1 patient had residual neoplasia after histopathological assessment of the surgical specimen. In the 4 patients who were not submitted to surgery, one local recurrence was observed. It occurred in a patient with a previous fragmented resection and was successfully treated by endoscopy. One 90-year-old man with R1 resection (VM+ and HM+) and lymphovascular invasion refused any additional surveillance or treatment. Another patient with an R0 resection but with submucosal invasion >500 µm refused additional surgical treatment and remained under endoscopic and imaging follow-up without signs of disease recurrence. The last patient was considered unfit for surgical treatment (78-year-old male, ASA IV) and remains under endoscopic follow-up without any signs of disease recurrence and with two more lesions treated by ESD.
Long-Term Outcomes
During a median follow-up of 12 months (IQR = 18), 6 cases of recurrence were diagnosed: 4 residual lesions (1 intramucosal adenocarcinoma resected in piecemeal and 3 HGINs with R1 resections due to positive HM) and 2 local recurrences in previous R0 resections (1 minimally invasive submucosal adenocarcinoma and 1 LGIN). The recurrent tissue was dysplastic and non-invasive in all cases. Residual lesions were treated with argon plasma coagulation, one local recurrence with EMR, and the other local recurrence was lost to follow-up. Residual lesions were observed more often in patients with larger lesions and with positive HMs when compared to smaller lesions (median = 40.0 mm, IQR = 26 vs. median = 20.0 mm, IQR = 15, p = 0.008) and R0 resection (50.0 vs. 0.0%, Fisher exact test, p < 0.001), respectively.
Three patients had been previously submitted to EMR for other gastric epithelial neoplastic lesions in different locations. During the surveillance period, 7 SGLs were observed and 3 MGLs were identified (Table 2). The cumulative incidence of MGLs at 34 months was 16.1% (Fig. 3). All lesions were removed with a repeat ESD.
Overall survival was 96%, but disease-specific survival was 100%, with a median follow-up of 12 months (IQR = 18). Four patients died during the follow-up period due to non-cancer-related causes (cerebrovascular accident, cirrhosis decompensation, end-stage pulmonary disease, and sudden death).
Discussion
ESD is a technique which was introduced in the last decade in Western countries that implies a high level of expertise, with outcomes still slightly inferior to those from Eastern series [11].
The current study represents a retrospective description of superficial epithelial gastric neoplasias treated by ESD in a single centre and the second largest Portuguese case series report published [12–14]. The outcomes were similar to the results presented in the literature, with an en bloc R0 resection rate reaching 90% and a cure rate of >80%, with a good safety profile [14, 15]. All adverse events (10.5% rate of bleeding and 0.9% rate of perforation) were controlled endoscopically and none of the patients needed surgery. After resection, a careful inspection of the resection site was done along with prophylactic coagulation of all visible vessels. The ulcer was covered with sucralfate, a gastroprotective agent that directly binds the gastric submucosa in the ulcer bed, providing a physical barrier against gastric irritants. Although there is no evidence regarding the use of sucralfate in ESD, recent studies have employed sucralfate as a topical drug for the healing of several types of epithelial wounds such as ulcers, mucositis, and burn wounds [16, 17].
Fragmented resection and positive HM are associated with a rate of residual lesion and local recurrence of around 10–30% [3]. Although ESD allows a high en bloc resection rate, positive HMs are sometimes encountered (a Japanese multicentre survey reported 2% positive HMs in differentiated-type gastric adenocarcinomas). Appropriate treatment strategies for differentiated-type gastric cancers with positive HMs or indeterminable margins after ESD have not yet been established in guidelines [18]. Moreover, non-surgical options may be proposed due to a low risk of lymph node metastasis [3, 18]. In this study, a 4.9% rate of residual recurrence and a 5.3% rate of local recurrence were reported. In patients with positive HMs on resected specimens, 50% had residual disease, which is higher than in previous studies, even though all residual lesions were managed endoscopically [18, 19].
Some retrospective studies have tried to identify risk factors to positive HMs [19–21]. Kakushima et al. [20] reported three main reasons for positive HMs after resection: lesions with a flat spreading area not included in the marking, lesions with an unexpected nearby lesion, and lesions with lateral extension in the submucosa under a non-cancerous mucosa. After that, Sekiguchi et al. [19] identified a cancer-positive lateral margin length ≥6 mm as an independent risk factor for local recurrence after ESD (with a sensitivity and specificity for a 5-year risk of developing local recurrence of 66.7 and 95.6%, respectively). Recently, Numata et al. [21] recognised that location of the tumour in the upper third of the stomach and lesions not matching the absolute indication criteria were independent risk factors for positive HMs. In this study, expertise with digital chromoendoscopy improved along with the ESD learning curve, and the regular use of highdefinition endoscopy in the last period can partially explain highly positive HMs in the beginning. Secondly, no treatment was done in positive HMs before residual lesion detection. Maybe high-risk patients need to be treated promptly and the length of cancer-positive HM can help to decide which ones need additional treatment [19].
Two cases of R0 resections (minimally invasive submucosal adenocarcinoma and LGIN) developed local recurrence. After a careful revision of the endoscopic and histological records, male sex was identified in both cases as well as narrow lateral margin on the first lesion and extensive atrophic gastritis on the second, all risk factors for local recurrence [22, 23].
Patients without endoscopic curative resection criteria, besides positive HMs, were sent to surgery for curative treatment, but only 1 patient from those submitted to gastrectomy had residual neoplasia with lymph node metastasis after histopathological assessment. This study confirmed the low risk of lymph node metastasis in expanded criteria patients and ESD as the best staging tool before surgery for EGC [3, 9, 15]. However, when lesions were divided into two groups of indications (absolute versus expanded indications), the second group presented lower rates of R0 (96.6 vs. 79.1%, p = 0.007) and curative resection (96.8 vs. 79.1%, p = 0.007), with an increased residual lesion rate (0 vs. 13.3%, p = 0.024), confirming a recent meta-analysis [24], although endoscopically treatable in most of the cases.
Seven SGLs were detected during the first year, possibly missed before or at the time of the ESD, and 3 MGLs during the remaining follow-up period [25]. Regardless of endoscopic treatment being less invasive and associated with better quality of life compared to surgery, preservation of the stomach carries a greater risk of other gastric cancers. Some studies report an annual incidence of 1–3% for other gastric cancers, and the cumulative incidence of MGLs constantly increased, at least during the first 3–5 years [4, 14, 23, 25]. Recently, one retrospective study showed that patients with SGLs or male patients with extensive intestinal metaplasia have a high risk of MGLs even after 5 years [25]. So, endoscopic surveillance is necessary and short intervals (≤12 months) detect more endoscopically treatable lesions, decreasing the need for surgery [23, 25]. Currently, there is still not sufficient evidence to decide when to stop surveillance in patients submitted to ESD for EGC.
Overall survival was 96%, with four deaths during the follow-up period due to non-cancer-related causes, but disease-specific survival was 100%. This may be explained by the application of this endoscopic technique to many patients who seem unfit for major surgery due to old age or significant morbidities.
The study has some limitations. Firstly, the median follow-up was short and consequently the long-term outcomes should be interpreted with caution. Secondly, procedure duration, which could be a good tool to evaluate operator efficiency, was not evaluated, even though 83.2% of the lesions were successfully treated by ESD. Lastly, LGIN and HGIN (besides adenocarcinoma) were included in the study, and the results were compared with those of Eastern studies; however, the differences in histopathological classifications in Western and Eastern countries raise some questions regarding these comparisons.
In conclusion, the study results showed that ESD is an effective resection technique for gastric lesions with a good safety profile, confirming other European series. Regardless of a high en bloc resection, positive HM is still a problem in some specimens resected by ESD. Endoscopic surveillance could detect local recurrence and new lesions in early stages potentially treatable by endoscopy.
References
1 Uedo N, Takeuchi Y, Ishihara R: Endoscopic management of early gastric cancer: endoscopic mucosal resection or endoscopic submucosal dissection: data from a Japanese high-volume center and literature review. Ann Gastroenterol 2012;25:281–290. [ Links ]
2 Japanese Gastric Cancer Association: Japanese gastric cancer treatment guidelines 2014. Gastric Cancer 2017;20:1–19. [ Links ]
3 Pimentel-Nunes P, Dinis-Ribeiro M, Ponchon T, Repici A, Vieth M, De Ceglie A, et al: Endoscopic submucosal dissection: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy 2015;47:829–854. [ Links ]
4 Pimentel-Nunes P, Libânio D, Dinis-Ribeiro M: Evaluation and management of gastric superficial neoplastic lesions. GE Port J Gastroenterol 2017;24:8–21. [ Links ]
5 Japanese Gastric Cancer Association: Japanese gastric cancer treatment guidelines 2010. Gastric Cancer 2011;14:113–123. [ Links ]
6 Gotoda T, Yanagisawa A, Sasako M, Ono H, Nakanishi Y, Shimoda T, et al: Incidence of lymph node metastasis from early gastric cancer: estimation with a large number of cases at two large centers. Gastric Cancer 2000;3:219–225. [ Links ]
7 Hirasawa T, Gotoda T, Miyata S, Kato Y, Shimoda T, Taniguchi H, et al: Incidence of lymph node metastasis and the feasibility of endoscopic resection for undifferentiatedtype early gastric cancer. Gastric Cancer 2009;12:148–152. [ Links ]
8 Gotoda T, Iwasaki M, Kusano C, Seewald S, Oda I: Endoscopic resection of early gastric cancer treated by guideline and expanded National Cancer Centre criteria. Br J Surg 2010;97:868–871. [ Links ]
9 Suzuki H, Oda I, Abe S, Sekiguchi M, Mori G, Nonaka S, et al: High rate of 5-year survival among patients with early gastric cancer undergoing curative endoscopic submucosal dissection. Gastric Cancer 2016;19:198–205. [ Links ]
10 Yakirevich E, Resnick MB: Pathology of gastric cancer and its precursor lesions. Gastroenterol Clin North Am 2013;42:261–284. [ Links ]
11 Probst A, Pommer B, Golger D, Anthuber M, Arnholdt H, Messmann H: Endoscopic submucosal dissection in gastric neoplasia – experience from a European center. Endoscopy 2010;42:1037–1044. [ Links ]
12 Dinis-Ribeiro M, Pimentel-Nunes P, Afonso M, Costa N, Lopes C, Moreira-Dias L: A European case series of endoscopic submucosal dissection for gastric superficial lesions. Gastrointest Endosc 2009;69:350–355. [ Links ]
13 Rodrigues J, Carmo J, Carvalho L, Barreiro P, Chagas C: Endoscopic submucosal dissection for gastrointestinal superficial lesions: initial experience in a single Portuguese center. GE Port J Gastroenterol 2015;22:190–197. [ Links ]
14 Pimentel-Nunes P, Mourão F, Veloso N, Afonso LP, Jácome M, Moreira-Dias L, et al: Long-term follow-up after endoscopic resection of gastric superficial neoplastic lesions in Portugal. Endoscopy 2014;46:933–940. [ Links ]
15 Tanabe S, Hirabayashi S, Oda I, Ono H, Nashimoto A, Isobe Y, et al: Gastric cancer treated by endoscopic submucosal dissection or endoscopic mucosal resection in Japan from 2004 through 2006: JGCA nationwide registry conducted in 2013. Gastric Cancer 2017;20:834–842. [ Links ]
16 Itoh T, Kusaka K, Kawaura K, Kashimura K, Yamakawa Y, Takahashi T, et al: Selective binding of sucralfate to endoscopic mucosal resection-induced gastric ulcer: evaluation of aluminium adherence. J Int Med Res 2004;32:520–529. [ Links ]
17 Masuelli L, Tumino G, Turriziani M, Modesti A, Bei R: Topical use of sucralfate in epithelial wound healing: clinical evidence and molecular mechanisms of action. Recent Pat Inflamm Allergy Drug Discov 2010;4:25–36. [ Links ]
18 Ishii N, Omata F, Fujisaki J, Hirasawa T, Kaise M, Hoteya S, et al: Management of early gastric cancer with positive horizontal or indeterminable margins after endoscopic submucosal dissection: multicenter survey. Endosc Int Open 2017;5:E354–E362. [ Links ]
19 Sekiguchi M, Suzuki H, Oda I, Abe S, Nonaka S, Yoshinaga S, et al: Risk of recurrent gastric cancer after endoscopic resection with a positive lateral margin. Endoscopy 2014;46:273–278. [ Links ]
20 Kakushima N, Ono H, Tanaka M, Takizawa K, Yamaguchi Y, Matsubayashi H: Factors related to lateral margin positivity for cancer in gastric specimens of endoscopic submucosal dissection. Dig Endosc 2011;23:227–232. [ Links ]
21 Numata N, Oka S, Tanaka S, Kagemoto K, Sanomura Y, Yoshida S, et al: Risk factors and management of positive horizontal margin in early gastric cancer resected by en bloc endoscopic submucosal dissection. Gastric Cancer 2015;18:332–338. [ Links ]
22 Yun GW, Kim JH, Lee YC, Lee SK, Shin SK, Park JC, et al: What are the risk factors for residual tumor cells after endoscopic complete resection in gastric epithelial neoplasia? Surg Endosc 2015;29:487–492. [ Links ]
23 Hahn KY, Park JC, Kim EH, Shin S, Park CH, Chung H, et al: Incidence and impact of scheduled endoscopic surveillance on recurrence after curative endoscopic resection for early gastric cancer. Gastrointest Endosc 2016;84:628–638. [ Links ]
24 Peng LJ, Tian SN, Lu L, Chen H, Ouyang YY, Wu YJ: Outcome of endoscopic submucosal dissection for early gastric cancer of conventional and expanded indications: systematic review and meta-analysis. J Dig Dis 2015;16:67–74. [ Links ]
25 Yang HJ, Kim SG, Lim JH, Choi JM, Oh S, Park JY, et al: Novel risk stratification for metachronous recurrence after curative endoscopic submucosal dissection for early gastric cancer. Gastrointest Endosc 2018;87:419–428.e3. [ Links ]
Statement of Ethics
All patients were informed about the risks and benefits of the procedure and written informed consent was obtained prior to ESD. This study was conducted in accordance with the ethical principles of the Declaration of Helsinki and in compliance with good clinical practice.
Disclosure Statement
The authors have no conflicts of interest to declare.
* Corresponding author.
Dr. Rita Seara Costa
Departamento de Gastrenterologia, Hospital de Braga
Sete Fontes – São Victor
PT–4710-243 Braga (Portugal)
E-Mail rita.seara.costa@gmail.com
Received: November 23, 2017; Accepted after revision: February 12, 2018














