Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.26 no.3 Lisboa jun. 2019
https://doi.org/10.1159/000492313
ORIGINAL ARTICLE
Risk Factors for Post-Endoscopic Retrograde Cholangiopancreatography Pancreatitis in the Indomethacin Era – A Prospective Study
Fatores de Risco para a Pancreatite pós-Colangiopancreatografia Retrógrada Endoscópica na Era da Indometacina – Um Estudo Prospetivo
David N. Perdigotoa,b, Dário Gomesa,b, Nuno Almeidaa,b, Sofia Mendesa, Ana Rita Alvesa, Ernestina Camachoa, Luís Toméa,b
aGastroenterology Department, Coimbra Hospital and University Center, Coimbra, Portugal; bMedical School, Coimbra University, Coimbra, Portugal
* Corresponding author.
ABSTRACT
Background and Aims: Although endoscopic retrograde cholangiopancreatography (ERCP) is an essential procedure used to treat conditions affecting the biliopancreatic system, it can lead to several complications. Post-ERCP pancreatitis (PEP) is the most frequent one, with an incidence ranging from 3 to 14%. Our aim was to assess the potential risk factors associated with PEP occurrence in patients undergoing ERCP with indomethacin prophylaxis. Methods: Prospective, single-center, real-world observational study (January to December 2015) with inclusion of patients submitted to ERCP, where relevant patient-related and procedure-related data had been collected. Patients had to have been admitted for a minimum of 24 h in order to establish the presence of early complications. All patients were submitted to PEP prophylaxis with 1 or 2 methods: rectal indomethacin and pancreatic duct (PD) stenting. Results: A total of 188 patients who had undergone ERCP were included (52.7% women; mean age 69.2 ± 16.0 years) and PEP was diagnosed in 13 (6.9%). PEP prophylaxis consisted of indomethacin in all cases (100%) and PD stenting in 7.4%. The pancreatitis was mild in 11 patients (84.6%) and severe in the other 2. One of them died (0.5%). None of the patient-related risk factors were associated with changes in PEP probability. Of all patients, 33.0% had 2 or more procedure-related risk factors. A higher number of synchronous procedure-related risk factors showed a statistically significant correlation with PEP occurrence, p = 0.040. Conclusions: The 6.9% PEP rate is considered acceptable since 33.0% patients had a medium-high risk for PEP due to challenging biliary cannulation. The total number of procedure-related risk factors seems to play a critical role in the development of PEP despite indomethacin prophylaxis.
Keywords: Endoscopic retrograde cholangiopancreatography, Post-ERCP pancreatitis, Indomethacin, Pancreatic duct stent, ERCP complications
RESUMO
Introdução e objetivo: A colangiopancreatografia retrógrada endoscópica (CPRE) é um método terapêutico crucial em doenças biliopancreáticas, mas pode levar a várias complicações. A pancreatite pós-CPRE (PPC) é a complicação mais frequente, podendo atingir uma incidência de 3 a 14%. O objetivo foi estudar os fatores de risco associados à PPC em doentes submetidos a CPRE com profilaxia por indometacina. Métodos: Estudo prospetivo e observacional com inclusão (janeiro-dezembro 2015) de doentes submetidos a CPRE num centro terciário, em condições de prática real. Foram registados os dados relevantes do doente e procedimento. Os doentes foram observados em internamento por, pelo menos, 24 horas para deteção de complicações. Todos os doentes incluídos foram submetidos a profilaxia de PPC, com recurso a um ou dois métodos: indometacina retal e prótese pancreática. Resultados: Estudados 188 doentes, 52.7%mulheres, com idade média de 69.2 ± 16.0 anos. Profilaxia de PPC envolveu indometacina em todos os casos (100%) e colocação de prótese pancreática em 7.4%. Registou-se PPC em 13 doentes (6.9%), sendo que 11 (84.6% de PPC) tiveram pancreatite ligeira. Os restantes dois apresentaram pancreatite grave e um deles faleceu (0.5%). Nenhum dos fatores de risco do doente se relacionou com maior probabilidade de PPC. Do total de doentes, em 33.0% estiveram presentes 2 ou mais fatores de risco associados ao procedimento. A presença simultânea de um número superior de fatores de risco associados ao procedimento relacionou-se significativamente com a ocorrência de PPC, p = 0.040. Conclusões: Considera-se aceitável a taxa de PPC de 6.9%, tendo em conta que 33.0% dos doentes apresentavam risco médio-alto para PPC devido a canulação biliar difícil. O número total de fatores de risco associados ao procedimento parece desempenhar um papel crucial no desenvolvimento de PPC, apesar da profilaxia com indometacina.
Palavras-Chave: CPRE, Pancreatite pós-CPRE, Indometacina, Prótese pancreática, Complicações de CPRE
Introduction
Endoscopic retrograde cholangiopancreatography (ERCP) is a crucial method for treatment of multiple biliopancreatic conditions [1]. This procedure can lead to several complications, post-ERCP pancreatitis (PEP) being the most common, with an incidence ranging from 3 to 14% [2–5]. Although the severity is mild to moderate in most cases of PEP, the rate of severe episodes is worrisome since it can reach 8–10% of PEP cases [6]. In fact, the death rate related to PEP is estimated to be 3% [2], which, when combined with a mean 4% rate of PEP incidence, anticipates a predicted 1.2 deaths per thousand patients submitted to ERCP.
Due to this dismal perspective, different groups have investigated potential strategies to reduce the occurrence of PEP. Several pharmacologic agents have been evaluated and tested as potential protectors against this complication [7–13]. Somatostatin is one of the most studied but, after promising initial trials, a meta-analysis demonstrated a less important role for this drug [14]. Afterwards, nonsteroidal anti-inflammatory drugs came up as potential PEP-preventive agents [15–17]. Among this group, rectal indomethacin gained more notoriety based on convincing evidence [18]. Since its first use 10 years ago, rectal indomethacin has progressively been accepted as a simple and easy to administer preventive measure. Therefore, it has been commonly adopted in most endoscopic units.
Additionally, prophylactic pancreatic duct (PD) stent placement after PD inadvertent cannulation and in highrisk patients was also investigated as an effective preventive measure [19, 20].
A rigorous selection of patients, guidewire-assisted cannulation technique, PD stenting if appropriate, use of rectal indomethacin (or diclofenac), and more recently, aggressive intravenous hydration are all regarded as the main prophylactic tools to prevent PEP according to current guidelines [21, 22].
The main aim of this study was to assess which patient-related and procedure-related risk factors were present and associated with PEP development in a cohort of patients that underwent ERCP and were submitted to rectal indomethacin prophylaxis. Secondly, we sought to evaluate the precise PEP rate in a tertiary center’s endoscopic unit by performing a quality assessment on a reallife basis.
Methods
Study Design and Exclusion Criteria
A prospective, 12-month (January to December 2015), singlecenter, observational study was designed. For each ERCP conducted in the endoscopic unit of a tertiary referral center, relevant data concerning patient-related and procedure-related risk factors were collected. All the essential information was registered before and after the procedure in a standard form. The patient was then followed up for at least 24 h to evaluate the occurrence of complications.
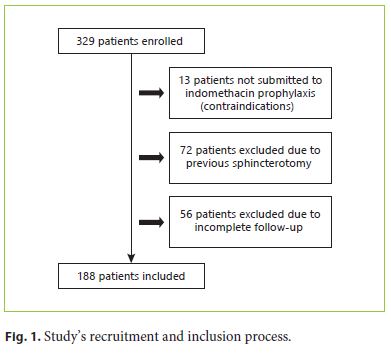
Concerning exclusion criteria, patients previously submitted to a biliary sphincterotomy (not-naïve papilla), patients in whom prophylactic measures were not done, patients with insufficient clinical data, and/or without appropriate follow-up were excluded. Most excluded patients had been referred by another medical institution. The incorporation process is detailed in Figure 1.
During the 24-h in-hospital follow-up, the patient was carefully evaluated by the assistant physician or, whenever necessary, by the department’s emergency doctor. Since PEP is considered a predominantly clinical diagnosis, if there was any slight clinical suspicion of PEP, appropriate laboratory investigation including C-reactive protein, amylase, and lipase parameters was done to screen for possible pancreatitis. The teams performing ERCP included an endoscopist with at least 150 ERCPs performed per year and 10 or more years of experience, an endoscopy nurse adequately skilled in the technique, and a trainee physician.
PEP and Severity Grade Definitions
PEP was defined as a new onset of abdominal pain or a worsening of an existing one, associated with an increase in amylase or lipase more than 3 times the upper cutoff value. This definition was based on the original one by Cotton et al. [23].
The severity of pancreatitis was graded according to the 2012 revised Atlanta classification [24]. Thus, mild PEP was present in the absence of organ failure, and local or systemic complications. Moderately severe PEP was characterized by organ failure that resolved within 48 h (transient organ failure) or local or systemic complications without persistent organ failure. Severe PEP was defined by persistent organ failure (> 48 h duration). Organ failure was classified according to the modified Marshal organ dysfunction criteria [24].
Patient-Related/Procedure-Related Risk Factors and Prophylactic Measures
The patient-related risk factors assessed were female gender, normal bilirubin value (institution’s cutoff of 1.2 mg/dL), patients’ age less than 40 years old, and history of acute pancreatitis or PEP. Previous history of suspected sphincter of Oddi dysfunction was not considered.
The guidewire-assisted technique for biliary cannulation was systematically performed, and a pancreatic guidewire-assisted technique was used whenever necessary after unintentional PD cannulation.
During the ERCP, every potential procedure-related risk factor was recorded. The following were registered: the duration and number of attempts to cannulate the common biliary duct, inadvertent cannulation of the main PD (considered when at least 1 PD cannulation was done) with and without contrast injection, transpancreatic septotomy (transpancreatic biliary sphincterotomy), execution of needle-knife precut sphincterotomy, and papillary balloon dilation (before sphincterotomy). The total number of procedure-related risk factors was considered as a single specific risk factor itself to test the potential synergism connected to the presence of multiple factors. Regarding this issue, the number of biliary cannulation attempts was considered as a risk factor when 4 or more tries were necessary for effective biliary cannulation since current European guidelines were only available in 2016 [1]. Concerning the duration of the cannulation process, it was considered a risk factor whenever it lasted for 5 min or more.
All included patients were treated with prophylactic 100 mg rectal indomethacin immediately after the procedure.
A prophylactic pancreatic stent (5 Fr) was placed after inadvertent PD cannulation, mainly when 2/3 cannulations occurred. The decision to place the PD stent was made individually by the endoscopist according to the global patient’s risk. Additionally, a PD stent was also placed after most cases of transpancreatic septotomy.
Prophylactic aggressive hydration was not performed, and therefore not evaluated as a specific preventive measure because, at the time the study was designed, there was not enough clear evidence to justify its use.
Statistical Analysis
Categorical variables were expressed as absolute number with correspondent percentage and continuous variables as the mean ± standard deviation (SD) with the median, quartile 1, and quartile 3 (Q1–Q3) if they showed non-normal distribution.
Categorical variables were compared with the χ2 test and Fisher’s exact test whenever any group had less than 20 elements. Normality was assessed with Kolmogorov-Smirnov and Shapiro-Wilk tests. Due to non-normal distribution, continuous variables were compared with the Mann-Whitney U test, and correlations were studied with a Spearman’s rho correlation for univariate analysis. Multivariate analysis for a hypothetical model was conducted with binary logistic regression after univariate analysis tests for individual relevant variables to integrate the model. Statistical significance was considered as a p value < 0.05.
The statistical study was carried out with SPSS (SPSS v.20 for OS; Chicago, IL, USA).
Ethical Considerations
This was a prospective observational study with no interference on clinical decision-making, prevention, and treatment. Therefore, formal approval from the institution’s ethical committee was waived due to the exclusively observational nature of the study. All the enrolled patients signed the proper department’s consent form for all endoscopic procedures, and for data recording as well. The patients’ confidentiality and anonymity were kept. Only the study’s investigators had access to the patients’ clinical data. All the principles stated in the Helsinki Declaration were fulfilled.
Results
PEP Rate
A total of 329 ERCPs with adequate procedure data, corresponding to the same number of patients, were enrolled. Due to the absence of indomethacin prophylaxis, previous biliary sphincterotomy, and incomplete followup, a total of 141 patients were excluded (Fig. 1). Thus, 188 procedures were eligible for analysis.
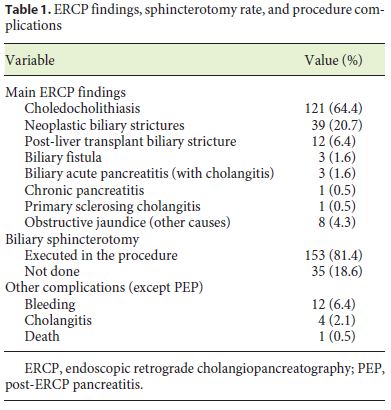
Of the studied patients, 99 (52.7%) were women. The patients’ mean age was 69.2 ± 16.0, ranging from 20 to 95 years. The ERCP main findings and complications observed are expressed in Table 1. Biliary sphincterotomy was not done, mostly in patients with post-liver transplant biliary stricture and in septic patients due to acute cholangitis where a temporary stent was used until a deferred procedure.
The continuous variables age, bilirubin, number of biliary cannulation attempts, duration of cannulation attempts, and the total number of risk factors showed a non-normal distribution, p < 0.0001 for both the Kolmogorov-Smirnov and Shapiro-Wilk tests.
The primary outcome, PEP, was present in 13 patients (6.9%). Within the PEP cases, 11 (84.6%) had mild pancreatitis. The other 2 patients experienced severe PEP; there were no patients with a moderate degree of PEP. There were no statistical differences in the PEP rate among different endoscopists. The patients that experienced pancreatitis were admitted for a mean period of 5.2 ± 4.2 days. The 2 patients with severe PEP required intensive care treatment, and one of them died, corresponding to a 0.5% global mortality rate. This death concerned an 87-year-old woman who had undergone ERCP due to suspicion of common biliary duct lithiasis. She had several comorbidities such as congestive heart failure, type 2 diabetes mellitus, hypertension, obesity, and atrial fibrillation.
With regard to preventive measures, besides indomethacin, pancreatic prophylactic stenting was used in 14 cases (7.4%), and only 1 of these patients developed PEP. When compared to the PEP rate in patients without PD stenting, the difference was not statistically significant, p = 1.0. The patient who developed PEP had had a challenging biliary cannulation that had required an elevated number of attempts, during a long period of time, and needle-knife precut, resulting in a total of 4 procedurerelated risk factors (including PD cannulation). Despite the prophylaxis with both PD stenting and indomethacin, the patient developed mild PEP.
Risk Factors
Concerning the risk factors, none of the patient-related factors was connected to a higher probability of PEP (Table 2). A normal value of bilirubin (≤1.2 mg/ dL), when compared to any value greater than this cutoff, was associated with a higher probability of PEP, 9.5 versus 4.8%, respectively. However, this difference was not statistically significant, p = 0.253. The number of patient-related risk factors was not associated with a higher risk of PEP, p = 0.561 (Table 2). There was no previous history of acute pancreatitis or PEP in the included patients.
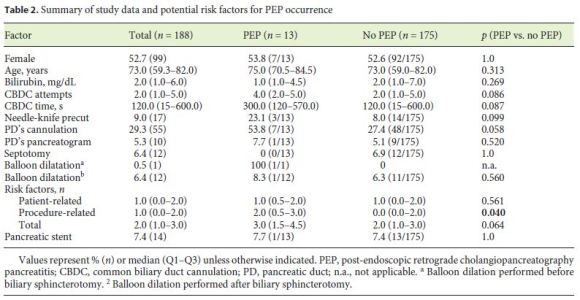
Regarding the single procedure-related risk factors, none of them showed statistical significance for PEP development (Table 2). Nevertheless, a number of biliary cannulation attempts higher than 3, when compared to 3 or less, was associated with a higher PEP rate, 13.8 versus 3.8%, respectively, p = 0.025, with an odds ratio of 2.15 (95% confidence interval: 1.32–3.51). The duration of biliary cannulation attempts was longer in the PEP group, but this difference was not relevant (Table 2).
The sum of the procedure-related risk factors evidenced a statistically significant connection with PEP occurrence, p = 0.040. There were 62 patients (33.0%) with 2 or more procedure-related risk factors. Within this group, the PEP rate was 11.3% (7/62) compared to a 4.8% rate in the remaining patients (6/126), p = 0.126. Additionally, the total number of factors, combining patient related and procedure-related, did not correlate with higher PEP rate, p = 0.064.
Sphincter of Oddi balloon dilatation before biliary sphincterotomy was performed only in one procedure, and therefore no statistical study could be done. Balloon dilatation performed immediately after biliary sphincterotomy showed no connection with PEP occurrence (Table 2).
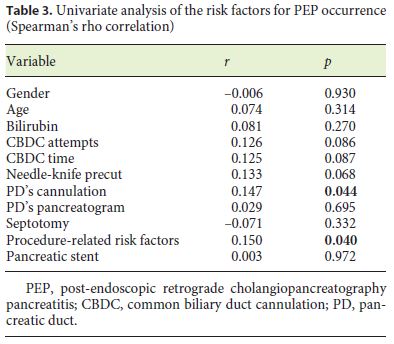
A univariate analysis with Spearman’s rho correlation was done to identify isolated risk factors. Only PD cannulation and the total number of procedure-related risk factors showed a statistical correlation with PEP development (Table 3). These 2 factors were then studied in a multivariate model and showed no significance for PEP prediction.
Transpancreatic septotomy was done in 12 patients (6.4%), and none of them developed PEP. However, this difference was not relevant.
Other Complications
Besides PEP, there were also other ERCP complications. Bleeding occurred in 12 cases (6.4%). In 4 cases, no treatment was necessary since the bleeding ceased spontaneously. In the other 8 cases, it was successfully treated with an adrenaline injection and endoclip placement. Cholangitis occurred in 4 cases (2.1%); all patients were successfully treated with antibiotics.
Discussion
Global Analysis and PEP Rate
The PEP frequency in our study (6.9%) is within the range normally observed in the published literature. Although most studies report an incidence rate closer to 4%, it is known that PEP occurrence can reach values as high as 14% in high-risk patients [4].
One-third of our cohort (33.0%) consisted of patients with 2 or more procedure-related risk factors due to challenging biliary cannulation. The presence of this group with a medium-high risk for PEP occurrence can partially justify our PEP rate, which we consider to be acceptable in such context.
Because most of the patients (84.6%) developed mild PEP, a reasonable inference would be that indomethacin might reduce the severity of pancreatitis. However, the absence of a control group does not allow this conclusion. Nevertheless, there is consolidated evidence that highlights this role of indomethacin [25, 26].
Prophylactic Measures
All patients were treated with prophylactic indomethacin. In this context, we had anticipated a lower PEP rate of about 4–5%. The higher rate identified is probably due to the fact that indomethacin can only partially reduce the occurrence of PEP. Unfortunately, a certain PEP risk is inevitable, particularly in patients with difficult biliary cannulation who therefore require more complex and hazardous ERCP techniques. Thus, when compared to the patients with less than 2 factors, the group of patients with several procedure-related risk factors (2 or more) showed a higher PEP rate, despite not being statistically significant.
In addition to indomethacin, PD prophylactic stenting was adopted to reduce PEP development. This procedure did not have an objective protective impact. Although the preventive potential of this method has been established [27], it is possible that no effect was observed due to the fact that only 14 patients were treated with PD stenting. Additionally, this kind of stent was used when repeated pancreatic cannulation has occurred and therefore a higher PEP probability is expected. Consequently, a considerable bias likely exists. In this context, the observed PEP rate of 7.7% in patients submitted to PD stent placement is considered acceptable.
Isolated Risk Factors and Their Specific Role
Because none of the patient-related risk factors showed a significant relationship to PEP occurrence, we might infer that, while their hazardous capacity to elevate the PEP tendency is well known [21], in our study their role was less relevant when compared to the procedure-related factors.
The fact that other factors such as suspected sphincter of Oddi dysfunction were not considered might have affected the results concerning patient-related risk factors. Although the number of biliary cannulation attempts did not correlate with PEP occurrence, a value higher than 3 was associated with an increased PEP rate. This cutoff is in line with current recommendations that advise limiting the papilla trauma [1]. Therefore, alternative techniques like early needle-knife fistulotomy or transpancreatic septotomy should be considered by experienced endoscopists to reduce the PEP risk in cases of challenging biliary cannulation [1].
Balloon dilatation executed after biliary sphincterotomy was not associated as expected with PEP occurrence, substantiating the concept that only balloon dilation with an intact sphincter is dangerous [21].
Only the total number of procedure-related risk factors showed a significant association with a higher PEP risk. Additionally, univariate analysis revealed a correlation also for PD cannulation. This apparent contradiction is justified by the lower number of PEP occurrences, forcing the adoption of a Fisher’s exact test to improve accuracy in the analysis. Consequently, only the number of procedure-related factors should be interpreted as significant.
The correlation coefficients in the univariate analysis were quite low for both factors (< 0.2). Accordingly, the absence of relevance of the multivariate study is not surprising.
Overall, our results suggest that, in patients being submitted to PEP prophylaxis with indomethacin, the presence of several synchronous procedure-related risk factors might be the most relevant trigger for PEP occurrence. This supports the known synergism that occurs when several procedure-related risk factors are combined [28].
Notably, PD cannulation and not unintentional pancreatogram (contrast injection) correlated with PEP occurrence. This suggests that independent of contrast use, PD cannulation must be avoided. Moreover, if PD cannulation occurs, a low threshold for PD stenting is recommended as stated in recent guidelines [1]. These results are also consistent with previous evidence that defined a higher odds ratio for PEP development with PD cannulation compared to the one associated with PD injection [21].
In contrast to needle-knife precut, the group of patients submitted to transpancreatic septotomy had no cases of PEP. The absence of statistical significance, probably due to the small sample size, does not allow for specific conclusions. As this is an evolving topic, future randomized studies comparing septotomy to other methods in the setting of difficult biliary cannulation would be useful.
Our study has several limitations. Since PEP is an uncommon occurrence, the study sample (n = 188) is insufficient to draw more striking conclusions about the different risk factors. The considerable number of excluded patients influenced the results.
Only objectively confirmed patient-related factors were assumed. While these criteria increased the accuracy of our study, they may have restricted the analysis of patient-related risk factors. Additionally, because several endoscopists were involved, it is not possible to exclude some inconsistency in data recording.
Conclusion
In conclusion, this study shows a PEP rate of 6.9% in a tertiary referral center, which is considered acceptable given that 33.0% patients had a medium-high risk for PEP. Even with indomethacin prophylaxis, there is still an inevitable certain percentage of PEP development probability, particularly for patients with medium-high risk.
The total number of procedure-related risk factors seems to play a critical role in the development of PEP despite indomethacin prophylaxis. In patients with one or more procedure-related risk factors, other prophylactic measures such as PD stenting should be systematically implemented. Future studies should focus on new prophylactic measures like standard early aggressive hydration and the evaluation of more complex patient-related risk factors.
References
1 Testoni PA, Mariani A, Aabakken L, et al: Papillary cannulation and sphincterotomy techniques at ERCP: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy 2016;48:657–683. [ Links ]
2 Andriulli A, Loperfido S, Napolitano G, et al: Incidence rates of post-ERCP complications: a systematic survey of prospective studies. Am J Gastroenterol 2007;102:1781–1788. [ Links ]
3 Kapral C, Mühlberger A, Wewalka F, et al: Quality assessment of endoscopic retrograde cholangiopancreatography: results of a running nationwide Austrian benchmarking project after 5 years of implementation. Eur J Gastroenterol Hepatol 2012;24:1447–1454. [ Links ]
4 Kochar B, Akshintala VS, Afghani E, et al: Incidence, severity, and mortality of post-ERCP pancreatitis: a systematic review by using randomized, controlled trials. Gastrointest Endosc 2015;81:143–149. [ Links ]
5 Masci E, Mariani A, Curioni S, et al: Risk factors for pancreatitis following endoscopic retrograde cholangiopancreatography: a metaanalysis. Endoscopy 2003;35:830–834. [ Links ]
6 Sutton VR, Hong MK, Thomas PR: Using the 4-h Post-ERCP amylase level to predict postERCP pancreatitis. JOP 2011;12:372–376. [ Links ]
7 Devière J, Le Moine O, Van Laethem JL, et al: Interleukin 10 reduces the incidence of pancreatitis after therapeutic endoscopic retrograde cholangiopancreatography. Gastroenterology 2001;120:498–505. [ Links ]
8 Arcidiacono R, Gambitta P, Rossi A, et al: The use of a long-acting somatostatin analogue (octreotide) for prophylaxis of acute pancreatitis after endoscopic sphincterotomy. Endoscopy 1994;26:715–718. [ Links ]
9 Andriulli A, Clemente R, Solmi L, et al: Gabexate or somatostatin administration before ERCP in patients at high risk for post-ERCP pancreatitis: a multicenter, placebo-controlled, randomized clinical trial. Gastrointest Endosc 2002;56:488–495. [ Links ]
10 Prat F, Amaris J, Ducot B, et al: Nifedipine for prevention of post-ERCP pancreatitis: a prospective, double-blind randomized study. Gastrointest Endosc 2002;56:202–208. [ Links ]
11 Budzyńska A, Marek T, Nowak A, et al: A prospective, randomized, placebo-controlled trial of prednisone and allopurinol in the prevention of ERCP-induced pancreatitis. Endoscopy 2001;33:766–772. [ Links ]
12 Rabenstein T, Fischer B, Wiessner V, et al: Low-molecular-weight heparin does not prevent acute post-ERCP pancreatitis. Gastrointest Endosc 2004;59:606–613. [ Links ]
13 Poon RT, Yeung C, Liu CL, et al: Intravenous bolus somatostatin after diagnostic cholangiopancreatography reduces the incidence of pancreatitis associated with therapeutic endoscopic retrograde cholangiopancreatography procedures: a randomised controlled trial. Gut 2003;52:1768–1773. [ Links ]
14 Andriulli A, Leandro G, Federici T, et al: Prophylactic administration of somatostatin or gabexate does not prevent pancreatitis after ERCP: an updated meta-analysis. Gastrointest Endosc 2007;65:624–632. [ Links ]
15 Sotoudehmanesh R, Khatibian M, Kolahdoozan S, et al: Indomethacin may reduce the incidence and severity of acute pancreatitis after ERCP. Am J Gastroenterol 2007;102:978–983. [ Links ]
16 Cheon YK, Cho KB, Watkins JL, et al: Efficacy of diclofenac in the prevention of post-ERCP pancreatitis in predominantly high-risk patients: a randomized double-blind prospective trial. Gastrointest Endosc 2007;66:1126–1132. [ Links ]
17 Elmunzer BJ, Waljee AK, Elta GH, et al: A meta-analysis of rectal NSAIDs in the prevention of post-ERCP pancreatitis. Gut 2008;57:1262–1267. [ Links ]
18 Elmunzer BJ, Scheiman JM, Lehman GA, et al: A randomized trial of rectal indomethacin to prevent post-ERCP pancreatitis. N Engl J Med 2012;366:1414–1422. [ Links ]
19 Tarnasky PR, Palesch YY Cunningham JT, et al: Pancreatic stenting prevents pancreatitis after biliary sphincterotomy in patients with sphincter of Oddi dysfunction. Gastroenterology 1998;115:1518–1524. [ Links ]
20 Mazaki T, Masuda H, Takayama T: Prophylactic pancreatic stent placement and postERCP pancreatitis: a systematic review and meta-analysis. Endoscopy 2010;42:842–853. [ Links ]
21 Dumonceau JM, Andriulli A, Elmunzer BJ, et al: Prophylaxis of post-ERCP pancreatitis: European Society of Gastrointestinal Endoscopy (ESGE) Guideline – updated June 2014. Endoscopy 2014;46:799–815. [ Links ]
22 Chandrasekhara V, Khashab MA, Muthusamy VR, et al: Adverse events associated with ERCP. Gastrointest Endosc 2017;85:32–47. [ Links ]
23 Cotton PB, Lehman G, Vennes J, et al: Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc 1991;37:383–393. [ Links ]
24 Banks PA, Bollen TL, Dervenis C, et al: Classification of acute pancreatitis – 2012: revision of the Atlanta classification and definitions by international consensus. Gut 2013;62:102–111. [ Links ]
25 Ding X, Chen M, Huang S, et al: Nonsteroidal anti-inflammatory drugs for prevention of post-ERCP pancreatitis: a meta-analysis. Gastrointest Endosc 2012;76:1152–1159. [ Links ]
26 Sethi S, Sethi N, Wadhwa V, et al: A metaanalysis on the role of rectal diclofenac and indomethacin in the prevention of post-endoscopic retrograde cholangiopancreatography pancreatitis. Pancreas 2014;43:190–197. [ Links ]
27 Mazaki T, Mado K, Masuda H, et al: Prophylactic pancreatic stent placement and postERCP pancreatitis: an updated meta-analysis. J Gastroenterol 2014;49:343–355. [ Links ]
28 Cotton PB, Garrow DA, Gallagher J, et al: Risk factors for complications after ERCP: a multivariate analysis of 11,497 procedures over 12 years. Gastrointest Endosc 2009;70:80–88. [ Links ]
Statement of Ethics
Formal approval from the institution’s ethical committee was waived due to the exclusively observational nature of the study. All the enrolled patients signed the proper department’s consent form for all endoscopic procedures, and for data recording as well.
Disclosure Statement
The authors declare no conflicts of interest
* Corresponding author.
Dr. David N. Perdigoto
Gastroenterology Department, Coimbra Hospital and University Center
Praceta Prof. Mota Pinto
PT–3000-075 Coimbra (Portugal)
E-Mail davidperdigoto@gmail.com
Received: January 24, 2018; Accepted after revision: July 23, 2018














