Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.26 no.3 Lisboa jun. 2019
https://doi.org/10.1159/000488605
IMAGES IN GASTROENTEROLOGY AND HEPATOLOGY
Lower Gastrointestinal Bleeding: Liver Rams into Gut!
Hemorragia digestiva baixa: Fígado contra o intestino!
Amit Soni, Nirmaljeet Singh Malhi
Department of Gastroenterology and Liver Disease, SPS Hospital, Ludhiana, India
* Corresponding author.
Keywords: Colon, Hepatocellular carcinoma, Lower gastrointestinal bleeding
Palavras-Chave: Cólon, Carcinoma hepatocelular, Hemorragia digestiva baixa
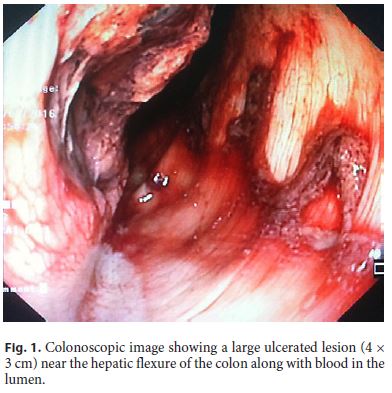
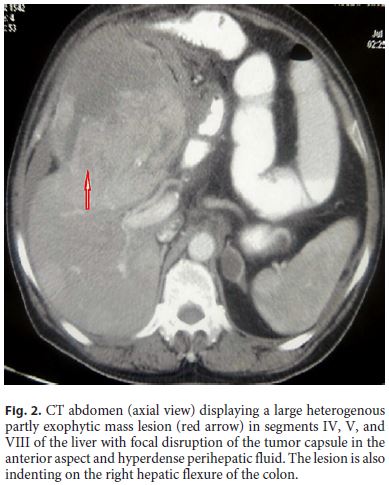
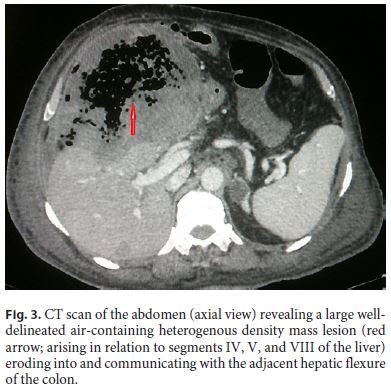
A 65-year-old male patient presented to the emergency department with bleeding per rectum for 1 day. He was diagnosed with hepatitis C virus-related chronic liver disease (decompensated) with hepatocellular carcinoma (HCC) (BCLC stage D) 3 months back and was on symptomatic treatment. On examination, the patient had tachycardia (pulse rate, 116/min; blood pressure, 90/50 mm Hg), pallor, and icterus. Abdominal examination revealed a large mass in the right upper quadrant. Laboratory tests were as follows: Hb, 5.8 g/dL; TLC, 20.4 × 109/L; platelets, 90 × 109/L; total bilirubin, 100.8 µmol/L; serum albumin, 22 g/L; SGOT, 120 IU/L; SGPT, 54 IU/L; INR, 2; AFP, 633 ng/mL; urea, 34.9 mmol/L; and creatinine, 136.1 µmol/L. After initial hemodynamic stabilization, a colonoscopy was performed. Colonoscopy documented a large ulcerated lesion (4 × 3 cm) near the hepatic flexure suggesting a malignant nature (Fig. 1). Multiple biopsies were taken from the ulcer margin. His previous computed tomography (CT) scan of the abdomen revealed a large heterogeneous, partly exophytic mass lesion (12 × 7 × 6 cm) in the liver segments IV, V, and VIII with focal disruption of the tumor capsule in the anterior aspect and hyperdense perihepatic fluid (Fig. 2). The lesion was indenting on the right hepatic flexure of the colon. A repeat CT scan of the abdomen was performed, which revealed a large well-delineated air-containing heterogeneous density mass lesion (arising in relation to the liver segments IV, V, and VIII) eroding into and communicating with the adjacent hepatic flexure of the colon (Fig. 3). Multiple well-delineated heterogeneously enhancing hepatic masses of varying sizes were also seen in both liver lobes. Histopathology confirmed the presence of HCC. The patient had a repeat massive lower gastrointestinal (GI) bleed episode and succumbed to death.
This is a rare case as a direct invasion of HCC into the GI tract is uncommon. Most of the extrahepatic metastasis of HCC occurs in patients with advanced-stage intrahepatic tumors. Lungs, abdominal lymph nodes, and bones are the most common sites of extrahepatic metastasis in HCC [1]. Direct invasion to the GI tract by HCC is uncommon, with a reported incidence of approximately 0.5–2% among clinical HCC cases [2, 3]. The most common clinical presentation is frank GI bleeding and the most common site of involvement is the stomach followed by the duodenum and colon [2, 3].
Colonic involvement by HCC has been reported in scanty case reports wherein HCC directly invaded into the transverse colon/hepatic flexure and presented with GI bleed. Rare reports with hematogenous spread of HCC to other parts of the colon are also available. Hirashita et al. [4] described 2 similar cases of HCC directly invading into the colon. Both patients underwent partial resection of the liver and colon but they had a very limited survival (1 month and 6 months, respectively). Lin et al. [2] reported 11 cases of GI metastasis in HCC and concluded that prognosis in all the patients was extremely poor. The authors also added that surgical intervention may be the optimal choice for palliative treatment of HCC with GI involvement. In a study from Taiwan, hematogenous spread of HCC to the rectum was seen in a patient who presented with tenesmus [5]. The authors described this as one of the rare cases of hematogenous spread to the colon. Kashani et al. [6] described another rare site of HCC metastasis (i.e., periampullary region). It was diagnosed when a patient (known case of HCC who underwent TACE) was evaluated for low hemoglobin. The authors postulated that the periampullary metastasis was the result of tumor fragments migrating through the biliary tract [6].
References
1 Katyal S, Oliver JH, Peterson MS, Ferris JV, Carr BS, Baron RL: Extrahepatic metastases of hepatocellular carcinoma. Radiology 2000;216:698–703. [ Links ]
2 Lin CP, Cheng JS, Lai KH, et al: Gastrointestinal metastasis in hepatocellular carcinoma: radiological and endoscopic studies of 11 cases. J Gastroenterol Hepatol 2000;15:536–541. [ Links ]
3 Chen LT, Chen CY, Jan CM, et al: Gastrointestinal tract involvement in hepatocellular carcinoma: clinical, radiological and endoscopic studies. Endoscopy 1990;22:118–123. [ Links ]
4 Hirashita T, Ohta M, Iwaki K, et al: Direct invasion to the colon by hepatocellular carcinoma: report of two cases. World J Gastroenterol 2008;14:4583–4585. [ Links ]
5 Ou TM, Tsai WC, Hsieh TY, Shih YL: Hepatocellular carcinoma with colonic metastasis. Singapore Med J 2014;55:e93–e95. [ Links ]
6 Kashani A, Nissen NN, Guindi M, Jamil LH: Metastatic periampullary tumor from hepatocellular carcinoma presenting as gastrointestinal bleeding. Case Rep Gastrointest Med 2015;2015:732140. [ Links ]
Statement of Ethics
This study did not require informed consent nor review/approval by the appropriate ethics committee.
Disclosure Statement
The authors have no conflicts of interest to declare.
* Corresponding author.
Dr. Nirmaljeet Singh Malhi
Department of Gastroenterology and Liver Disease
SPS Hospital Ludhiana 141003 (India)
E-Mail drnjsmalhi@gmail.com
Received: December 3, 2017; Accepted after revision: March 6, 2018














