Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.26 no.4 Lisboa ago. 2019
https://doi.org/10.1159/000493439
CLINICAL CASE STUDY
Perforated Meckels Diverticulum in an Adult
Perfuração de divertículo de Meckel num adulto
Rita Cameloa, Paula Santosa,b, Rui Mateus Marquesa,b
aServiço de Imagiologia, Hospital de São José, Centro Hospitalar Lisboa Central, Lisbon, Portugal; bDepartamento de Radiologia, NOVA Medical School, Faculdade de Ciências Médicas da Universidade Nova de Lisboa, Lisbon, Portugal
* Corresponding author.
ABSTRACT
Meckels diverticulum is the commonest congenital anomaly of the gastrointestinal tract. Its complications have an extensive variety of clinical and imaging manifestations, extending from benign and indolent findings to acute lifethreatening conditions. Complicated Meckels diverticulum often constitutes a challenging diagnosis for both the clinician and the radiologist. Therefore, imaging techniques play an important role in this condition in evaluating its complications, determining decision making. We describe a case of a 49-year-old man suffering from right abdominal pain with fever and constipation, during the past 5 days. Laboratory data revealed C-reactive protein of 306 mg/L and leukocytosis. Contrast-enhanced CT features were highly suggestive of perforated Meckels diverticulum. The purpose of this article is to emphasize that besides its rarity, Meckels diverticulum complications can occur in adult patients.
Keywords: Gastrointestinal symptoms, Surgery, Gastrointestinal tract, Diagnosis, Computed tomography
RESUMO
O divertículo de Meckel é a anomalia congénita mais comum do tracto gastrointestinal. As suas complicações variam num amplo espectro, desde achados benignos e indolentes até condições potencialmente graves, e constituem frequentemente um desafio diagnóstico tanto para o clinico como para o médico radiologista. Neste sentido, os métodos de diagnóstico por imagem desempenham um papel importante na avaliação e extensão das suas complicações, determinando muitas vezes a tomada de decisões. Descrevemos um caso de um paciente de 49 anos, que apresenta dor abdominal lateralizada à direita, febre e obstipação, durante um período de 5 dias. Analiticamente apresenta valores de proteína C reactiva de 306 mg/L e leucocitose. O estudo TC contrastado foi muito sugestivo de divertículo de Meckel perfurado. O objectivo deste artigo é enfatizar que, apesar da sua raridade, as complicações do divertículo de Meckel podem ocorrer em pacientes em idade adulta.
Palavras-Chave: Sintomatologia gastrointestinal, Cirurgia, Tracto gastrointestinal, Diagnóstico, Tomografia computorizada
Introduction
Meckels diverticulum (MD) is the commonest congenital anomaly of the gastrointestinal tract. It is a true diverticulum having all the layers of the intestinal wall [1, 2] and is usually localized in the pelvic or periumbilical region or right iliac fossa. The referred locations of MD are related to its complications. The preferred location is at the anti-mesenteric border of the ileum, 2 ft (60 cm) proximal to the ileocecal valve. The well-known rules of 2 state that the MD occurs in about 2% of the population, it is about 2 inches in length, is usually located within 2 ft of the ileocaecal valve, and usually presents before 2 years of age [3]. MD results from the incomplete obliteration of the omphalomesenteric or vitelline duct during the 5th week of gestation [3].
MD manifests more commonly in children. However, complications can occur in adults and it may give rise to bleeding (11.8%), intestinal obstruction (36.5%), inflammation (12.7%), intussusceptions (13.7%), and neoplasm (3.2%). Perforation is very rarely seen and, in a review, was reported as being responsible for 0.5% of symptomatic diverticulum [4–6]. In adult patients, intestinal obstruction is the most common complication, with incidence rates varying from 22 to 50% [7].
MD complications become clinically apparent in up to 16–20% patients with this condition [1, 8]. Symptomatic diverticula are more common in males than in females, despite the fact that there is no known gender predisposition of asymptomatic MD [3], and the incidence of complications decreases with age, with the majority occurring in the pediatric population [9].
Case Report
A 49-year-old Caucasian male attended the emergency department because of right abdominal pain, fever, and constipation during the past 5 days. He also reported increasing symptoms during the last day. The patient had no significant medical history.
Physical examination detected significant tenderness on palpation of his right iliac fossa, with signs of localized peritonitis, including involuntary guarding and rebound tenderness. Auricular temperature was 37.5ºC. Laboratory data revealed C-reactive protein serum level of 306 mg/L (normal range, < 5.0 mg/L) and leukocytosis (24,000/µL [normal range, 4,500–11,000/µL]).
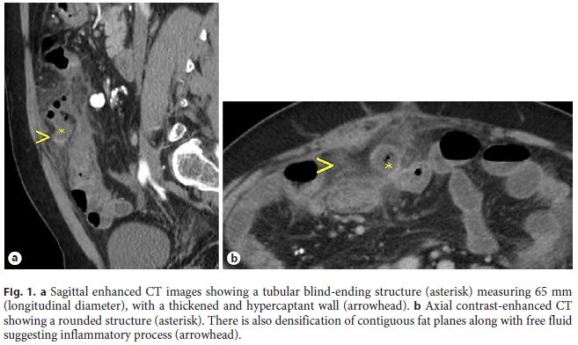
Abdominal X-ray and abdominal ultrasound showed no significant alterations, with no signs of acute appendicitis. In this case of acute abdomen, without an evident cause, an abdominal/pelvic computed tomography (CT) scan with intravenous contrast was performed, and a tubular blind-ending structure arising from the terminal ileum, measuring 65 × 25 mm (longitudinal and transverse diameter, respectively), was demonstrated. It was associated with a thickened and hypercaptant distal ileum, with intramural bowel gas as well as foci of adjacent extraluminal gas. A surrounding fat stranding was also detected (Fig. 1). No significant lymphadenopathy could be appreciated. The rest of the abdomen, including the appendix, was unremarkable. In conclusion, contrast-enhanced CT features were highly suggestive of a perforated MD.
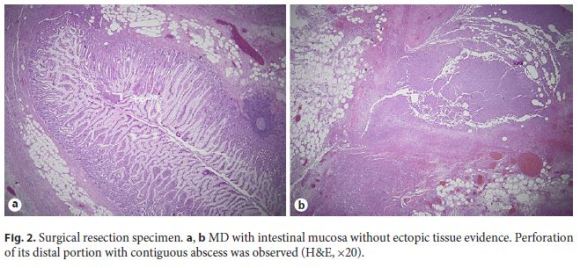
Based on imaging findings in association with worsening general condition, an emergency laparotomy intervention was performed and perforated Meckels diverticulitis was confirmed, along with an extensive inflammatory mass (abscess) with ileal, ascending colon, and abdominal wall involvement. Therefore, the patient was submitted to a right hemicolectomy and segmental enterectomy, with an ileocolostomy. Histological examination revealed an MD, measuring about 80 × 35 mm, with perforation of its distal portion with contiguous abscess. There was no evidence of ectopic tissues in the MD (Fig. 2). The patient recovered well after surgery and completed 8 days of antibiotic therapy.
Discussion
The majority of MD cases remain clinically silent during the entire lifetime, and their presence may be discovered incidentally during surgery, autopsy, or when performing small gastrointestinal studies [10, 11]. On CT, MD may appear as a fluid- or air-filled blind-ending pouch that arises from the antimesenteric side of the distal ileum. However, CT has a low sensitivity for the detection of uncomplicated MD because its appearance mimics that of a normal bowel loop. Complicated MD represents an important cause of acute abdominal pain [12, 13], and most cases with inflamed MD may be visualized on CT.
The diverticulum is considered complicated if it is the site of bowel obstruction or if it presents surrounding features of infiltration or inflammation, signs of perforation, adjacent fluid collection, or active bleeding. Depending on the type of complication, the diverticulum may have surrounding mesenteric inflammatory changes or may look like a localized fluid or air-fluid collection, with normal aspect of the small bowel proximal and distal to the diverticular inflammation [3]. However, less than 10% of symptomatic MD is diagnosed preoperatively [5].
The most common presentation associated with symptomatic or complicated MD is bleeding, followed by intestinal obstruction, diverticulitis, intussusceptions, and neoplasm [14]. Perforation is noted to be an occasional consequence of acute Meckels diverticulitis, but the exact rate of this has not been reported [15].
There are a few studies described in this particular complication in adults, and they are not consensual: According to a study by Kusumoto et al. [16], in a review of 776 Japanese patients, it has been reported that perforation accounted for 10.8% (84 of 776) of complications associated with the MD. According to Chae et al. [7], perforation is rarely seen and was reported as being responsible for 0.5% of symptomatic diverticulum. Another study (composed of 12 men and 11 women, with a mean age of 42.6 years, over a 15-year period) concluded that diverticulum-related complications demonstrated by surgery were inflammation in 14 patients, bleeding in 5 patients, intestinal obstruction in 3 patients, and penetrating foreign body causing perforation in 1 patient [3].
MD perforation is a serious and often life-threatening complication, usually secondary to diverticulitis, gangrene, or peptic ulceration due to ectopic gastric mucosa. Other various pathologies leading to perforation are Littres hernia and tumors such as leiomyosarcoma, lymphatic sarcoma, and poorly differentiated stromal tumor [17]. Perforation of MD by foreign bodies is extremely rare, and in a review, the indication rate for a resection due to perforation by foreign body was reported to be 8% of all complicated diverticula [18].
However, a symptomatic or complicated MD diagnosis is difficult to confirm on the basis of history, physical examination, laboratory findings, and imaging, because a variety of conditions can mimic the MD both clinically and radiologically (such as appendicitis, ileal/colonic diverticulitis, or regional enteritis/colitis) [19].
Traditionally, clinicians, when confronted with a patient with complicated MD, relied on conventional gastrointestinal contrast studies, angiography, or scintigraphy. However, these methods have been progressively replaced by CT scan, which is now routinely used as the first-line imaging tool in the diagnostic workup of the acute abdomen [20]. The sensitivity of diagnosing the MD on CT scan has increased owing to the availability of higher spatial resolution and multiplanar isotropic reconstruction ability of the latest MDCT scanners, which allow visualization of the small bowel in various planes [21].
Other techniques, including conventional radiographic examination, are of limited value and usually unrevealing. However, it may show enteroliths, findings of bowel obstruction, and the presence of gas or a gas-fluid level in the diverticulum [22]. Although of limited value, sonography has been used for the investigation of MD [23]. High-resolution sonography usually shows a fluid-filled structure in the right lower quadrant having the appearance of a blind-ending, thick-walled loop of bowel, with the typical gut signature and a clear connection to a peristaltic, normal small-bowel loop [21]. Scintigraphy with 99mTc-Na-pertechnetate has only minor diagnostic value and a limited sensitivity of 60% in diagnosing MD [24]. However, it aids in the diagnosis of diverticula with ectopic gastric mucosa. Pertechnetate is taken up by mucinsecreting cells of the gastric mucosa and ectopic gastric tissue. Higher sensitivity in pediatric (85–90%) than in adult (60%) patients is noticed [24]. This could be due to earlier symptoms (such as hemorrhage) in patients with ectopic gastric mucosa.
There is no consensus in the literature on the management of MD complications. In one study, the authors suggested four features associated with symptomatic diverticula – age < 50 years, male sex, diverticulum length > 2 cm, and the presence of ectopic or abnormal features within the diverticulum – and recommended that the presence of any of these four criteria should warrant removal of the MD [1]. Surgical removal of an MD is the current management of choice in a patient symptomatic for an MD or for any of its complications. However, the controversy surrounding surgical removal of an incidentally detected MD still continues today [1]. This article highlights the importance of CT in the evaluation of MD complications because in the case of diverticulitis and perforation, inflammatory changes and extraluminal air may be present and can be easily identified on CT scan.
In conclusion, if an inflammatory process is visualized on CT in the lower abdomen or pelvis, particularly at midline, or if there is evidence of distal small-bowel obstruction, one should carefully search for the presence of a complicated diverticulum. If a normal appendix is identified, the likelihood of this diagnosis increases [25]. MD complications can present with a wide range of clinical and imaging manifestations, from benign indolent findings to acute life-threatening conditions [21]. CT findings of complicated MD are very polymorphic and should be remembered in the evaluation of adult patients with acute abdomen [8].
References
1 Park JJ, Wolff BG, Tollefson MK, Walsh EE, Larson DR: Meckel diverticulum: the Mayo clinic experience with 1,476 patients (1950– 2002). Ann Surg 2005;241:529–533. [ Links ]
2 Matsagas MI, Fatouros M, Koulouras B, Gian- noukas AD: Incidence, complications, and management of Meckels diverticulum. Arch Surg 1995;130:143–146. [ Links ]
3 Platon A, Gervaz P, Becker CD, Morel P, Poletti PA: Computed tomography of complicated Meckels diverticulum in adults: a pictorial review. Insights Imaging 2010; 1:53–61. [ Links ]
4 Groebli Y, Bertin D, Morel P: Meckels diverticulum in adults: retrospective analysis of 119 cases and historical review. Eur J Surg 2001; 167: 518–524. [ Links ]
5 Ymaguchi M, Takeuchi S, Awazu S: Meckels diverticulum. Investigation of 600 patients in Japanese literature. Am J Surg 1978;136:247–249. [ Links ]
6 Leijonmarck CE, Bonman-Sandelin K, Frisell J, Raf L: Meckels diverticulum in the adult. Br J Surg 1986; 3:146–149. [ Links ]
7 Chae HD: Perforation of Meckels diverticulum by a chicken bone; preoperatively presenting as bowel perforation. J Korean Surg Soc 2011;80:234–237. [ Links ]
8 Mackey WC, Dineen P: A fifty year experience with Meckels diverticulum. Surg Gynecol Obstet 1983;156:56–64. [ Links ]
9 Kloss BT, Broton CE, Sullivan AM: Perforated Meckel diverticulum, Int J Emerg Med 2010;3:455–457. [ Links ]
10 Levy AD, Hobbs CM: From the archives of the AFIP. Meckel diverticulum: radiologic features with pathologic correlation. Radiographics 2004;24:565–587. [ Links ]
11 Rossi P, Gourtsoyiannis N, Bezzi M, Raptopoulos V, et al: Meckels diverticulum: imaging diagnosis. AJR Am J Roentgenol 1996;166:567–573. [ Links ]
12 Sancar S, Demirci H, Sayan A, Arıkan A, Candar A: Meckels diverticulum: ten years experience. Ulus Cerrahi Derg 2015;31:65–67. [ Links ]
13 Yahchouchy EK, Marano AF, Etienne JC, Fingerhut AL: Meckels diverticulum. J Am Coll Surg 2001;192:658–662. [ Links ]
14 Dimitriou I, Evaggelou N, Tavaki E, Chatzitheoklytos E: Perforation of Meckels diverticulum by a fish bone presenting as acute appendicitis: a case report. J Med Case Rep 2013;7:231. [ Links ]
15 Ferguson H, Soumian S, Dmitrewski J: Perforation of Meckels diverticulum secondary to a large faecolith. BMJ Case Rep 2010;2010. pii: bcr09.2009.2308. [ Links ]
16 Kusumoto H, Yoshida M, Takahashi I, Anai H, Maehara Y, Sugimachi K: Complications and diagnosis of Meckels diverticulum in 776 patients. Am J Surg 1992;164:382–383. [ Links ]
17 Hager M, Maier H, Eberwein M: Perforated Meckels diverticulum presenting as a gastrointestinal stromal tumor: a case report. J Gastrointest Surg 2005;9:809–811. [ Links ]
18 Yagcı G, Cetiner S, Tufan T: Perforation of Meckels diverticulum by a chicken bone, a rare complication: report of a case. Surg Today 2004;34:606–608. [ Links ]
19 Khandelwal A, Virmani V, Ryan J, Kielar A, Fraser-Hill M, Sheikh A: Solving the mystery of Meckel diverticulum. AJR Am J Roentgenol 2012;198:E166. [ Links ]
20 Leschka S, Alkadhi H, Wildermuth S, Marincek B: Multidetector computed tomography of acute abdomen. Eur Radiol 2005;15:2435–2447. [ Links ]
21 Kotha K, et al: Radiologists perspective for the Meckels diverticulum and its complications Br J Radiol 2014;87:20130743. [ Links ]
22 Elsayes KM, Menias CO, Harvin HJ, Francis IR: Imaging manifestations of Meckels diverticulum. AJR Am J Roentgenol 2007; 189:81– 88. [ Links ]
23 Mostbeck GH, Liskutin J, Dorffner R, et al: Ultrasonographic diagnosis of a bleeding Meckels diverticulum. Pediatr Radiol 2000;30:382. [ Links ]
24 Poulsen KA, Qvist N: Sodium pertechnetate scintigraphy in detection of Meckels diverticulum: is it usable? Eur J Pediatr Surg 2000;10:228–231. [ Links ]
25 Bennett GL, Birnbaum BA, Balthazar EJ: CT of Meckels diverticulitis in 11 patients. AJR Am J Roentgenol 2004;182:625–629. [ Links ]
Statement of Ethics
The authors have no ethical conflicts to disclose.
Disclosure Statement
The authors have no conflicts of interest to declare.
Funding Sources
No subsidies or grants contributed to this work.
* Corresponding author.
Rita Camelo
Serviço de Imagiologia, Hospital de São José, Centro Hospitalar Lisboa Central
R. José António Serrano PT–1150-199 Lisbon (Portugal)
E-Mail ritameiracamelo@gmail.com
Received: June 27, 2018; Accepted after revision: September 2, 2018
Acknowledgement
The authors would like to thank Dr. Joana Santos, Pathology Department, Centro Hospitalar Lisboa Central, Hospital de São José, for slides review and helpful discussion.














