Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.26 no.5 Lisboa out. 2019
https://doi.org/10.1159/000495524
ORIGINAL ARTICLE
Cross-Sectional Study to Assess Endoscopic Ultrasound Practice in Portugal
Estudo transversal de avaliação da prática de ecoendoscopia digestiva em Portugal
Juliana M. Costa, Dália Fernandes, Bruno Gonçalves, Raquel Gonçalves, João B. Soares
Gastroenterology Department, Braga Hospital, Braga, Portugal
* Corresponding author.
ABSTRACT
Background: Despite the increasing number of national departments performing endoscopic ultrasound (EUS), there are no official data regarding clinical EUS practice in Portugal. Objectives: We aimed to evaluate the current practice of EUS in Portugal. Methods: By email, we invited 1 physician of each one of the 26 national Gastroenterology Departments which perform EUS to complete a survey questionnaire available on the Google Forms platform. The online questionnaire was available from September 2017 until February 2018 and was answered only by physicians who perform EUS. Results: A total of 21/26 (80.8%) national Gastroenterology Departments answered the questionnaire. In Portugal, there are 42 echoendoscopes in total; most of the echoendoscopy units have only 1 EUS processor (81%), 1 radial echoendoscope (66.7%), 1 linear echoendoscope (76.2%), 1 anorectal probe (57.1%), but no miniprobes (85.7%). About 81% have histological core acquisition needles. In 81% of the units, there are at least 2 ultrasonographers who perform echoendoscopy together (at least 2 ultrasonographers per EUS) in 47.6% of these departments. The ultrasonographers also performed abdominal ultrasound (US), anal US, and endoscopic retrograde cholangiopancreatography in 71.4, 66.7, and 42.9%, respectively. The echoendoscopy units have 2.4 ± 1.1 periods of echoendoscopy per week and 4 ± 1.5 EUS per period (499.2 ± 416.8 EUS per year). Subepithelial lesions and biliopancreatic lesion evaluation as well as gastrointestinal neoplasia staging were the most common EUS indications. The number of FNA (fineneedle aspirations) ranges from 10 to 160/year. Rapid on-site evaluation (ROSE) is available in 60% of units and is performed by the cytopathologist (66.7%) in the majority of cases. The main reason for omitting ROSE is the limited pathology staff. Cytopathological material is prepared by the ultrasonographer in 25% of the units. Air drying (50%) and formalin (50%) are most frequently used to fix and preserve smears, respectively. Pancreatic pseudocyst drainage (66.7%), celiac plexus neurolysis (52.4%) and pancreatic necrosectomy (42.9%) are the most widespread therapeutic procedures. Conclusions: This survey provides the first insight into the current status of digestive echoendoscopy in Portugal. There is a great variability in diagnostic and therapeutic echoendoscopy practice.
Keywords: Endoscopic ultrasound, Echoendoscopy, Portugal, Survey questionnaire
RESUMO
Introdução: Apesar do crescente número de serviços nacionais a realizar ecoendoscopia digestiva, não existem dados sobre a prática da ecoendoscopia no nosso país. Objetivos: Pretendemos avaliar a prática da ecoendoscopia em Portugal. Métodos: Por e-mail convidámos um elemento de cada dos 26 serviços nacionais de Gastrenterologia que realizam ecoendoscopia a preencher um questionário disponível na plataforma google forms. O questionário esteve disponível via online de setembro de 2017 a fevereiro de 2018 e foi respondido apenas por médicos que realizam ecoendoscopia. Resultados: Obtivemos resposta de 21 dos 26 serviços convidados (80.8%). Em Portugal existe um total de 42 ecoendoscópios. A maioria das unidades possui 1 ecógrafo (81%), 1 ecoendoscópio radial (66.7%), 1 eco endoscópio linear (76.2%), 1 sonda rectal (57.1%) mas não dispõem de mini-sondas (85.7%). 81% dispõem de agulhas de aquisição de core histológico. Em 81% dos serviços existem pelo menos 2 ecoendoscopistas que realizam ecoendoscopia em conjunto em 47.6% dos serviços. Os ecoendoscopistas também realizam ecografia abdominal, ecografia anal e colangiopancreatografia retrógrada endoscópica em 71.4, 66.7 e 42.9% respectivamente. Os serviços têm em média 2.4 ± 1.1 períodos de ecoendoscopia/semana realizando em média 4 ± 1.5 ecoendoscopia/período (499.2 ± 416.8 ecoendoscopias/ano). A avaliação de lesões subepiteliais e bilio-pancreática, assim como o estadiamento de neoplasias do tubo digestivo são as indicações mais frequentes para a realização de ecoendoscopia. O número de punções diagnósticas guiadas por ecoendoscopia varia entre 10 e 160/ano. A maioria dos serviços (60%) dispõe de rapid on-site pathological evaluation (ROSE) que é realizada pelo citopatologista na maioria das vezes (66.7%). A carência de funcionários nas unidades de Anatomia Patológica é o principal motivo para a ausência de ROSE. A preparação do material citopatológico é realizada pelo ecoendoscopista em 25% dos serviços. A secagem ao ar (50%) e o formol (50%) são o método de fixação dos esfregaços e o meio de preservação mais usados, respetivamente. A drenagem de pseudocisto pancreático (66.7%), neurólise do plexo celíaco (52.4%) e necrosectomia pancreática (42.9%) são os procedimentos terapêuticos mais disseminados. Conclusões: Este trabalho fornece os primeiros dados sobre a prática de ecoendoscopia digestiva em Portugal. Existe uma grande variabilidade nos exames diagnósticos e terapêuticos.
Introduction
Endoscopic ultrasound (EUS) has been widely used for diagnosing, staging, and treatment of gastrointestinal, pancreatobiliary, anorectal, and mediastinal diseases [1]. Despite EUS being routinely used in many national Gastroenterology Departments, there are no official data regarding EUS practice in Portugal. In this study, we aimed to assess the current status of EUS in Portugal and seek to identify areas where the development of EUS expertise could be further enhanced.
Materials and Methods
Selection of Study Subjects
An online survey questionnaire was sent by email to 1 physician of each of the 26 national Gastroenterology Departments (26 in total of 38 governmental hospitals with Gastroenterology department) which perform EUS. The questionnaire was answered only by physicians who perform EUS. Consent to participate in the study was inferred from voluntary completion of the questionnaire.
Survey Questionnaire
An online questionnaire using the Google Forms platform with 42 questions (Appendix) was developed and took less than 15 min to complete. The survey questionnaire was divided into five sections: the first part (A) focused on description of the echoendoscopy unit; the second (B) examined the equipment and technology used; the third (C) included questions about echoendoscopy unit staff; the fourth (D) included questions regarding the practice of EUS including techniques, tissue processing, and analysis; the final part (E) of the survey examined training and local research studies in EUS.
Questionnaire Administration
Physicians were approached by email with a study invitation and were provided a direct link to the questionnaire. The online questionnaire was available from September 2017 until February 2018, and answering all questions was needed to complete the questionnaire. A reminder was sent by email once a week requesting the participation of the physicians who had not responded to the questionnaire. Subjects who did not respond until February 2018 were considered to be nonrespondents. The confidentiality of the survey and the anonymity of the respondents were ensured.
Statistical Analysis
Only completed survey questionnaires were used for data analysis. Data were tabulated as raw data and analyzed using a Microsoft Office Excel® spreadsheet; only a descriptive statistical analysis was performed. The variables in one question (question D4) were evaluated based on a score of frequency of responses, expressing a ranking of importance among the variables (sum of the score [1–5; 1 = least frequent and 5 = most frequent] given by the unit at each listed indication). Descriptive statistics, including frequencies, means, standard deviations, median, and range were generated for the variables of interest.
Results
A total of 26 national Gastroenterology Departments (governmental hospitals) were invited to respond to a survey questionnaire, of which 21 responded (80.8%). Table 1 summarizes general characteristic of echoendoscopy practice in Portugal.
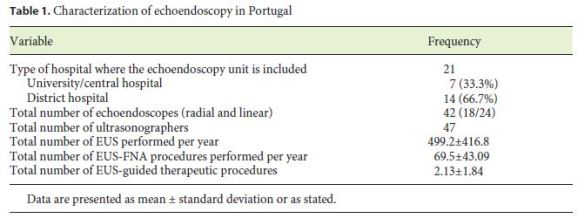
Echoendoscopy Unit Description
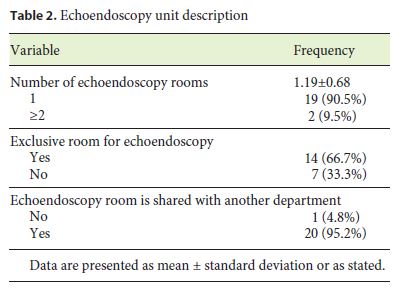
The echoendoscopy unit features are shown in Table 2. The majority of the requested departments have 1 exclusive echoendoscopy room. Only one department shares the echoendoscopy room with another department (General Surgery).
Echoendoscopy Equipment Description
The echoendoscopy equipment and technology used in national echoendoscopy units are shown in Table 3.
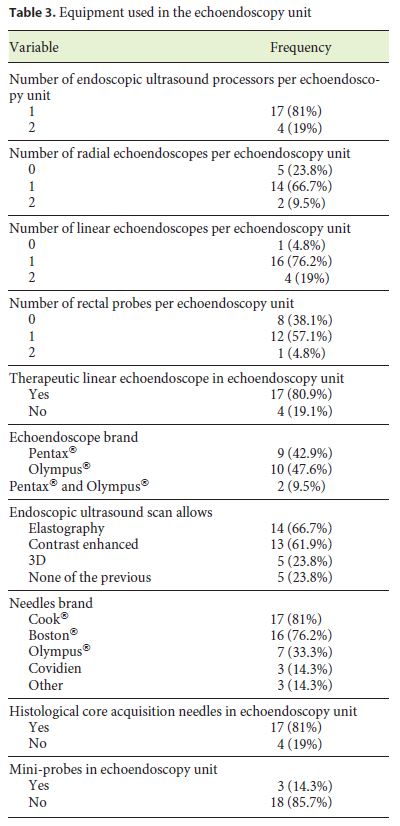
Almost all echoendoscopy units have only 1 EUS processor (81%), 1 radial echoendoscope (66.7%), 1 linear echoendoscope (76.2%), 1 anorectal probe (57.1%), but no miniprobes (85.7%). About 81% have histological core acquisition needles. Elastography and contrast-enhanced study are available in 66.7 and 61.9% of the echoendoscopy units, respectively.
Echoendoscopy Staff Description
The echoendoscopy staff description is presented in Table 4.
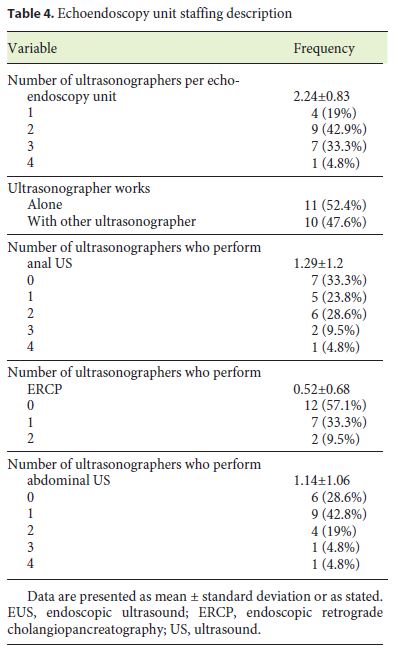
In 81% of the participating departments, there are at least 2 ultrasonographers who perform EUS together (at least 2 ultrasonographers per EUS) in 47.6% of these. The ultrasonographers also performed abdominal ultrasound (US), anal US and endoscopic retrograde cholangiopancreatography (ERCP) in 71.4, 66.7, and 42.9% of the inquired units.
EUS Practice
The EUS practice description is shown in Table 5. The echoendoscopy units have 2.4 ± 1.1 periods of echoendoscopy per week and 4 ± 1.5 EUS per period (499.2 EUS per year [range 169–1,001]). The most common EUS indications were subepithelial lesion evaluation (score 85), biliopancreatic lesions evaluation (score 74), and gastrointestinal neoplasia staging (score 54).
The majority of units perform EUS-FNA (95.2%) and the number of EUS-FNA ranges from 10 to 160 per year (69.5 ± 43.09 per year). Rapid on-site evaluation (ROSE) is available in 60% of units and is performed by the cytopathologist (66.7%) in the majority of units. The main reason for omitting ROSE is the limited pathology staff. Cytopathological material is prepared by a cytotechnician, a nurse or an ultrasonographer in 45, 30, and 25% of the units, respectively. Air drying (50%) and formalin (50%) are mostly used to fix and preserve smears, respectively. The cell block technique is applied in all echoendoscopy units which perform EUS-FNA.
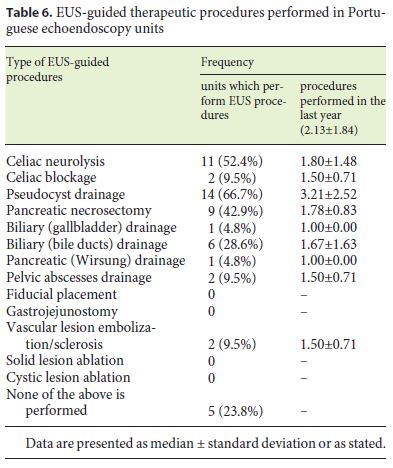
EUS-guided therapeutic procedures are described in Table 6. In Portuguese echoendoscopy units, 2.13 ± 1.84 (mean ± SD) therapeutic procedures were performed per year. Pancreatic pseudocyst drainage, celiac plexus neurolysis and pancreatic necrosectomy are the most widespread therapeutic procedures (66.7, 52.4, and 42.9%, respectively). Pancreatic pseudocyst drainage is the procedure most frequently performed (3.21 ± 2.52 per year). In 61.9% of the departments, at least 1 ultrasonographer is involved in multidisciplinary meetings. There are EUS databases in 57.1% of the units.
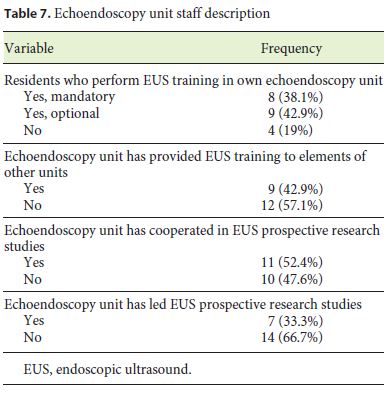
Training and Local Research Studies
For 80.9% of all respondents, the EUS training integrates the residents training program, and in 42.9% of the units EUS training was given to elements of another unit. The majority of units (52.4%) have cooperated in EUS prospective research studies, but only 36.8% have led research studies (Table 7).
Discussion
This is the first study to assess the current EUS practice in Portugal. Furthermore, this survey was completed by almost all invited echoendoscopy national units (response rate of 80.8%). It jointly assesses issues relating to echoendoscopy equipment use, staff, techniques, training, and local EUS research.
In terms of EUS equipment use, almost all national echoendoscopy units have equipment to perform diagnostic and therapeutic procedures which are usually performed by 2 ultrasonographers together. This compares to equipment use by ultrasonographers in the Asia-Pacific, where the majority of the ultrasonographers used radial echoendoscope (94.3%), linear echoendoscope (52.1%), and catheter US probe (66.2%) [2]; the same results were found in an international survey (radial [94.8%] and linear [79%] echoendoscopes and catheter US probes [60.2%] were generally used) [3].
In this survey, ultrasonographers tend to be more diagnostical than interventional endoscopists, since most of them perform diagnostic procedures such as abdominal and anal US (71.4 and 66.7%, respectively) and only 42.9% of them also perform ERCP. In other studies, most ultrasonographers performed ERCP [2–5]. In 1999, in the United States, 84% of the ultrasonographers performed ERCP [5]. In 2004, Das et al. [3] compared North American ultrasonographers with other international ultrasonographers; the study showed that they were more interventional and also performed ERCP and EUS-guided interventional procedures more often than other international ultrasonographers (86.4 vs. 67.9% and 86.4 vs. 63%, respectively) . One study published in 2006 concluded that in Asia the majority of the surveyed ultrasonographers performed ERCP (87.3%), while more than half of them carried out transabdominal US procedures (53.5%) [2]. Most recent research showed that in Latin America the percentage of ultrasonographers who also performed ERCP was 70% [4].
An interesting finding of this survey is that national echoendoscopy units perform a median of 500 EUS per year (range 169–1,001), and subepithelial lesion and biliopancreatic lesion evaluation as well as gastrointestinal neoplasia staging are the most common EUS indications.
In the majority of previous studies, the data about the number of EUS performed are shown as number of procedures performed during each ultrasonographers career, reflecting the ultrasonographers experience. In the 1999 United States survey, the median number of procedures ever performed was 200 (range 20–4,000) [5]. In the 2004 international survey, more than a third of ultrasonographers had been performing EUS for at least 5 years [3]. In the 2006 Asian survey, the respondents had a median experience of 5 years (range 0–17) in EUS practices and performed a median of 500 procedures (range 3–6,000) in their career [2]. However, in 2016, van Riet et al. [6] proposed to evaluate practice patterns within the international endosonographic community and revealed that most of the international respondents performed > 300 EUS (58%) and > 100 EUS-FNA procedures per year (68%).
Regarding indications for EUS, our results are consistent with other researches. A United States survey revealed that esophagogastric and pancreaticobiliary evaluations were the most common [5]; in a Latin America survey, pancreaticobiliary evaluation was the most common EUS indication [4] supporting our data. However, this may still reflect the level of knowledge of national ultrasonographers about EUS indications. The research conducted in 2006 by Yusuf et al. [7] aimed to assess the level of knowledge of American Society of Gastroenterology (ASGE) members about the indications of EUS and showed that the levels of knowledge of colorectal applications of EUS are the poorest for the four studied organ systems (esophagus, gastroduodenum, hepatopancreatobiliary, and colorectum).
Another interesting finding of this survey is that the vast majority of procedures are diagnostic. EUS-FNA is the most common interventional procedure being performed in 95.2% of the national units (69.5 ± 43.09 per year). Therapeutic procedures are performed by 76.2% (16/21 of the total requested units). However, these procedures are rarely performed (2.13 ± 1.84 per year), with pancreatic pseudocyst drainage, celiac plexus neurolysis, and pancreatic necrosectomy being the most frequent (performed in 66.7, 52.4, and 42.9% of the departments, respectively). These data are supported by Drigo et al. [4] who revealed that FNA (median 319, range 0–2,500), neurolysis (median 12, range 0–189), and pseudocyst drainage (median 10, range 0–178) were the procedures most frequently performed by Latin American ultrasonographers in their entire career.
It is important to notice that in our survey, ROSE is available only in 60% of units and is performed by the cytopathologist in most cases (66.7%). Limited pathology staff is the main reason for omitting ROSE. van Riet PA et al. showed only half of the European and Asian respondents used ROSE. In this study, respondents who refrain from using ROSE consider limited pathology staff (74%) and disbelieve in its additive value (32%) as the main reasons for omitting it [6]. These data were corroborated by DiMaio et al. [8] in a survey study which demonstrated that the vast majority of American ultrasonographers (76.2%) utilize ROSE when performing EUS-FNA.
In our study, air drying (50%) and formalin (50%) are most frequently used to fix and preserve smears, respectively. van Riet et al. [6] showed that after EUS-FNA, a majority of the ultrasonographers air dried (43%) and used formalin to preserve FNA specimens (62%).
In our survey, the cell block technique is applied in all echoendoscopy units which performed EUS-FNA. These data are in line with the results of van Riet et al. [6] which demonstrated that the majority of respondents applied the cell block technique (85%), but it was used to a lesser extent in Europe (85%) and Asia (70%) than in the United States (96%).
Also noteworthy is the general involvement of at least 1 ultrasonographer in multidisciplinary meetings (61.9%) and the existence of a local EUS database (57.1%).
The last, but certainly not the least remarkable finding concerns the EUS training and research. The majority (80.9%) of national echoendoscopy units train their own residents, and 42.9% have provided EUS training to elements of another hospital. The majority of units cooperated in EUS prospective research studies (52.4%). These data reflect the current EUS training program which has been practiced in Europe and consists of a combination of two methods of learning EUS: fellowship program and informal training (short repeated exposures to handson experience) [9].
The main strength of our survey is the high rate of response which ensures that our data reflect EUS national practice. Our survey has however some potential limitations. First, a reporting or goodwill bias is likely to exist, since this is inevitable in retrospective surveys that are based on self-reporting. Second, we evaluated the unit as a whole and not the individual practice, which may differ within each unit.
Conclusions
This study provides an overview and the first insight into the current status of EUS in Portugal revealing that there is a great deal of variability in diagnostic and therapeutic echoendoscopy.
Although our results suggest that Portuguese EUS practitioners are not behind their overseas counterpart in terms of technology adoption and practical experience, the same does not apply to therapeutic procedure experience.
Our survey questionnaire could serve as a model for the assessment and monitoring of national EUS practice with the involvement of all Portuguese ultrasonographers. Our data may be a benchmark for future studies.
References
1 Dumonceau JM, Polkowski M, Larghi A, Vilmann P, Giovannini M, Frossard JL, et al.; European Society of Gastrointestinal Endoscopy. Indications, results, and clinical impact of endoscopic ultrasound (EUS)-guided sampling in gastroenterology: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2011 Oct;43(10):897–912. [ Links ]
2 Ho KY. Survey of endoscopic ultrasonographic practice and training in the Asia-Pacific region. J Gastroenterol Hepatol. 2006 Aug;21(8):1231–5. [ Links ]
3 Das A, Mourad W, Lightdale CJ, Sivak MV Jr, Chak A. An international survey of the clinical practice of EUS. Gastrointest Endosc. 2004 Nov;60(5):765–70. [ Links ]
4 Drigo JM, Castillo C, Wever W, Obaldía JR, Fillipi S, Ribeiro MC, et al. Endoscopic ultrasound practice survey in Latin America. Endosc Ultrasound. 2013 Oct;2(4):208–18. [ Links ]
5 Savides TJ, Fisher AH Jr, Gress FG, Hawes RH, Lightdale CJ; ASGE Ad Hoc Endoscopic Ultrasound Committee. 1999 ASGE endoscopic ultrasound survey. Gastrointest Endosc. 2000 Dec;52(6):745–50. [ Links ]
6 van Riet PA, Cahen DL, Poley JW, Bruno MJ. Mapping international practice patterns in EUS-guided tissue sampling: outcome of a global survey. Endosc Int Open. 2016 Mar;4(3):E360–70. [ Links ]
7 Yusuf TE, Harewood GC, Clain JE, Levy MJ. International survey of knowledge of indications for EUS. Gastrointest Endosc. 2006 Jan;63(1):107–11. [ Links ]
8 DiMaio CJ, Buscaglia JM, Gross SA, Aslanian HR, Goodman AJ, Ho S, et al. Practice patterns in FNA technique: A survey analysis. World J Gastrointest Endosc. 2014 Oct;6(10):499–505. [ Links ]
9 Polkowski M, Larghi A, Weynand B, Boustière C, Giovannini M, Pujol B, et al.; European Society of Gastrointestinal Endoscopy (ESGE). Learning, techniques, and complications of endoscopic ultrasound (EUS)-guided sampling in gastroenterology: European Society of Gastrointestinal Endoscopy (ESGE) Technical Guideline. Endoscopy. 2012 Feb;44(2):190–206. [ Links ]
Statement of Ethics
Protection of Human and Animal Subjects
The authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentially of Data
The authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to Privacy and Informed Consent
Consent to participate in the study was inferred from voluntary completion of the survey questionnaire.
Disclosure Statement
The authors have no conflicts of interest to declare.
Funding Sources
No funding.
* Corresponding author.
Juliana M. Costa, MD
Gastroenterology Department, Hospital de Braga
Sete Fontes – São Victor
PT–4710-243 Braga (Portugal)
E-Mail julianamcosta87@gmail.com
Received: August 21, 2018; Accepted: November 13, 2018
Acknowledgements
The authors thank all the ultrasonographers who participated in the survey.
Author Contributions
Juliana M. Costa wrote the manuscript. Dália Fernandes, Bruno Gonçalves, Raquel Gonçalves, and João B. Soares revised the manuscript. All authors read and approved the final manuscript.














