Serviços Personalizados
Journal
Artigo
Indicadores
Links relacionados
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.27 no.2 Lisboa abr. 2020
https://doi.org/10.1159/000501403
IMAGES IN GASTROENTEROLOGY AND HEPATOLOGY
Rare Differential Diagnosis for a Common Crohns Disease Presentation
Diagnóstico diferencial incomum com apresentação Crohn-like
Joyce Chiviaa, Teresa Costab, Pedro Figueiredoa
aDepartment of Gastroenterology, Centro Hospitalar de Lisboa Ocidental, Hospital de Egas Moniz, Lisbon, Portugal; bDepartment of Pathology, Centro Hospitalar de Lisboa Ocidental, Hospital de Egas Moniz, Lisbon, Portugal
* Corresponding author.
Keywords: Ileocecal endometriosis, Crohns disease, Intestinal obstruction
Palavras-Chave: Endometriose ileocecal, Doença de Crohn, Obstrução intestinal
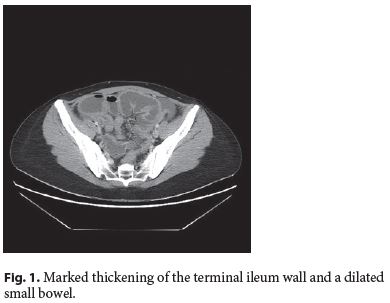
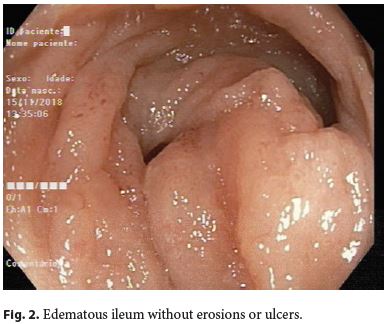
A 36-year-old female with no past medical history was admitted with a 1-week history of abdominal pain, vomiting, and no passing of stool or gas for 5 days. One week before, she had presented to the emergency department with a 2-week history of diarrhea, vomiting, generalized abdominal pain, and a 4-kg weight loss, without fever, which had been diagnosed as gastroenteritis and had been treated with broad-spectrum antibiotics and antiemetics. Physical examination showed a distended and tympanized abdomen, without peritoneal signs. Laboratory workup was only relevant for an elevated C-reactive protein 7.5 mg/dL. Abdominal X-ray revealed multiple airfluid levels; therefore, computed tomography was performed, showing marked thickening of the terminal ileum wall and a dilated small bowel, locoregional and mesenteric lymphadenopathies, as well as free liquid in the mesentery, paracolic gutter, and pelvic cavity (Fig. 1). Taken together, these findings were suggestive of ileal Crohns disease with small-bowel obstruction, so she was started on methylprednisolone. As there was no improvement, the patient underwent ileocolonoscopy that revealed a deformed cecum and a short segment of edematous ileum without erosions or ulcers (Fig. 2). Biopsies were inconclusive, so an ileocecal resection was scheduled.
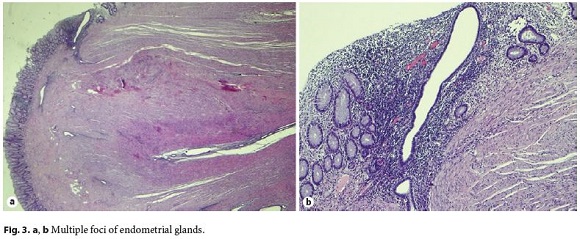
The surgical specimen revealed thickening of the terminal ileum and cecal wall, caused by multiple foci of endometrial glands with low proliferative activity along the muscularis propria, corresponding to ileocecal endometriosis (Fig. 3a, b).
In a previously asymptomatic immunocompetent young female, alternative diagnoses such as infectious ileitis were considered less likely due to the persistence of symptoms despite broad-spectrum antibiotics and the lack of risk factors for tuberculosis. Additionally, there were no clinical and laboratory clues suggesting malignant, vascular, or infiltrative diseases. Thus, given the typical clinical scenario, a presumptive diagnosis of Crohns disease was made. Colonoscopy was not initially performed due to the increased risk as well as the inability to undergo bowel preparation in the setting of bowel occlusion. Steroids were started as an urgent therapy with the intent to avoid surgery. Afterwards, the lack of improvement under steroids raised diagnostic doubts; therefore, a colonoscopy was done using carbon dioxide insufflation following several cleansing enemas.
Endometriosis was not considered in the initial differential diagnosis because there were no gynecological symptoms. However, estimates of endometriosis prevalence range from 2 to 10% of the women of reproductive age, and an unknown proportion are asymptomatic [1]. Ileocecal involvement is rare and may perfectly mimic or overlap with Crohns disease [2, 3]. Moreover, patients with endometriosis are at an increased risk of developing Crohns disease, which may cause future misdiagnosis of abdominal and gynecological symptoms in this patient [4]. In conclusion, although preoperative diagnosis is difficult, endometriosis should always be considered in the differential diagnosis of Crohns disease in women of reproductive age.
References
1 Dunselman GA, Vermeulen N, Becker C, Calhaz-Jorge C, DHooghe T, De Bie B, et al.; European Society of Human Reproduction and Embryology. ESHRE guideline: management of women with endometriosis. Hum Reprod. 2014 Mar;29(3):400–12.
2 Machairiotis N, Stylianaki A, Dryllis G, Zarogoulidis P, Kouroutou P, Tsiamis N, et al. Extrapelvic endometriosis: a rare entity or an under diagnosed condition? Diagn Pathol. 2013 Dec;8(1):194. [ Links ]
3 Craninx M, DHaens G, Cokelaere K, Baert F, Penninckx F, DHoore A, et al. Crohns disease and intestinal endometriosis: an intriguing co-existence. Eur J Gastroenterol Hepatol. 2000 Feb;12(2):217–21.
4 Jess T, Frisch M, Jørgensen KT, Pedersen BV, Nielsen NM. Increased risk of inflammatory bowel disease in women with endometriosis: a nationwide Danish cohort study. Gut. 2012 Sep;61(9):1279–83.
Statement of Ethics
This study did not require informed consent nor review/approval by the appropriate ethics committee.
Disclosure Statement
The authors declare no conflicts of interest.
Funding Sources
The authors have no funding sources to declare.
* Corresponding author.
Pedro Figueiredo
Department of Gastroenterology, Centro Hospitalar de Lisboa Ocidental
Hospital de Egas Moniz, Rua da Junqueira No. 126
PT–1349-019 Lisbon (Portugal)
E-Mail pedro.c.figueiredo@hotmail.com
Received: March 12, 2019; Accepted after revision: April 29, 2019
Acknowledgements
We thank Dr. Rui Mendo for performing critical revision. We thank Dr. Miguel Fróis Borges who performed the surgery and critical revision of the article.
Author Contributions
Joyce Chivia: acquisition of data; analysis and interpretation of data; drafting of the manuscript.
Teresa Costa: histological analysis and interpretation.
Pedro Figueiredo: critical revision of the manuscript for importante intellectual content.














