Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.27 no.2 Lisboa abr. 2020
https://doi.org/10.1159/000501804
IMAGES IN GASTROENTEROLOGY AND HEPATOLOGY
A Long History of Constipation
Uma longa história de obstipação
Andreia Ribeiroa, Gonçalo Freireb, Marlene Alvesc
aUSF Descobertas, ARS Lisboa e Vale do Tejo, Lisbon, Portugal; bRadiology Department, Hospital Beatriz Ângelo, Loures, Portugal; cUSF Santa Maria da Benedita, ARS Lisboa e Vale do Tejo, Alcobaça, Portugal
* Corresponding author.
Keywords: Fecal impaction, Intestinal obstruction, Abdominal pain, Constipation
Palavras-Chave: Impactação fecal, Obstrução intestinal, Dor abdominal, Obstipação
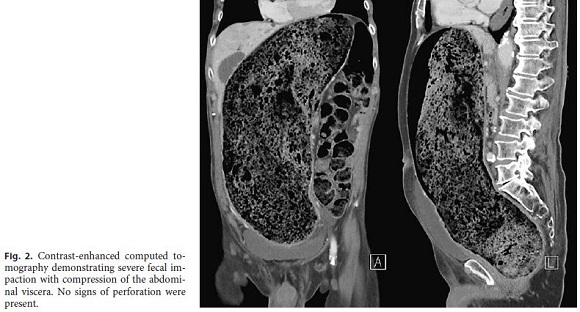
An otherwise healthy 64-year-old male presented to the emergency department with a 2-month history of constipation and tenesmus. He had seven admissions in the emergency department within the last 6 weeks and was already under laxative therapy, but it was ineffective. His physical examination was unremarkable, except for dehydration and diffuse abdominal pain. Blood tests demonstrated a mildly elevated serum creatinine. Abdominal radiography was performed and documented severe fecal impaction (Fig. 1). Computed tomography confirmed the presence of a fecal impaction with marked compression of the abdominal viscera, including the bile ducts, without signs of colonic perforation (Fig. 2). After rehydration, the patient underwent manual disimpaction under general anesthesia. His recovery was unremarkable.

Fecal impaction is a frequent and potentially serious medical condition. It is defined as a mass of compacted feces at any intestinal level that cannot be evacuated spontaneously [1].
Fecal impaction is a preventable disorder, and early diagnosis and treatment reduce the risk of complications, which include bowel obstruction leading to stercoral ulcer, perforation, peritonitis, or cardiopulmonary collapse with hemodynamic instability [2].
Constipation is frequent in adults > 60 years, in whom the prevalence is about 30%, increasing to at least 50% in nursing home residents [3]. In addition to age, risk factors for chronic constipation include female gender, physical inactivity, low education and income, concurrent medication use, and depression [4]. Decreased mobility and the inability to sense and respond to the presence of stool in the rectum will ultimately lead to impaction. This explains why the patients with the highest risk are the elderly and patients with neuropsychiatric disorders [5].
A digital rectal examination confirms the diagnosis of fecal impaction most of the times. However, impaction can occur in the proximal rectum or sigmoid colon, and a digital rectal examination will be nondiagnostic. In these cases, the next step should be an abdominal radiography as it can confirm the diagnosis and exclude major complications. Management involves mechanical removal of the stools, followed by implementation of a bowel maintenance regimen to prevent recurrence.
References
1 Zhao W, Ke M. Report of an unusual case with severe fecal impaction responding to medication therapy. J Neurogastroenterol Motil. 2010 Apr;16(2):199–202.
2 Hussain ZH, Whitehead DA, Lacy BE. Fecal impaction. Curr Gastroenterol Rep. 2014 Sep;16(9):404. [ Links ]
3 Mounsey A, Raleigh M, Wilson A. Management of Constipation in Older Adults. Am Fam Physician. 2015 Sep;92(6):500–4.
4 Higgins PD, Johanson JF. Epidemiology of constipation in North America: a systematic review. Am J Gastroenterol. 2004 Apr;99(4):750–9.
5 Obokhare I. Fecal impaction: a cause for concern? Clin Colon Rectal Surg. 2012 Mar;25(1):53–8.
Statement of Ethics
This study did not require informed consent or review/approval by the appropriate ethics committee.
Disclosure Statement
The authors have no conflicts of interest to declare.
Funding Sources
No funding was received.
* Corresponding author.
Andreia Ribeiro
USF Descobertas, ARS Lisboa e Vale do Tejo
Rua Fernão Mendes Pinto, No.19
PT–1400-145 Lisbon (Portugal)
E-Mail andreia.ribeiro@arslvt.min-saude.pt
Received: April 14, 2019; Accepted after revision: June 28, 2019
Author Contributions
Andreia Ribeiro designed this work and was responsible for clinical data acquisition and wrote the clinical vignette. In addition, she revised the whole manuscript.
Gonçalo Freire was responsible for the acquisition and processing of the images. He wrote the legends and revised the whole work.
Marlene Alves was responsible for the review of literature. She also revised the manuscript.














