Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.27 no.3 Lisboa jun. 2020
https://doi.org/10.1159/000503011
ENDOSCOPIC SNAPSHOT
Endoscopic Vacuum Therapy for Esophageal Perforation Treatment after Foreign Body Ingestion: Resolution after a Single Session
Terapêutica endoscópica de vácuo para perfuração esofágica após ingestão de corpo estranho: resolução após uma única sessão
Rui Morais, Filipe Vilas-Boas, Marco Silva, Pedro Pereira, Guilherme Macedo
Gastroenterology Department, Hospital de São João, Porto, Portugal
* Corresponding author.
Keywords: Esophageal perforation, Foreign body, Endoscopic vacuum therapy
Palavras-Chave: Perfuração esofágica, Corpo estranho, Terapêutica endoscópica de vácuo
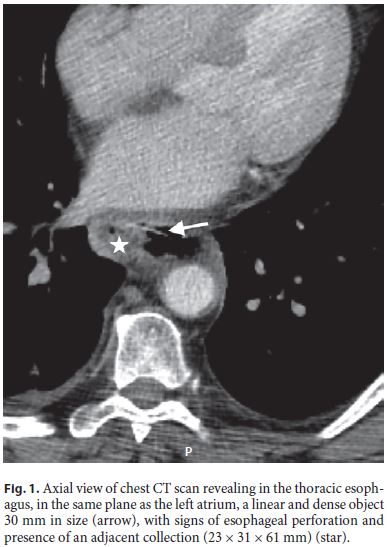
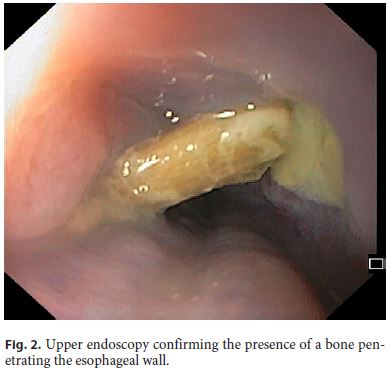
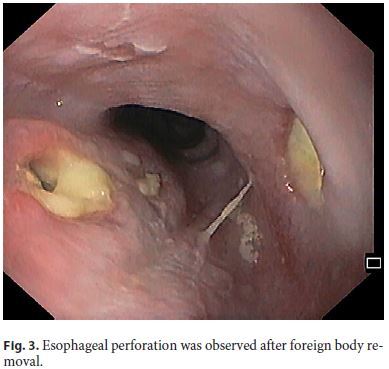
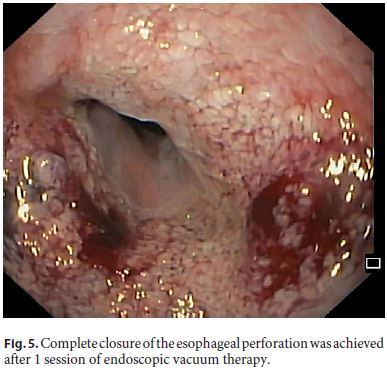
A 70-year-old man was admitted to the Emergency Department due to chest pain after foreign body ingestion (chicken bone) 5 days before. He mentioned having fever but denied other symptoms. Chest computed tomography (CT) scan revealed in the thoracic esophagus, in the same plane as the left atrium, a linear and dense object 30 mm in size, with signs of esophageal perforation and presence of an adjacent collection (23 × 31 × 61 mm) (Fig. 1). Following multidisciplinary discussion, it was decided to remove the foreign body and close the esophageal defect endoscopically. Upper endoscopy was performed (online suppl. Video; see http://www.karger.com/doi/10.1159/000503011) and confirmed the presence of a bone penetrating the esophageal wall, 32 cm from the incisors (Fig. 2). The surrounding mucosa was congestive, and purulent drainage was noticed. The foreign body was removed using an alligator jaw grasping forceps, and a 5-mm esophageal wall defect was observed (Fig. 3). We decided to perform endoscopic vacuum therapy (EVT) to try to close the defect and simultaneously treat the collection. The sponge (Endo-Sponge system, B. Braun, Melsungen, Germany) was placed in the esophageal lumen after appropriate positioning of the overtube (Fig. 4). After the procedure, the patient was admitted on total parenteral nutrition, antibiotics, and an antifungal. Five days later, upper endoscopy was repeated with sponge removal. Granulation tissue was observed at the location of the wall defect, with apparent resolution of the perforation (Fig. 5). CT was repeated showing no oral contrast leakage and significant improvement of the collection dimensions (27 × 17 mm). The patient resumed oral feeding 2 days after sponge removal, completed a 10-day antibiotic course, and was discharged. He remains well 9 months after the procedure, with no esophageal symptoms.
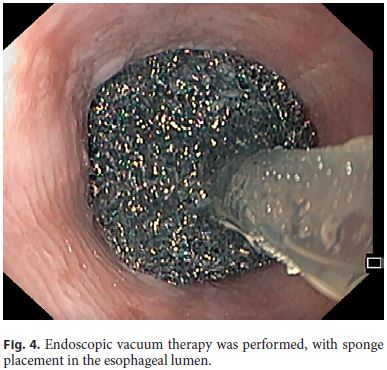
Esophageal perforations are rare, with an incidence of 3.1 per 1,000,000 per year [1] but are associated with high morbidity and mortality [2, 3]. Although surgery has traditionally been the gold standard care for patients with esophageal perforation, endoscopy is now emerging as the primary treatment modality of this condition [4]. Endoscopic closure of esophageal transmural defects can be achieved using a variety of modalities, including through-the-scope clips, over-the-scope clips, stents, or endoscopic suturing; however, additional percutaneous/surgical drainage of collections is often required [5]. EVT is an alternative approach for the endoscopic treatment of esophageal perforations, allowing simultaneous closure of the defect and drainage of a collection [6, 7]. Previous studies have evaluated the role of EVT in the treatment of esophageal perforations, with a reported successful closure of the defect between 70 and 100%, with an average of 5 sponge exchanges (range 0–39) [8–11]. In this case, only 1 EVT session was necessary, with no need for sponge replacement, highlighting the efficacy of this technique for treating esophageal wall defects with associated collections.
References
1 Vidarsdottir H, Blondal S, Alfredsson H, Geirsson A, Gudbjartsson T. Oesophageal perforations in Iceland: a whole population study on incidence, aetiology and surgical outcome. Thorac Cardiovasc Surg. 2010 Dec;58(8):476–80.
2 Altorjay A, Kiss J, Vörös A, Bohák A. Nonoperative management of esophageal perforations. Is it justified? Ann Surg. 1997 Apr;225(4):415–21.
3 Bufkin BL, Miller JI Jr, Mansour KA. Esophageal perforation: emphasis on management. Ann Thorac Surg. 1996 May;61(5):1447–51.
4 Saxena P, Khashab MA. Endoscopic Management of Esophageal Perforations: Who, When, and How? Curr Treat Options Gastroenterol. 2017 Mar;15(1):35–45.
5 Rodrigues-Pinto E, Morais R, Macedo G, Khashab MA. Choosing the Appropriate Endoscopic Armamentarium for Treatment of Anastomotic Leaks. Am J Gastroenterol. 2019 Mar;114(3):367–71.
6 Laukoetter MG, Mennigen R, Neumann PA, Dhayat S, Horst G, Palmes D, et al. Successful closure of defects in the upper gastrointestinal tract by endoscopic vacuum therapy (EVT): a prospective cohort study. Surg Endosc. 2017 Jun;31(6):2687–96.
7 de Moura DT, de Moura BF, Manfredi MA, Hathorn KE, Bazarbashi AN, Ribeiro IB, et al. Role of endoscopic vacuum therapy in the management of gastrointestinal transmural defects. World J Gastrointest Endosc. 2019 May;11(5):329–44.
8 Möschler O, Nies C, Mueller MK. Endoscopic vacuum therapy for esophageal perforations and leakages. Endosc Int Open. 2015 Dec;3(6):E554–8.
9 Kuehn F, Schiffmann L, Janisch F, Schwandner F, Alsfasser G, Gock M, et al. Surgical Endoscopic Vacuum Therapy for Defects of the Upper Gastrointestinal Tract. J Gastrointest Surg. 2016 Feb;20(2):237–43.
10 Loske G, Schorsch T, Dahm C, Martens E, Müller C. Iatrogenic perforation of esophagus successfully treated with Endoscopic Vacuum Therapy (EVT). Endosc Int Open. 2015 Dec;3(6):E547–51.
11 Heits N, Stapel L, Reichert B, Schafmayer C, Schniewind B, Becker T, et al. Endoscopic endoluminal vacuum therapy in esophageal perforation. Ann Thorac Surg. 2014 Mar;97(3):1029–35.
Statement of Ethics
The authors have no ethical conflicts to disclose.
Disclosure Statement
The authors have no conflicts of interest to declare.
* Corresponding author.
Rui Morais
Gastroenterology Department, Hospital de São João
Alameda Professor Hernâni Monteiro
PT–4200-319 Porto (Portugal)
E-Mail ruimorais20@gmail.com
Received: July 1, 2019; Accepted after revision: August 29, 2019














