Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.27 no.6 Lisboa dez. 2020
https://doi.org/10.1159/000507336
REVIEW ARTICLE
Palliative Care in End-Stage Liver Disease Patients Awaiting Liver Transplantation: Review
Cuidados Paliativos nos doentes com Doença Hepática avançada que aguardam transplante hepático: revisão
Sara Vieira Silvaa,b, Elga Freirea,b, Helena Pessegueiro Mirandab–d
aEquipa Intra-Hospitalar de Suporte de Cuidados Paliativos, Serviço de Medicina, Centro Hospitalar e Universitário do Porto, Porto, Portugal; bInstituto de Ciências Biomédicas Abel Salazar (ICBAS), Universidade do Porto, Porto, Portugal; cUnidade de Transplantação Hepato-bilio-pancreática, Centro Hospitalar e Universitário do Porto, Porto, Portugal; dInstituto de Saúde Publica da Universidade do Porto (ISPUP), Universidade do Porto, Porto, Portugal
* Corresponding author.
ABSTRACT
Introduction: End-stage liver disease (ESLD) is the advanced phase of most liver diseases. The cure is liver transplantation (LT), only available for a minority of patients. This review summarizes the evidence regarding palliative care (PC) in ESLD patients awaiting LT. Methods: Review of the literature available in Medline, Scopus and Web of Knowledge, with keywords ESLD and PC. Results: Fifteen of the 230 articles reviewed met the inclusion criteria. Ten main themes were addressed: symptom burden; perspectives of life-sustaining treatment and comfort for patients, families and health professionals; goals of care discussions; patient and family needs; quality of life; PC and survival; referral to PC, barriers and opportunities; integration of PC; outpatient care and cost-effectiveness analysis. The referral of patients to PC was only evaluated in a few studies, all of which reported low referral rates. Better knowledge of how PC professionals can support other professionals was considered important, and also better ways to integrate PC were considered essential. Conclusion: ESLD patients awaiting LT have a significant need for PC and, despite the insufficient response, were reported to benefit from this type of care. Future research is essential to determine the means to overcome barriers and better integrate PC for ESLD patients awaiting LT.
Keywords: Palliative care, End-stage liver, Liver transplantation
RESUMO
Introdução: A doença hepática avançada (DHA) corresponde à fase mais avançada das doenças hepáticas. O transplante hepático (TH) é o tratamento curativo, disponível apenas para uma minoria de doentes. Esta revisão sumariza a evidência sobre cuidados paliativos (CP) em doentes com DHA que aguardam TH. Métodos: Revisão da literatura existente na Medline, Scopus e Web of Knowledge. Palavras chave pesquisadas CP e DHA. Resultados: Quinze dos 230 artigos encontrados cumpriram critérios de inclusão. Dez temáticas foram abordadas: carga sintomática; discussão de objectivos de cuidados; perspectivas sobre tratamentos de suporte artificial e conforto; necessidades do doente e família; qualidade de vida; CP e impacto no prognóstico; referenciação para CP, barreiras e oportunidades; integração dos CP; cuidados de ambulatório e análises de custo-benefício. Poucos estudos avaliaram a referenciação para CP, todos com baixas taxas. Mais conhecimento e formação dos profissionais que acompanham doentes com DHA parece ser necessário, bem como, melhor articulação entre os diferentes intervenientes. Conclusão: Doentes com DHA que aguardam TH apresentam importantes necessidades de CP. Apesar da insuficiente resposta a este nível, parecem beneficiar deste tipo de cuidados. Estudos futuros que clarifiquem como ultrapassar as barreiras e a melhor integração dos CP nos doentes que aguardam TH são essenciais.
Palavras-Chave: Cuidados paliativos, Doença hepática avançada, Transplante hepático
Introduction
End-stage liver disease (ESLD) is the advanced phase of most liver diseases and is characterized by the complications of liver disease [1]. It is responsible for almost 2% of all deaths and is currently the 7th leading cause of death at the European level [2]. ESLD is the leading cause of organ failure amongst the population under 65 years [3], thus corresponding to a very significant loss of years of potential life. Episodes of decompensation have a significant impact on mortality, and it is estimated that, after the first episode, mortality at 5 years may reach 85% [4]. The only effective treatment is liver transplantation (LT), available for a minority of patients.
Previous studies have shown that ESLD patients usually present with high symptom prevalence [5], similar to patients with other advanced diseases such as cancer, heart or respiratory failure. Symptom burden associated with LT complexity and the high risk of mortality suggest significant palliative care (PC) needs for ESLD patients. Despite these important needs, PC referral remains low and the available data are scarce [6]. In one of the rare known studies [7], only 10% of the patients excluded from the transplant list were referred for PC. Little is known about the remainder of ESLD patients and specifically about PC for patients awaiting LT.
This review summarizes the available evidence-based literature regarding PC in ESLD patients awaiting LT.
Methods
We conducted a review in order to scan the current literature and identify the nature and extent of research evidence related to PC in ESLD patients awaiting LT. The review was carried out by one reviewer and was supervised by two experts, one hepatologist and one PC specialist.
Search Strategy
We searched for evidence-based articles in the following electronic databases: Medline (PubMed), Scopus and Web of Knowledge. The search strategy was limited to all English language articles published until June 6, 2019. The terms “palliative care” and “end-stage liver disease” were used as keywords. The key concepts resulted in 25 articles in Pubmed, 84 articles in Scopus and 115 articles in Web of Knowledge. Additionally, 6 studies were found after searching the references or articles included from the search databases.
Inclusion Criteria
Only studies involving PC in ESLD patients and a population over 18 years old were included.
Exclusion Criteria
Articles written in languages other than English were excluded. Editorials, letters to the editor, comments and narrative case reports were excluded, as well as articles that did not include patients waiting for LT.
Data Synthesis and Data Collection Process
Detailed information of the articles included was categorized by major themes: symptom burden; perspectives of life-sustaining treatment and comfort for patients, families and health care professionals; goals of care discussions; patient and family needs; quality of life; PC and survival; referral to PC, barriers and opportunities; integration of PC; outpatient care and cost-effectiveness analysis. Data extraction was done manually, without resorting to any extraction software. Quality review was not assessed as the purpose of this review is to scan the current literature in order to determine what has been reported and what needs to be investigated related to PC in ESLD patients awaiting LT.
Results
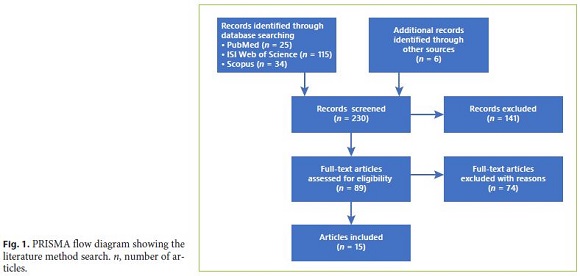
A total of 230 articles were reviewed for inclusion using the keywords. The articles were then screened and further eliminated after reviewing the abstracts, with 89 retained for further reading. Of these, only the 15 articles that met the inclusion criteria were selected. A flow diagram following PRISMA guidelines [8] showing all literature procedures as well as the resulting number of articles selected is displayed in Figure 1. An overview of the 15 articles included is presented in Tables 1 and 2 with the articles organized according to publication date [9–23]. Data gathered from the articles were summarized using percentages and frequencies for descriptive purposes.
Most studies originated in North America (n = 12) or in Europe (n = 3). Studies predominantly used quantitative (n = 9) or mixed (n = 4) designs. We found only surveys, mostly prospective (n = 11).
Study populations included patients, carers and health care professionals. The male gender predominated, and the median age of patients ranged from 51 to 62 years. Ten main themes were addressed: symptom burden; perspectives of life-sustaining treatment and comfort for patients, families and health care professionals; goals of care discussions; patient and family needs; quality of life; PC and survival; referral to PC, barriers and opportunities; integration of PC; outpatient care and cost-effectiveness analysis.
Symptom Burden
Few studies addressed directly symptoms in ESLD patients awaiting LT. An early PC intervention study has found that the most commonly reported symptoms were fatigue, sleep disorders and pruritus [9]. In another study patients reported lack of energy, pain, sleep disorders and drowsiness as the most frequent, severe and distressing symptoms [10]. Other frequent and severe symptoms were dry mouth, lack of concentration and itching. Lack of concentration was considered more distressing than dry mouth.
A qualitative interview study of patients and bereaved carers found deteriorating physical health was compounded by ongoing psychological issues, commonly relating to alcohol dependence, including depression and guilt related to the nature of the disease [11].
Attitudes toward symptom management, such as pain in ESLD patients, were evaluated and showed that 30–40% of participants, despite having moderate pain, reported using no pain medication. The patient who used it reported having less than 50% relief and were only moderately satisfied with their overall pain treatment. Moreover, although 8 out of the 11 patients who were not LT candidates took a strong opioid, only 2 out of the 9 patients awaiting LT were given the same pain relief treatment [12]. In a survey of LT service providers [13], nurses, postgraduate year 1 medical and surgical trainees were less likely to agree that LT providers were proficient in managing pain and depression than attending physicians. Also, postgraduate year 1 medical and surgical trainees (86%) and attending physicians (100%) were reported more likely to avoid using opioid medication to treat pain in these patients than nurses (62%) (p = 0.0001).
Perspectives of Life-Sustaining Treatment and Comfort for Patients, Families and Health Care Professionals
An intensive care unit prospective study that included 6 patients (all considered for LT), 19 family members and 122 health care professionals revealed that the decision trajectory and the reasoning behind the life-sustaining treatment and comfort care decisions are resumed by the metaphor “on the train” [14]. The use of this expression enabled patients and family members to conceptualize their experience of the decision-making process – patients and families are in the train, where each life-sustaining treatment decision is a “train station,” a place where they can theoretically choose to disembark but they feel that they have little choice to do it. In the same study, Hansen et al. [14] stated that 4 subthemes became evident during the patients’ stay in the intensive care unit: (i) for families, life was the obvious answer, the purpose of lifesustaining treatment decisions was to keep the patient alive and headed toward the goal of LT; (ii) excluding families from “minor” life-sustaining treatment decisions added to their limited preparedness for major ones that followed; (iii) multiple professionals, each with a narrow focus, infrequently explained to family members how the function of an organ interrelated with the function of other organs or what it meant in the context of the overall picture of the patient’s illness; (iv) different perceptions of the patients’ illness course among specialities, between professions, and between professions and patients/families.
A structured PC intervention study in the surgical intensive care unit showed that, during the intervention period, the number of patients without resuscitation status significantly increase over time amongst those who died (from 52 to 81%, p = 0.03) [15]. The mean length of stay decreased, both in those who died and those who survived in the intensive care unit. Withdrawal of ventilator, pressors and nutritional support increased significantly in the intervention period.
Goals of Care Discussions
Goals of care discussions seem to be less common in patients considered for LT [15], and we found different perspectives from different professionals in the survey of Beck et al. [13]: a vast majority of nurses (96%) and postgraduate year 1 medical and surgical trainees (91%) responded that it was appropriate to hold goals of care discussions during clinical visits with the patient’s primary care provider, while only about a third of attending physicians (31%) agreed (p = 0.0001). In contrast, more attending physicians (69%) thought it was appropriate for a patient’s hepatologist to have goals of care discussions during clinical visits, with 100% of nurses and 91% of postgraduate year 1 medical and surgical trainees agreeing.
PC intervention studies revealed different results: in the intensive care unit [15] setting goals of care discussion increased from 2 to 39%, while in an outpatient early PC intervention study [9] it did not significantly increase rates of advance directive documentation.
Patient and Family Needs
Patients with ESLD who die while awaiting transplantation seems to have greater unmet needs for PC than other decedents, even if all received relatively aggressive care during their terminal hospitalization [15].
Two studies addressed indirectly some patient and family needs [11, 21]. Physical health problems and ongoing psychological issues (related or not with alcohol and other dependences) were identified as associated to physical disability, financial insecurity and the risk of increasing isolation [11]. Some patients feared advance care planning would result in a loss of hope and referred uncertainties about disease trajectory. Regarding LT, being assessed unsuitable was considered as an uniquely difficult period [11]. Families were perceived to be in need of support themselves, requiring frequent reassurance as the patient’s condition deteriorated [21]. Caregiving was associated with psychological distress (particularly relating to ongoing alcohol use and hepatic encephalopathy) and deprioritization of individual needs [11].
Quality of Life
None of the selected articles assessed quality of life directly. Beck et al. [13] reported that patients and their families value goals of care discussions and were grateful for PC. Responses from the Family Quality of Dying and Death questionnaire, after a structured PC intervention in the surgical intensive care unit [15], revealed a trend toward improvements in “time with family and friends,” breathing comfort, spiritual services, presence at time of death and overall physician care.
PC, LT and Survival
The study of Medici et al. [20] reported that 4 of the 6 transplanted patients experienced an improvement of their MELD score during hospice stay, suggesting that this service can potentially provide effective care to terminally ill patients. None of the other studies revealed data regarding the impact of PC on prognosis.
Referral to PC, Barriers and Opportunities
The included studies revealed different rates of referral of ESLD patients to PC, ranging from 4.5 to 29.1% [13, 17, 18], with an increasing tendency over the past 10–15 years [13, 18, 19].
Specifically from patients awaiting LT who died, only 2% received PC consultation [13] and in a nation-wide US weighted sample of 59,687 patients dying in the hospital with decompensated liver disease from 2009 to 2013, 18,027 (29.1%) received a PC consultation during the hospitalization and 331 patients were awaiting or received LT (1.9%) [19]. A study about the utility of the MELD (Model for End-Stage Liver Disease) score in transplant candidates and simultaneous hospice referral described a 5% rate (8/157) of referral to hospice care [20].
Factors associated with low PC referral included African-American, Hispanic and Asian ethnicity [18, 19] and absence of insurance coverage [18]. Factors associated with increased referral to PC were older age [17, 18], Caucasian ethnicity [17], “do not resuscitate” status [18], treatment in a teaching hospital [18, 19], in medium [18] and large-sized hospitals [18, 19], presence of hepatocellular carcinoma [18], presence of metastatic cancer [18], higher MELD score at listing [17, 20] and at delisting [17] and higher Charlson comorbidity index [19]. Decedents who were listed or received LT during admission were also less likely to receive PC than those who were not listed for LT [19].
Late referrals to PC among patients who died awaiting transplantation were identified by Kathpalia et al. [17], who found that the median number of days between PC consultation and death was 4. Different perspectives were identified by Beck et al. [13] among different professional groups, with nurses (88%) and postgraduate year 1 medical and surgical trainees (63%) being more likely than attending physicians (44%) to report that there were patients for whom they wished they had consulted PC earlier (p = 0.001). Attending physicians were less likely than nurses or postgraduate year 1 medical and surgical trainees to agree that it is appropriate to consult PC when the patient is diagnosed with ESLD, when the patient is listed for transplantation or when a patient with ESLD is admitted to the hospital for any reason. In contrast, the majority of attending physicians agreed that it is appropriate to consult PC when the patient is imminently dying [13]. In another study, the majority of LT service surgeons felt that PC should have been introduced earlier in the patient course, but only a few considered that there was a delay in the institution of PC under their care [15].
Attending physicians, more than any other group, were identified by all respondents (including attending physicians themselves), as creating a barrier to involving PC in the care of their patients [13]. In addition, they were much more likely than nurses and postgraduate year 1 medical and surgical trainees to identify the patient and family members as creating a barrier to PC consultation. Many respondents cited lack of clear criteria for involving PC and difficulty prognosticating end of life in ESLD patients as significant barriers. In a qualitative study involving general practitioners from the UK [21], the main concerns identified were those relating directly to the condition (symptom management and the need to combine a PC approach with ongoing medical interventions), issues arising from patients’ social circumstances (stigma, social isolation and the social consequences of liver disease) and deficiencies in the organization and delivery of services.
Benefits of PC were verified on life-sustaining treatments [19], goals of care discussions [15] and symptom management reported in the early PC intervention study [9]. As a matter of fact, these studies found a 50% improvement of the initial moderate-to-severe pruritus, and of the general well-being, appetite, anxiety and fatigue. Pain, myalgia, sexual dysfunction, sleep disturbance and dyspnea also showed improvement, but this improvement did not reach statistical significance, and the early intervention also decreased depression (27.8%). An American study identified a significantly lower mean of total costs and length of stay for patients who received PC consultation in its terminal hospitalization, with an association of PC consultation with reduced hospital length of stay and reduction in nearly all procedures [19].
Integration of PC
A qualitative study on the incompatibility of health care services and end-of-life needs in advanced liver disease reported that patients relied on hospital services for most aspects of care, with general practitioners often being bypassed in decision-making and perceived as being unaware of ongoing developments [11]. On the other hand, general practitioners consider themselves as likely to have an established relationship with the patient and a greater understanding of their social situation and needs, whereas specialists offer expert knowledge on liver disease and treatment options [21]. They highlighted the importance that primary care physicians place on being able to provide a coordinating role but only when supported by members of the specialist teams. Managing complex and unusual symptoms, or judging when to introduce a PC approach, for instance, would benefit from this collaboration. Collaborative working with the support from specialist hospital clinicians was regarded as essential, with general practitioners acknowledging their own lack of experience and expertise in this area. Further training of general practitioners and PC professionals on issues specific to liver disease were referred in another study [22]. Improved awareness of supportive care on symptom control, advanced communication and prognosis discussion for all professionals, and better knowledge of how PC professionals can support general practitioners and liver specialists were also referred as important measures [22]. A study of proactive case finding to improve concurrently curative and PC in patients with ESLD showed that patients in the quality improvement project were more likely to be considered for LT (77.6%, p < 0,001), to have their transplant evaluation completed (22.4%, p = 0,01) and to receive PC (62.5%, p = 0.38) [23].
Outpatient Care
Of the 15 studies selected, 1 took place in the hospice [20], 8 studies exclusively included inpatients [13–19, 23] and 4 studies were developed in the outpatient setting [9– 12]. Of the 4 studies that included only health care professionals, 2 also considered the outpatient context [21, 22].
From the published results it is not possible to assess that there are differences between the needs of inpatients and those of outpatients. Baumann et al. [9] reported that after the early palliative care intervention in the outpatient setting, 50% of moderate to severe symptoms improved and 43% of patients showed improvement in clinically significant depressive symptoms, greater in those with more symptoms.
In another 2 studies [21, 22], many general practitioners felt unable to manage advanced cirrhosis in the community. All health care professional groups seem to wish to increase community provision of PC support and recognized that they required further training to improve their skills in caring for people with ESLD [22]. Service configuration was one of the key areas identified for future research [22].
Cost-Effectiveness Analysis
Based on the National Inpatient Sample (national data set across the USA) having been listed or receiving LT during the hospitalization was associated with higher overall costs compared to the unlisted status [19]. In this study, Patel et al. [19] reported that PC consultation was associated with lower costs and procedure burden at the end of life.
Discussion
We have identified 15 studies which met the inclusion criteria. Studies were quite diverse on themes, including symptom burden in ESLD patients to life-sustaining treatment decisions or integration of PC. There were also differences on the populations studied, all studies included patients with ESLD awaiting LT, but some also included noneligible LT patients. The authors found no randomized controlled trials. In accordance with previous literature male patients under 65 years old predominate [24].
In a global perspective, the studies considered in this review reported significant PC needs of ESLD patients awaiting LT and some benefits of PC but still an inadequate response to these needs, with challenging barriers to better integration of PC for patients awaiting LT.
Symptoms such as fatigue and sleep disturbance were the most frequent and severe symptoms identified [9, 10] similar to what has been described in a recent meta-analysis [25]. Pain was also reported in one of the included studies [10]. In contrast, breathlessness and sexual dysfunction were not mentioned as they had been in the same meta-analysis [25], with sexual dysfunction not even being evaluated, which suggests that it should also be included in future symptom assessments. Psychological needs were identified but apparently not in the same manner by all professionals, as recommended [11, 13]. A significant burden from psychological symptoms, such as depression, was also identified in more than 50% of ESLD patients included in an Italian survey [26], and anxiety was reported in pretransplantation patients ranging from 27 to 44% [27, 28]. The experience of waiting for a LT has considerable impact on patients [29]. Qualitative studies have described uncertainty as the cornerstone of this psychological process, with very diverse perspectives being reported by patients: some expressed joy and relief and regarded transplantation as an opportunity; others manifested a sense of danger at facing the likelihood of death and of developing cancer during the waiting period [30, 31]. Difficulty coping, loss of trust in physicians and medical, personal and social uncertainties have all been reported [30–32]. LT patients with a coexisting history of substance abuse, in particular, would probably benefit from special attention [33], since this population tends to be threatened by negative attitudes of health care professionals, has a significant risk of noncompliance to treatment and might have special concerns about both symptom management and caregivers’ support.
Despite the significant symptom burden, symptom management is still probably suboptimal as suggested by low rates of pain relief [12] and inappropriate professional skills [13]. Adequate medication in ESLD is challenging, since most drugs are metabolized in the liver, thus putting patients at a higher risk of adverse effects. As a result, physicians often resort to less aggressive symptom management. Moreover, physicians may avoid the prescription of opioids to those with a history of substance abuse and often fear the side effects of opioids (e.g., constipation and worsened encephalopathy) [34].
Although there were few studies that directly evaluate the impact of PC in LT patients, most of them identified potential benefits, not only in symptom management [9], but also in goals of care discussions [15], in life-sustaining treatment decisions [19] and even in direct and indirect health costs [19]. Similar results have been reported in patients awaiting other organ transplants [35–37]. There is an inherent difficulty in discussing goals of care and advanced directives with patients pursuing curative therapies, but as suggested by Potosek et al. [34] it is imperative to discuss those and to identify health care proxies, as encephalopathy can impair decision-making. Regarding cost-effectiveness analysis, more studies are required.
Only 2 studies indirectly addressed the quality of life of patients with ESLD [13, 15]. Both favored the PC approach which has a beneficial impact on it. However, robust studies that specifically assess quality of life are essential as one of the cornerstones of the overall PC approach.
The study of Medici et al. [20] reported an improvement of their MELD score during hospice stay, suggesting that this service can potentially provide effective care to terminally ill patients. Although no other study has directly assessed the impact of PC on the prognosis and survival of ESLD patients, it is expected that this might be positive, similarly to studies regarding other medical conditions [38].
Referrals of LT patients to PC seem to be increasing but are still quite low and probably occur only in very late stages of the disease, putting patients at risk for decreased quality of care at the end of life [13, 17–19]. Many barriers have been identified, considering patients, carers, health care professionals and services. The “on the train” perspective hinders the ability of all the interveners to consider a simultaneous approach of PC while awaiting transplantation [14]. Kathpalia et al. [17] considered that these patients represent a unique subgroup of patients with a terminal condition – by virtue of having ESLD – but await the promise of a cure through LT. In this setting, PC, which traditionally has been considered only for those “at the end of life,” may be perceived – by both the patient and providers alike – as unnecessary and unwelcome. More and appropriate education of health care professionals and training is probably necessary, as suggested in surveys analyzed here [13, 18, 19, 21, 22].
Integration of PC in LT patients seems to be considered essential by all parts [13, 15, 21, 22]. Transplant candidates not only benefit from being provided PC, since they suffer from a terminal condition with significant needs, but also require a complete and complex medical care even when their condition is very advanced [39]. Also, LT patients who are removed from the waiting list often experience withdrawal of specialty care, feelings of abandonment and likely imminent death [34], all of which must be addressed. Development of clinical triggers for PC consultation and effective collaborative approach may clarify better integration [21].
This review was limited by the restricted number of articles included, written only in English, which resulted in a data set that is limited to North American and European ESLD patients that may not take into consideration other relevant realities. Note also that important differences regarding design of the studies may have resulted in significant data heterogeneity, which is beyond the scope of this review since quality assessment was not evaluated.
Conclusions
This review found notable discrepancy between the need for PC and its use in ESLD patients awaiting LT. The belief that transplantation and PC are mutually exclusive still prevails. However, there is increasing evidence that the strategy of providing PC alongside disease-directed therapy while awaiting LT might benefit patients, carers and even the health system. This review indicates some potential areas for developing shared care models. Further research is required, with more robust studies, to better define the optimal strategy of the best way of PC integration for ESLD patients awaiting LT.
References
1 Mokdad AA, Lopez AD, Shahraz S, Lozano R, Mokdad AH, Stanaway J, et al. Liver cirrhosis mortality in 187 countries between 1980 and 2010: a systematic analysis. BMC Med. 2014;12:145. [ Links ]
2 Kotzeva M, editor. European social statistics (Eurostat Pocketbooks). Luxembourg:Eurostat;2013. [ Links ]
3 Perri GA, Bunn S, Oh YJ, Kassam A, Berall A, Karuza J, et al. Attributes and outcomes of end stage liver disease as compared with other noncancer patients admitted to a geriatric palliative care unit. Ann Palliat Med. 2016 Apr;5(2):76–82.
4 Schuppan D, Afdhal NH. Liver cirrhosis. Lancet. 2008 Mar;371(9615):838–51.
5 Peng JK, Hepgul N, Higginson IJ, Gao W. Symptom prevalence and quality of life of patients with end-stage liver disease: a systematic review and meta-analysis. Palliat Med. 2019 Jan;33(1):24–36.
6 Lamba S, Murphy P, McVicker S, Harris Smith J, Mosenthal AC. Changing end-of-life care practice for liver transplant service patients: structured palliative care intervention in the surgical intensive care unit. J Pain Symptom Manage. 2012 Oct;44(4):508–19.
7 Poonja Z, Brisebois A, van Zanten SV, Tandon P, Meeberg G, Karvellas CJ. Patients with cirrhosis and denied liver transplants rarely receive adequate palliative care or appropriate management. Clin Gastroenterol Hepatol. 2014 Apr;12(4):692–8.
8 Moher D, Liberati A, Tetzlaff A, Altman DJ. The PRISMA group (2009) preferred reporting items for systematic reviews and metaanalyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. [ Links ]
9 Baumann AJ, Wheeler DS, James M, Turner R, Siegel A, Navarro VJ. Benefit of early palliative care intervention in end-stage liver disease patients awaiting liver transplantation. J Pain Symptom Manage. 2015 Dec;50(6):882–6.e2.
10 Hansen L, Leo MC, Chang MF, Zaman A, Naugler W, Schwartz J. Symptom distress in patients with end-stage liver disease toward the end of life. Gastroenterol Nurs. 2015;38(3):201–10.
11 Hudson B, Hunt V, Waylen A, McCune CA, Verne J, Forbes K. The incompatibility of healthcare services and end-of-life needs in advanced liver disease: A qualitative interview study of patients and bereaved carers. Palliat Med. 2018 May;32(5):908–18.
12 Hansen L, Leo MC, Chang MF, Zucker BL, Sasaki A. Pain and self-care behaviours in adult patients with end-stage liver disease: a longitudinal description. J Palliat Care. 2014;30(1):32–40.
13 Beck KR, Pantilat SZ, O’Riordan DL, Peters MG. Use of palliative care consultation for patients with end-stage liver disease: survey of liver transplant service providers. J Palliat Med. 2016;19(8):836–42.
14 Hansen L, Press N, Rosenkranz SJ, Baggs JG, Gray EN, Kendall J, et al. Life-sustaining treatment decisions in the ICU for patients with end-stage liver disease: a prospective investigation. Res Nurs Health. 2012;35(5):518–32.
15 Lamba S, Murphy P, McVicker S, Smith JH, Mosenthal AC. Changing end-of-life care for liver transplant service patients: structured palliative care intervention in the surgical intensive care unit. J Pain Symptom Manage. 2012;44(4):508–19.
16 Walling AM, Asch SM, Lorenz KA, Wenger NS. Impact of consideration of transplantation on end-of-life care for patients during a terminal hospitalization. Transplantation 2013;95(4):641–6.
17 Kathpalia P, Smith A, Lai JC. Underutilization of palliative care services in the liver transplant population. World J Transplant. 2016;6(3):594–598.
18 Rush B, Walley KR, Celi LA, Rajoriya N, Brahmania M. Palliative care access for hospitalized patients with end-stage liver disease across the United States. Hepatology. 2017;66(5):1585–91.
19 Patel AA, Walling AM, May FP, Saab S, Wenger N. Palliative care and healthcare utilization for patients with end-stage liver disease at the end of life. Clin Gastroenterol Hepatol. 2017;15(10):1612–9.
20 Medici V, Rossaro L, Wegelin JA, Kamboj A, Nakai J, Fisher K, et al. The utility of the model for end-stage liver disease score: a reliable guide for liver transplant candidacy and for select patients, simultaneous hospice referral. Liver Transplant. 2008;14(8):1100–6.
21 Standing H, Jarvis H, Orr J, Exley C, Hudson M, Kaner E, et al. How can primary care enhance end-of-life care for liver disease? Qualitative study of general practitioners' perceptions and experiences. BMJ Open 2017;7:e017106. [ Links ]
22 Low J, Vickerstaff V, Davis S, Bichard J, Greenslade L, Hopkins K. Palliative care for cirrhosis: a UK survey of health professionals’ perceptions, current practice and future needs. Frontline Gastroenterol. 2016;7(1):4–9.
23 Wailling AM, Schreibeis-Baum H, Pimstone N, Asch SM, Robinson L, Korlekar S, et al. Proactive case finding to improve concurrently curative and palliative care with endstage liver disease. J Palliat Med. 2015;18(4):378–81.
24 Effiong K, Osinowo A, Pring A. Deaths from liver disease: implications for end of life care in England. Bristol: National End of Life Care Intelligence Network;2012. [ Links ]
25 Peng JK, Hepgul N, Higginson I, Gao W. Symptom prevalence and quality of life of patients with end-stage liver disease: a systematic review and meta-analysis. Palliat Med. 2019;33(1):24–36.
26 Bianchi G, Marchesini G, Nicolino F, Graziani R, Sgarbi D, Loguercio C, et al. Psychological status and depression in patients with liver cirrhosis. Dig Liver Dis. 2005 Aug;37(8):593–600.
27 Singh N, Gayowski T, Wagener MM, Marino IR. Depression in patients with cirrhosis. Impact on outcome. Dig Dis Sci. 1997 Jul;42(7):1421–7.
28 Santos GR, Boin IF, Pereira MI, Bonato TC, Silva RC, Stucchi RS, et al. Anxiety levels observed in candidates for liver transplantation. Transplant Proc. 2010 Mar;42(2):513–6.
29 Kanwal F, Hays RD, Kilbourne AM, Dulai GS, Gralnek IM. Are physician-derived disease severity indices associated with health-related quality of life in patients with end-stage liver disease? Am J Gastroenterol. 2004 Sep;99(9):1726–32.
30 Bjork IT, Naden D. Patients’ experiences of waiting for a liver transplantation. Nurs Inquiry. 2008;15(4):289–98.
31 Brown J, Sorrell JH, McClaren J, Creswell JW. Waiting for a liver transplant. Qual Health Res. 2006 Jan;16(1):119–36.
32 Martin SC, Stone AM, Scott AM, Brashers DE. Medical, personal, and social forms of uncertainty across the transplantation trajectory. Qual Health Res. 2010;20(2):182–96.
33 Koch M, Banys P. Liver transplantation and opioid dependence. JAMA. 2001 Feb;285(8):1056–8.
34 Potosek J, Curry M, Buss M, Chittenden E. Integration of palliative care in end-stage liver disease and liver transplantation. J Palliat Med. 2014(11):1271–7.
35 Freeman N, Le LW, Singer LG, Colman R, Zimmermann C, Wentlandt K. Impact of a transplant palliative care clinic on symptoms for patients awaiting lung transplantation. J Heart Lung Transplant. 2016;35(8):1037–9.
36 Wentlandt K, Dall’Osto A, Freeman N, Le LW, Kaya E, Ross H, et al. The transplant palliative care clinic: an early palliative care model for patients in a transplant program. Clin Transplant. 2016;30(12):1591–6.
37 Schwarz ER, Baraghoush A, Morrissey RP, Shah AB, Shinde AM, Phan A, et al. Pilot study of palliative care consultation in patients with advanced heart failure referred for cardiac transplantation. J Palliat Med. 2012;15(1):12–5.
38 Cardenas A, Ginès P. Management of complications of cirrhosis in patients awaiting liver transplantation. J Hepatol. 2005;42(1 Suppl):S124–33.
39 Hoerger M, Wayser GR, Schwing G, Suzuki A, Perry LM. Impact of interdisciplinary outpatient specialty palliative care on survival and quality of life in adults with advanced cancer: a meta-analysis of randomized controlled trials. Ann Behav Med. 2019 Jun;53(7):674–85.
Statement of Ethics
The authors have no ethical conflicts to disclose.
Disclosure Statement
The authors have no conflict of interest to declare.
Funding Sources
The authors have no funding source to declare.
* Corresponding author.
Sara Vieira Silva
Equipa Intra-Hospitalar de Suporte de Cuidados Paliativos
Serviço de Medicina, Centro Hospitalar e Universitário do Porto
Largo Abel Salazar, PT–4050 Porto (Portugal)
Received: November 10, 2019; Accepted: March 17, 2020
Author Contributions
Sara Vieira Silva contributed to the conception of the work, acquisition, analysis and interpretation of the data work, drafted the work and gave the final approval of the version to be published. Elga Freire contributed to the conception of the work, writing of the results, discussion and conclusions, to revising it critically for important intellectual content and gave the final approval of the version to be published. Helena Pessegueiro contributed to the conception of the work, writing of the results, discussion and conclusions, to revising it critically for important intellectual content and gave the final approval of the version to be published.














