Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.27 no.6 Lisboa dez. 2020
https://doi.org/10.1159/000507224
CLINICAL CASE STUDY
The Usefulness of an Endoscopic OverStitch Suturing System for Managing Anastomotic Dehiscence – A Case Report
Utilidade do Sistema Endoscópico de Sutura OverStitch para o Tratamento de uma Deiscência Anastomótica – Um Caso Clínico
Gaurav Patil,Arun Iyer, Ankit Dalal, Amit Maydeo
Baldota Institute of Digestive Sciences, Global Hospitals, Mumbai, India
* Corresponding author.
ABSTRACT
Anastomotic dehiscence (AD) after colorectal surgery contributes to poor outcomes resulting in multiple postoperative complications. Conventional management would be a repeat laparotomy and tension suturing. But owing to the unhealthy vicinities near the suture lines, there is a significant risk of technical failure which further increases postoperative morbidity and mortality. A 60-year-old male, with a history of hypertension, ischemic heart disease, and previous percutaneous transluminal coronary angioplasty, underwent sigmoid colectomy with colorectal anastomosis for complicated sigmoid diverticulitis. He then developed anastomotic site leak for which an ileostomy was done. Prior to the ileostomy revision, he was referred for colonoscopic evaluation which showed the persistence of a partial AD. We decided to close the defect endoscopically with the Apollo OverStitch device. Initial tissue preparation was done by creating a surgical surface using argon plasma coagulation at the perimeter of the leak site. A double channel therapeutic endoscope with the OverStitch assembly was passed to take full-thickness running sutures across the rent to facilitate full closure. The area examined showed good suture approximation and complete closure. The procedure was successful with no immediate or delayed postprocedural complications. Repeat endoscopic evaluation at about two weeks showed well-approximated edges with intact suture lines, and there was complete resolution of the leak. The patient subsequently underwent revision surgery after a month. The patient is under close follow-up and doing well. The Apollo OverStitch device has certainly opened new avenues in flexible endoscopic surgery which need further exploratory studies to add to existing promising results.
Keywords: Anastomotic dehiscence, Leak, Postoperative complications, Endoscopic suturing system
RESUMO
A deiscência anastomótica (DA) após a cirurgia colorretal contribui para piores resultados, resultando em múltiplas complicações pós-operatórias. A terapêutica convencional passa por repetir a laparotomia e uma sutura de tensão. Mas devido às condições locais perto das linhas de sutura há um risco significativo de falência técnica, o que aumenta ainda mais a morbimortalidade destes doentes. Neste caso um homem de 60 anos com história de hipertensão e cardiopatia isquémica com angioplastia coronária percutânea prévia foi submetido a colectomia do sigmóide com anastomose colorretal, devido a uma diverticulite do sigmóide complicada. Verificou-se deiscência da anastomose pelo que uma ileostomia foi realizada. Antes do encerramento da ileostomia o doente realizou colonoscopia que evidenciou persistência parcial da DA. Foi decidido encerramento endoscópico da DA utilizando o sistema de sutura Apollo OverStitch. O tecido foi inicialmente preparado através da criação de uma superfície cirúrgica utilizando coagulação com argon plasma dos bordos da DA. Foi utilizado um endoscópio terapêutico de duplo canal montado já com o sistema de OverStitch de forma a possibilitar suturas continuas transmurais, facilitando o encerramento da fístula. A área intervencionada mostrou uma boa aproximação dos bordos da sutura e um encerramento completo. O procedimento foi um sucesso, sem complicações imediatas ou tardias. A endoscopia de reavaliação duas semanas depois mostrou os bordos bem aproximados com linhas de sutura intactas com resolução completa de DA. A revisão cirúrgica foi efetuada um mês depois e o doente está clinicamente bem. O sistema de sutura Apollo OverStitch abre novas possibilidades na cirurgia endoscópica flexível, sendo necessários mais estudos exploratórios a acrescentar evidência aos promissores resultados já existentes.
Palavras-Chave: Deiscência anastomótica, Complicações pós-operatórias, Sistema de sutura endoscópico
Introduction
Anastomotic dehiscence (AD) is the most feared among all complications by colorectal surgeons [1]. It represents a failure of technique even in experienced hands. There is an increased risk of technical failure in such cases owing to the unhealthy vicinities near the suture lines. The incidence of AD with subsequent leaks is 2–30% [2, 3]. These leaks have a mortality of 5–36% [4–6]. Early hospital discharge after surgery has been associated with an increase in the number of patients returning with anastomotic leak. Outpatient diagnosis of AD delays diagnosis and further intervention with a negative influence on patient outcome. Recent innovations in endoscopy have resulted in the development of endoscopic closure techniques. Through the scope, clips have shown promising results in successful endoscopic closure of perforation and leaks. The OverStitch endoscopic suturing system (Apollo Endo-surgery, Austin, TX, USA) allows the placement of full-thickness sutures. To the best of our knowledge, there is only a single video case which has been reported on the closure of AD with this device [7].
Case Presentation
A 60-year-old male, with a history of hypertension, ischemic heart disease, and previous percutaneous transluminal coronary angioplasty, underwent sigmoid colectomy with colorectal anastomosis for complicated sigmoid diverticulitis – Hinchey classification (stage 2 disease). The procedure was complicated with anastomotic site leakage for which he underwent ileostomy. Two months later, he was planned for ileostomy closure, hence he was referred to our hospital for routine colonoscopic evaluation to look for any persistence of anastomotic leak.
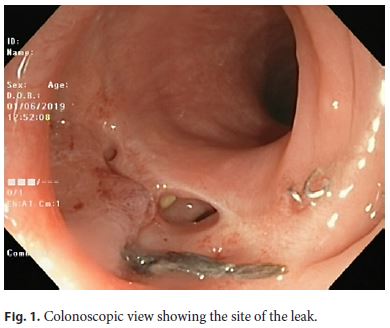
An abdominal computed tomography (CT) scan was done which showed the presence of a 1.8 × 1.1 cm sealed-off collection around the anastomotic site. The patient was under broad-spectrum antibiotics for aerobic and anaerobic cover. Colonoscopy showed the persistence of a partial AD (Fig. 1). The distance to the anastomosis from the anal verge was 20 cm, the size of the defect was about 2.5 cm. The development of an anastomotic leakage was evident 1 week after the procedure. It was noticed during the same admission of the emergent surgery. After explaining the role of endoscopic suturing for a small defect versus a repeat surgery to the patient, it was decided to proceed with endoscopic suturing.
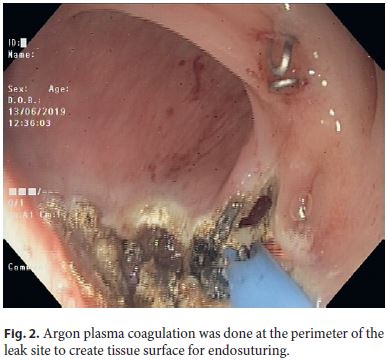
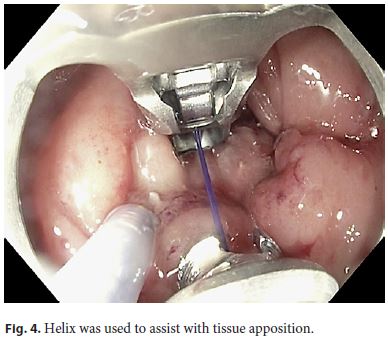
The procedure was carried out with the patient in the left lateral position, using CO2 insufflation, under total intravenous anesthesia. Initial tissue preparation was done by creating a surgical surface using argon plasma coagulation (energy settings of Pulsed APC with a flow rate of 1.2 L/min [end-firing, 55 W]) at the perimeter of the leak site (Fig. 2). A double-channel therapeutic endoscope with the Over-Stitch assembly was passed along with an overtube to take full-thickness running sutures across the rent to facilitate full closure (Fig. 3, 4). The edges of the rent were further reinforced with another layer of suturing. The area examined showed good suture approximation and complete closure (Fig. 5). The procedure was successful with no postprocedural complications.

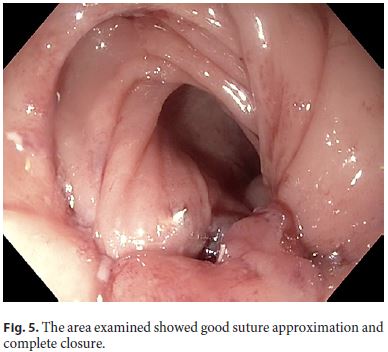
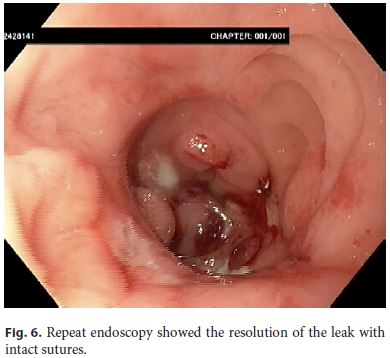
Repeat endoscopic evaluation after around 2 weeks showed resolution of the leak with intact sutures (Fig. 6). The patient subsequently underwent revision surgery with closure of the ileostomy after a month. He was discharged and managed without complications as an outpatient for 4 weeks. Currently, he is under close follow-up and doing well.
Discussion
Colectomy with colorectal anastomosis is technically challenging, and repeat operative surgeries are sometimes unavoidable [8]. Risk factors for a dehiscence and leak are classified as extraperitoneal or intraperitoneal based on anastomosis. This is an unusual case of AD which has been treated successfully with the OverStitch assembly. In conventional settings, the management of anastomotic leaks is cumbersome, subjecting the patient to multiple surgeries and the subsequent increased risk for complications like intraabdominal adhesions [9]. Moreover, it requires adequate expertise to manage such cases surgically, and even in safe hands, there is an increase in the risk of complications, risk from anesthesia, increased time for postoperative recovery, and increase in analgesic use. This could also result in an increase in overall health care expenditure.
An increased risk for AD was seen in patients who had an ASA score ≥3, prolonged operative time (> 3 h), and rectal location of the disease [10]. Some of these determinants that influence outcomes of surgery need to be considered in perioperative decision-making to avert leakage. However, with the advent of novel accessories in endoscopy and an apt collaborative work of surgery with endoscopy, new avenues have opened up for the endoscopist.
CT scans have been found to be effective in identifying patients with anastomotic leaks, in 65–89% of all patients [2, 11]; while one study has shown that water-soluble enema is superior to CT imaging in delineating distal colonic anastomotic leaks [12]. A CT scan is not accurate enough to provide assurance of anastomotic integrity, and patient parameters with symptoms need to be considered. Randomized studies for identifying AD that can compare CT scans combined with rectal contrast enema versus water-soluble enema are warranted. Intraoperative colonoscopy is vital for the assessment of stapled anastomosis, as it can directly visualize the anastomosis line. In our case, we found CT was useful as it showed a collection as a result of which the case was referred for further colonoscopy evaluation. CT in this patient was done without rectal contrast, hence it might have perhaps failed to detect the leak.
The basic principles of leak management include the identification of the site of the leak, drainage of leaked contents, and disruption of the flow of intestinal fluids across the leak with diversion or closure [13]. Preparation of the lumen with APC at the perimeter of the leak site is recommended. Running interrupted sutures are usually performed in two to three layers. The OverStitch assembly is a USFDA-approved endoscopic suturing device. It has the ability to reload the suture without removing the endoscope, the ability to use tissue grasping accessories in the adjacent working channel, and a reliable depth of needle penetration. However, it is only compatible with doublechannel therapeutic endoscopes, it is large in size, and it has a limited field of view [14]. Suturing is difficult in the gastric fundus, duodenum, and colon. This becomes challenging in the colon where there is a limited working space and maneuverability of the scope, it also becomes difficult especially at bends or flexures, as it was present in our case.
Currently, there are not too many articles available on the use of this device for managing AD. Hence, a headto- head comparison is currently not feasible. Nevertheless, the OverStitch assembly has been widely used for 9 years to place stents within the gastrointestinal lumen and to perform closure of leaks and fistulas, which suggests that it can be safely used with good outcomes. The OverStitch assembly has been successfully used for the closure of iatrogenic esophageal perforations, stent fixation, mucosal defect closure, and stoma reduction after bariatric surgery [15, 16]. This device may be superior to endoclips in perforations, due to its ability to achieve full-thickness suturing and create an airtight closure [16].
Although the treatment of our patient was successful and the chosen technique appropriate, other options with different profiles in terms of safety, cost, and evidence are available; namely, but not limited to, endo-sponge application, placement of a covered self-expanding metal stent, over-the-scope clip (OTSC) positioning, and fibrin glue injection [17]. OTSC has a limited role in large perforations. There are various tips and tricks for managing postoperative challenges; however, every procedure has its own limitations and strengths. Primary anastomosis with diverting loop ileostomy appears to be a safe alternative to Hartmann’s procedure in emergent cases [18]. The primary treating surgeon felt that performing primary anastomosis with diverting ileostomy was appropriate in our patient at that point; alternatively, a two-stage Hartmann’s procedure could also have been performed.
Conclusion
Endoscopic suturing with the OverStitch device is an emerging technique for managing perforation and leaks. Although its use requires comprehensive training with a steep learning curve, it has the capability to mimic surgical closure in a minimally invasive manner. Due to the availability of limited data on its long-term use, further larger prospective and comparative studies are needed to define the role of endoscopic suturing devices in managing defects of the gastrointestinal tract.
References
1 Cong ZJ, Hu LH, Xing JJ, Bian ZQ, Fu CG, Yu ED, et al. Incidence and mortality of anastomotic dehiscence requiring reoperation after rectal carcinoma resection. Int Surg. 2014 Mar-Apr;99(2):112–9.
2 Marres CC, van de Ven AW, Leijssen LG, Verbeek PC, Bemelman WA, Buskens CJ. Colorectal anastomotic leak: delay in reintervention after false-negative computed tomography scan is a reason for concern. Tech Coloproctol. 2017 Sep;21(9):709–14.
3 Nikolian VC, Kamdar NS, Regenbogen SE, Morris AM, Byrn JC, Suwanabol PA, et al. Anastomotic leak after colorectal resection: A population-based study of risk factors and hospital variation. Surgery. 2017 Jun;161(6):1619–27.
4 Turrentine FE, Denlinger CE, Simpson VB, Garwood RA, Guerlain S, Agrawal A, et al. Morbidity, mortality, cost, and survival estimates of gastrointestinal anastomotic leaks. J Am Coll Surg. 2015 Feb;220(2):195–206.
5 Matthiessen P, Hallböök O, Andersson M, Rutegård J, Sjödahl R. Risk factors for anastomotic leakage after anterior resection of the rectum. Colorectal Dis. 2004 Nov;6(6):462–9.
6 Hedrick TL, Sawyer RG, Foley EF, Friel CM. Anastomotic leak and the loop ileostomy: friend or foe? Dis Colon Rectum. 2006 Aug;49(8):1167–76.
7 Belfiori V, Antonini F, Deminicis S, Marraccini B, Piergallini S, Siquini W, et al. Successful closure of anastomotic dehiscence after colon-rectal cancer resection using the Apollo overstitch suturing system. Endoscopy. 2017 Aug;49(8):823–4.
8 Jamali FR, Soweid AM, Dimassi H, Bailey C, Leroy J, Marescaux J. Evaluating the degree of difficulty of laparoscopic colorectal surgery. Arch Surg. 2008 Aug;143(8):762–7.
9 Kavic SM, Kavic SM. Adhesions and adhesiolysis: the role of laparoscopy. JSLS. 2002 Apr-Jun;6(2):99–109.
10 Buchs NC, Gervaz P, Secic M, Bucher P, Mugnier-Konrad B, Morel P. Incidence, consequences, and risk factors for anastomotic dehiscence after colorectal surgery: a prospective monocentric study. Int J Colorectal Dis. 2008 Mar;23(3):265–70.
11 Hyman N, Manchester TL, Osler T, Burns B, Cataldo PA. Anastomotic leaks after intestinal anastomosis: it’s later than you think. Ann Surg. 2007 Feb;245(2):254–8.
12 Nicksa GA, Dring RV, Johnson KH, Sardella WV, Vignati PV, Cohen JL. Anastomotic leaks: what is the best diagnostic imaging study? Dis Colon Rectum. 2007 Feb;50(2):197–203.
13 Thomas MS, Margolin DA. Management of Colorectal Anastomotic Leak. Clin Colon Rectal Surg. 2016 Jun;29(2):138–44.
14 Muniraj T, Aslanian HR. The use of Over- StitchTM for the treatment of intestinal perforation, fistulas and leaks. Gastrointest Interv. 2017;6(3):151–6.
15 Stavropoulos SN, Modayil R, Friedel D. Current applications of endoscopic suturing. World J Gastrointest Endosc. 2015 Jul;7(8):777–89.
16 Ge PS, Thompson CC. The Use of the Overstitch to Close Perforations and Fistulas. Gastrointest Endosc Clin N Am. 2020 Jan;30(1):147–61.
17 Singh RR, Nussbaum JS, Kumta NA. Endoscopic management of perforations, leaks and fistulas. Transl Gastroenterol Hepatol. 2018 Oct;3:85. [ Links ]
18 Lee JM, Bai P Chang J, El Hechi M, Kongkaewpaisan N, Bonde A, Mendoza AE, et al. Hartmann’s Procedure vs Primary Anastomosis with Diverting Loop Ileostomy for Acute Diverticulitis: Nationwide Analysis of 2,729 Emergency Surgery Patients. J Am Coll Surg. 2019 Jul;229(1):48–55.
Statement of Ethics
We state that the subject of this case has given his written informed consent for the publication of his case.
Disclosure Statement
There are no conflicts of interest.
Funding Sources
The authors received no grants of financial support.
* Corresponding author.
Ankit Dalal
Baldota Institute of Digestive Sciences
Global Hospitals
Mumbai, Maharashtra 400012 (India)
Received: December 15, 2019; Accepted: February 22, 2020
Acknowledgement
We thank Mr. Sehajad Vora for acting as a chief technician and assisting during the procedure. We thank Dr. Nagesh Kamat for his assistance with manuscript preparation.














