We report the case of a 67-year-old man with a previous history of appendectomy who presented to the emergency department with abdominal pain. The patient suffered from intense, diffuse, and constant abdominal pain, lasting for 3 h, but without any other associated gastrointestinal (GI) symptoms or fever.
An initial evaluation, including blood laboratory tests, electrocardiogram, abdominal radiography, and abdominal ultrasound, was performed and showed no significant changes, including absence of pneumoperitoneum and GI obstruction (Fig. 1a). The symptoms persisted despite analgesic treatment, so a computed tomography (CT) scan was performed. In the CT scan, a 32-mm arciform foreign body resembling a bone/fishbone was identified penetrating the antral wall of the stomach (Fig. 1b-d), without signs of complications (leakage, intraperitoneal gas, or locoregional liquid collections). Then, the patient mentioned that he had eaten cod the previous day, without noticing to have swallowed a fishbone.
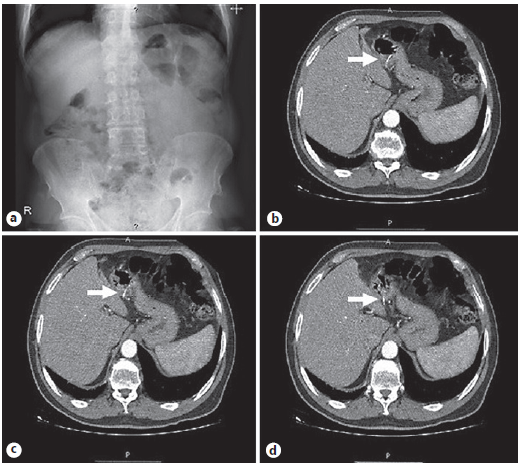
Fig. 1 Imaging study. Abdominal radiography without signs of pneumoperitoneum or GI obstruction (a). CT scan showing a linear and arciform foreign body on the antral wall of the stomach, penetrating the gastric wall (b-d).
Since the patient had no signs of perforation, such as abdominal tenderness or abdominal guarding, after discussion with the surgical team, an upper GI endoscopy was performed with the aim of removing the foreign body. Prophylactic intravenous ceftriaxone was administered before the endoscopy that was performed under deep sedation with propofol. The procedure revealed antral mucosa erosion and erythema (Fig. 2a, b), as a result of the foreign body trying to pass the pylorus. In the antrum penetrating the gastric wall, a yellow fishbone was found, without other changes in the mucosa (Fig. 2c, d). The fishbone was pulled out with alligator-tooth grasping forceps and was safely removed in a longitudinal position with the pointed end distally to the endoscope. After removal (Fig. 3a), there was no evidence of perforation of the gastric wall (Fig. 3b), and the patient remained stable, without abdominal distention or signs of peritoneal irritation. The abdominal radiography performed 6 h later did not show free air in the abdominal cavity. The patient was discharged 7 days after the procedure and was asymptomatic in the follow-up appointment 1 month later.
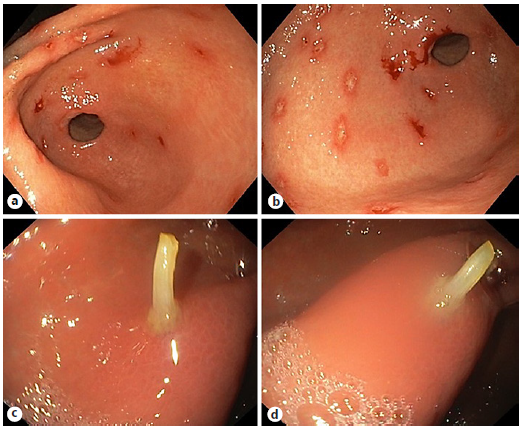
Fig. 2 Mucosal antral erosion and erythema as a result of the foreign body trying to pass the pylorus (a, b). Fishbone penetrating the gastric wall (c, d).
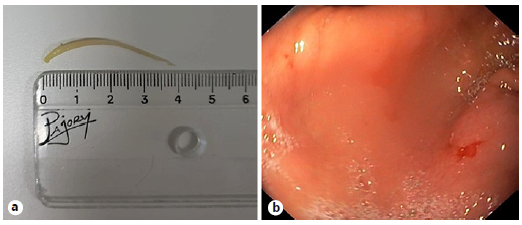
Fig. 3 Imaging showing the length of the fishbone (a). No signs of perforation or other complications in the gastric wall at the end of the procedure are present (b).
In clinical practice, foreign body ingestion is common and the majority of ingested foreign bodies pass through the GI tract spontaneously [1, 2]. However, endoscopic removal may be necessary in 10-20% of cases of foreign body ingestion, and surgery extraction is required in less than 1% [1, 2].
Fishbone penetration/perforation of the stomach is rare [3], the most common sites are the ileum, the ileocecal junction, and the rectosigmoid colon [4]. Accordingly, the diagnosis of fishbone penetration/perforation is clinically challenging, because a simple radiography imaging has a limited sensitivity of only 32%. Therefore, if a foreign body penetration/perforation is suspected, CT scan is the preferred imaging tool due to its greater sensitivity and specificity [1]. Additionally, the CT scan can also provide information about possible complications [1, 2, 4].
Generally, surgery is the recommended treatment when there is a foreign body perforation [1]. Nevertheless, like Wada et al. [3] and Ngan et al. [5] described, if penetrating fishbones are identified early, namely in the absence of or with mild peritonitis, endoscopic extraction may be possible and should be attempted. There are several devices that can be used to retrieve this kind of sharp foreign bodies (rat-tooth, alligator-tooth, or shark-tooth), the choice of retrieval device is determined by the size and shape of the foreign body and by the endoscopist’s preference and practice [1, 2]. A latex rubber hood is also very useful in this setting [1]; unfortunately, it was not available when this procedure was carried out.
Administration of antibiotics for fishbone perforation after endoscopic treatment is a controversial topic. Unlike Wada et al. [3], we just administered one dose of prophylactic antibiotic therapy, and no complications occurred.
In conclusion, cooperation with the surgical team is essential. Minimally invasive management by endoscopic removal can be a safe and effective alternative to surgery for gastric penetration by foreign bodies such as a fishbone.














