Introduction
Radiation proctitis is a common complication following pelvic radiation therapy. It can be classified either as acute or chronic proctitis based on the time of onset of symptoms after therapy [1]. Chronic radiation proctitis occurs in 5-10% of patients either as progression from the acute phase, or 3 months after therapy completion. Although not necessarily, it generally occurs in patients who suffered from severe acute proctitis [2]. There are several treatment options, which can range from medical therapy and endoscopic techniques to surgery in the refractory or severe cases [1].
Argon plasma coagulation (APC) is an endoscopic therapy for patients who failed medical treatment and remains one of the techniques most commonly reported [1]. Although it is considered a safe and effective technique, APC can be associated with rectal ulcers as post-procedure complications [3].
In most cases, rectal ulcers are asymptomatic and do not require additional monitoring or treatment [4]. For those who remain symptomatic, treatment guidelines are currently lacking in the literature. While hyperbaric oxygen (HBO) therapy has been reported as an effective treatment strategy in patients with radiation-induced rectal ulcers [5], its use has not been described in APC-induced rectal ulcers. Therefore, this is an original case report on the use of HBO therapy as a treatment of an acute ulcer as a complication after APC.
Case Report
A 72-year-old man was referred to our institution for management of rectal bleeding for 2 weeks, without other digestive symptoms. His past medical history was significant for hyperlipidemia, type 2 diabetes mellitus, and T2aN0 prostatic cancer treated 8 months earlier with external radiotherapy and chemotherapy. His current medication included simvastatin, vildagliptin, and metformin. Blood tests revealed a hemoglobin of 8.1 mg/dL with a mean corpuscular volume of 76 fL, white blood count of 6,800/mm3, and platelets of 146,000/mm3.
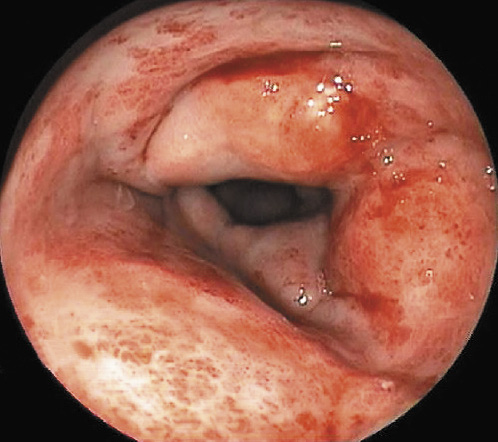
The patient underwent rectosigmoidoscopy which revealed friable and edematous rectal mucosa with multiple angioectasias, consistent with radiation proctitis (Fig. 1).
He began a 4-week course of sucralfate enemas (2 g twice daily), without clinical or endoscopic improvement on reevaluation.
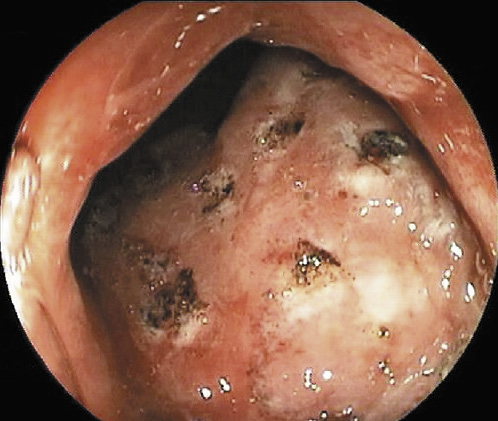
Due to persistence of rectal bleeding and endoscopic signs of radiation proctitis, APC treatment was initiated, which was applied to the bleeding areas of the mucosa with an energy level of 40 W and gas flow of 1.5 L/min (Fig. 2).
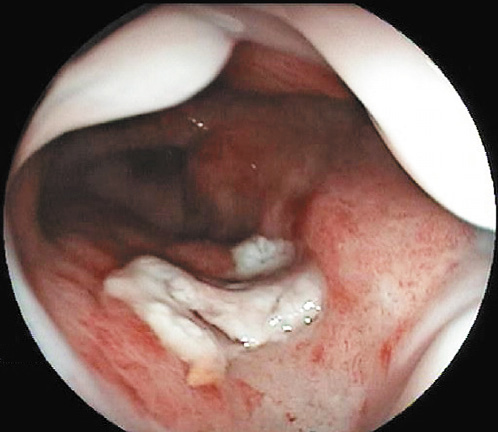
After 2 weeks, the patient reported intense proctalgia and worsening of rectal bleeding. A new rectosigmoidoscopy revealed a 10-mm ulcer, located at the site of previous APC therapy, on the anterior circumference of the low rectum (Fig. 3).
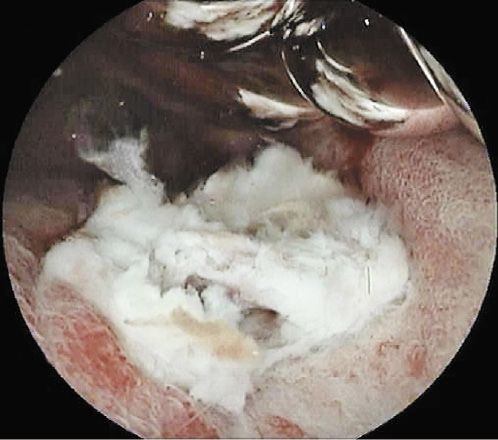
Fig. 3: Ulcer of 10 mm, located at the site of previous APC therapy, on the anterior circumference of the low rectum.
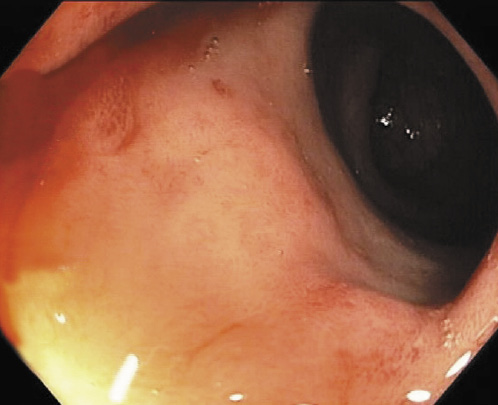
The patient resumed topical therapy with sucralfate enemas (2 g twice daily) and began mesalazine suppositories (1 g daily). As no clinical or endoscopic changes were observed after 8 weeks of topical therapy, the patient was submitted to HBO therapy, having performed 50 sessions over a period of 10 weeks (100 min per session, 5 sessions per week). The rectal ulcer completely healed, but significant improvement of rectal bleeding and radiation proctitis was not observed (Fig. 4, 5). It was decided to maintain therapy with sucralfate enemas. At 6 months, the patient was asymptomatic without anemia.
Discussion
Rectal ulcers are a common complication after APC treatment, being seen in approximately 50% of cases that underwent this endoscopic therapy [4, 6]. The development of rectal ulcers after APC is thought to be an effect of thermal injury to a damaged tissue with poorer healing. There are multiple factors associated with a risk of ulceration such as the method of application, the time interval between treatment sessions, and the flow rate of the argon [4]. However, there is no consensus regarding the optimal APC settings [7]. In a recent systematic review, Peng et al. [7] reported that the electric power setting ranged from 25 to 80 W (median 50 W), with an argon flow rate from 0.6 to 3.0 L/min (median 1.5 L/min) in several studies.
Sato et al. [8] showed that a power of 40 W with 1.2 L/min gas flow and a coagulation time of 2 s was associated with an effectively treated submucosal telangiectasia without affecting the deeper underlying muscle layer. Canard et al. [9] reported that almost all complications occurred at power settings above 45 W. Gheorge et al. [10] concluded that there was no statistical significance concerning efficacy and side effects of APC treatment between the 60 and 50 W power setting. However, rectal stenosis was observed with higher power settings.
In this case, the endoscopy performed after failure of medical treatment confirmed the persistent active hemorrhagic radiation proctitis without initial ulcerative lesions, which led us to perform APC therapy. The presence of a rectal ulcer after APC allowed to assume it as a complication of the procedure. The settings seemed appropriate, although the time of coagulation had not been noted, which may be one of the presumed causes for the development of the ulcer after one session of APC. After no clinical and endoscopic improvement with medical treatment for the APC-induced ulcer, we decided to perform HBO therapy. HBO therapy has been described as an alternative option for patients with severe radiation chronic proctitis [1, 11, 12].
In a single randomized controlled trial, Clarke et al. [13] found significant improvement of the healing responses in patients with refractory radiation proctitis. In a systematic review, Feldmeier et al. [14] reported that most articles showed a positive result for the treatment of chronic radiation proctitis, and the authors suggested HBO therapy as an alternative therapy for cases who need more invasive interventions. Despite the efficacy of HBO therapy in trials [12-14], the evidence is lacking, and more studies are necessary.
HBO therapy also has a role in radiation-induced rectal ulcers. Recently, Yoshimizu et al. [5] showed complete ulcer resolution among 5 patients with radiation-induced rectal ulcers. This report is limited by the small number of cases, but HBO therapy was effective in all cases.
In spite of the efficacy of HBO therapy in severe chronic proctitis and radiation-induced rectal ulcers, no clinical report has ever been published on using HBO therapy for ulcers after APC. This may be due to ulcers being usually clinically silent and self-limiting, with no need for treatment.
In this case, HBO therapy was an effective treatment option, and the patient had complete healing of the ulcerative lesions.