Introduction
Coronavirus disease 2019 (COVID-19) is a public health emergency caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) virus [1] that was first detected in Wuhan, China, in December 2019 and quickly spread to different countries, being classified as a pandemic by the World Health Organization in March 2020.
In Portugal the first cases were confirmed on March 3 and after that the number of infected people increased steadily, leading to the declaration of a state of emergency on March 18 and a consecutive lockdown of society until May 2.
COVID-19 has affected clinical practice in several ways and disrupted health care delivery systems around the world, including gastroenterology care and gastroenterology training. A Harvard study showed a 60% decline in the number of visits to ambulatory practices since early April 2020 [2]. To prevent the transmission of COVID-19 within endoscopy units, infection control measures were and are being established. These measures are intended to reduce the risk of spread of infection from possible COVID-19 patients, reduce the risk of cross-infection, and preserve the use of personal protective equipment [1]. Resorting to telemedicine for patient management, restricting nonessential procedures, and following strict protective strategies seem to be the key to help sail through these difficult times [3]. However, despite the benefits in terms of control of the pandemic, the prolonged suspension of everyday gastrointestinal practice will result in many gastrointestinal conditions that were once allowed to wait now requiring more urgent attention.
In this line of thought, the authors consider it is essential to investigate how the pandemic has affected Portuguese hospitals. Thus, this study aimed to assess the impact of COVID-19 in gastroenterology departments across Portugal and the strategies developed to overcome these challenges.
Materials and Methods
This is a cross-sectional study based on an online survey. A detailed questionnaire concerning different aspects of gastroenterology department activity was developed. The questions regarded numerous areas, i.e., staff planning, endoscopy unit, outpatient clinic, gastroenterology ward, and fellows in training. Two different periods were assessed, i.e., the first peak (during the emergency state) and the recovery period (from May to September 2020). The online survey, using the Google Forms® platform, was sent via e-mail to the heads of gastroenterology departments of Portuguese District Hospitals (n = 26). The answers were collected during 2 months (September and October). A reminder was sent via e-mail during the month of October. Those who had not responded by October 31, 2020, were considered nonresponders.
The Portuguese District Hospital Gastroenterology Departments consist of medium-sized to large facilities, secondary or tertiary centers, with a variable staff size. They all perform urgent and elective endoscopic procedures and outpatient consultations, as well as inpatient activity. Several departments provide gastroenterology training, with different numbers of fellows.
Results
During the study period, a total of 21 heads of gastroenterology departments filled out the questionnaire, which represents an 80.8% response rate. There were 4 hospitals from the northern region of Portugal, 8 from the center, 5 from the Lisbon metropolitan area, 1 from the south, and 3 from Madeira and Azores. These departments had a median of 6 (IQR = 4) senior gastroenterologists and 13 had fellows in training (median 3 fellows/department, IQR = 1.75). All of the participating hospitals had patients hospitalized with COVID-19.
First Peak
COVID-19 in Healthcare Workers
A total of 28.6% (n = 6) of the responders reported that healthcare professionals from their unit were infected with COVID-19, with the nursing staff being the most affected (n = 5), followed by healthcare assistants (n = 3) and finally medical doctors (n = 1). Most units had only 1 infected individual, but one department had 4 and another had 7 infected healthcare professionals.
General Planning
The pandemic had a significant impact on almost all gastroenterology departments. In terms of organization of the work schedule, 86% created rotating teams with different schedules and 14% maintained the usual schedule but defined strictly separate work places. In 66.7% (n = 14) of the departments it was necessary to deploy members of the department to another non-gastroenterology-related activity. The most frequently deployed members were fellows (n = 9), and they were deployed to the COVID-19 ward (n = 9) or the general emergency department (n = 9). Regarding telework, in 9 hospitals doctors already had remote access from their home before the pandemic and 7 were provided access during this period. The most frequent activities performed from home were medical appointments and meetings.
Endoscopy Unit
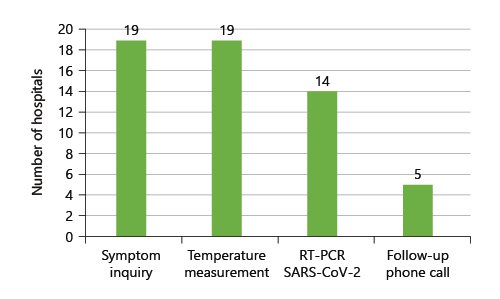
The location of the endoscopy unit had to be changed in 5 (23.8%) hospitals. Only 19.0% (n = 4) of the departments have negative pressure rooms, but in 58.9% (n = 10) of the remaining departments a room with appropriate conditions for performing procedures in high risk patients was provided. Planned endoscopy shifts had to be cancelled in 76.2% (n = 16) of the hospitals, mostly due to service rearrangement (n = 9) and shortness of staff (n = 4). In fact, during the emergency state, 47.6% (n = 10) of the hospitals only performed urgent/emergent endoscopic procedures, which was in keeping with national guidelines. Of the 15 hospitals enrolled in a colorectal cancer screening program, only 1 (6.7%) did not suspend it. The reduction in planned and urgent endoscopic activity is depicted in Figures 1 and 2.
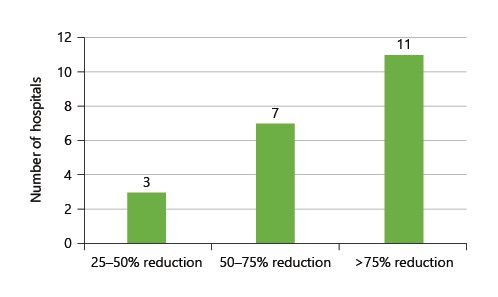
Fig. 1: Reduction of planned endoscopy productivity in the state of emergency compared to the prepandemic period.
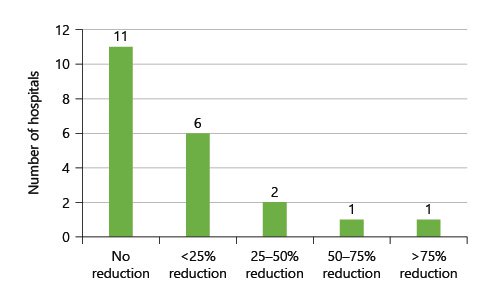
Fig. 2: Reduction of urgent endoscopy productivity in the state of emergency compared to the prepandemic period.
Concerning preendoscopic screening of COVID-19, the most frequent measures were symptom inquiry and temperature measurement, as can be seen in Figure 3. The pandemic also took a toll on anesthesiology collaborations, as 9 (42.9%) departments failed to keep endoscopy shifts with anesthesiologist sedation. Finally, 4 responders confirmed that there was a shortage/rationing of personal protective equipment in their department.
Outpatient Clinic and Gastroenterology Ward
The reduction in medical appointments was rather variable (Fig. 4). Face-to-face consultations took place in 71.4% (n = 15) of the hospitals, mostly in specific situations, such as first appointments. On the other hand, all of the hospitals performed remote consultations, i.e., 3 via video calls and 10 via phone calls from home.
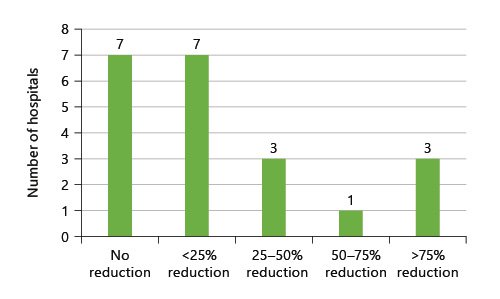
Fig. 4: Reduction of outpatient consultations during the state of emergency compared to the prepandemic period.
In terms of outpatient treatments, the location of the day hospital had to be changed in 38.1% (n = 8) of the hospitals. However, planned administration of biological therapy for inflammatory bowel disease was postponed or canceled in only 3 hospitals and large volume paracentesis for refractory ascites in only 1.
Finally, due to hospital reorganization, 6 departments saw their gastroenterology ward reduced while in 1 it was increased and in 5 its location had to be changed.
Fellows in Training
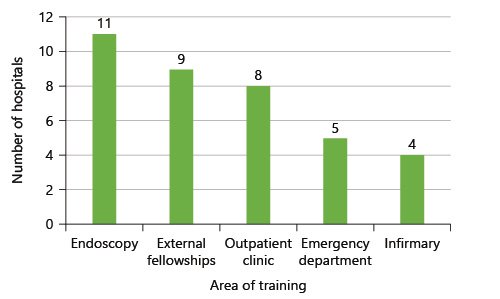
Of the 13 hospitals that had fellows in training, the majority of the responders (n = 11) considered the training of their fellows to have been significantly altered, with only 1 saying it had been mildly altered and 1 replying that there had been no impact on gastroenterology training. Figure 5 shows the different areas in which the heads of gastroenterology departments felt their fellows had been affected. In 38.5% (n = 5) of the departments the need to ration personal protective equipment led to the suspension of endoscopic training.
Recovery Period
Staff Planning
Concerning the recovery period, at the time of answering the survey, 14.3% (n = 3) of the hospitals did not have the complete medical staff back in service, 38.1% (n = 8) kept working in rotating teams in different schedules, and 28.6% (n = 6) had some kind of remote activity. Healthcare professionals were screened for COVID-19 in 57.1% (n = 12) of the hospitals, mostly by temperature measurement and symptom screening.
Endoscopy Unit
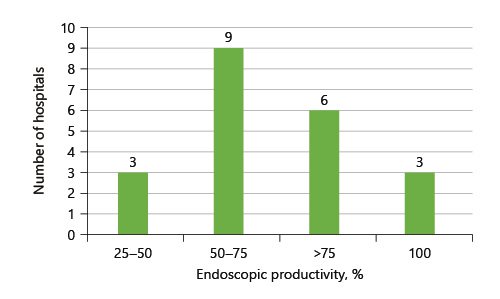
The overall endoscopic productivity in comparison to the period before the pandemic is presented in Figure 6; it was under 75% in more than half the hospitals (n = 12). In general, nonurgent/nonemergent procedures (95.2%) and endoscopic shifts with anesthesiologist sedation (100%) were resumed. The colorectal cancer screening program was restarted in 14 (93.3%) hospitals. In 6 hospitals a plan for overtime endoscopy work was developed in order to reduce the waiting list. The measures of preendoscopic screening remained largely the same. It is important to stress that 81% (n = 17) of the responders confirmed that they had postponed procedures at patients’ request for “fear of getting infected.”
Outpatient Clinic and Gastroenterology Ward
On the whole, medical appointments were resumed, with 19 (90.5%) hospitals achieving 75-100% of the productivity from before the pandemic. Remote consultations were maintained in 17 (81%) hospitals and ranged from < 25 to > 75% of all consultations. These hospitals were planning to keep some kind of remote consultation in the near future.
Regarding inpatients, only 1 hospital had not resumed normal activity. Of those who changed location, only 1 (12.5%) had returned to the original place. Likewise, regarding the day hospital, most (85.7%) had returned to >75% normal productivity, even though only 3 (37.5%) had returned to the usual location.
Fellows in Training
There were only 12 responses to this section from the 13 departments that had fellows. Most areas of gastroenterology training were restarted (outpatient clinic, 91.7%; endoscopy, 91.7%; inpatient care, 100%; and emergency unit, 100%). However, external fellowships, seeking to further expand the training of a specific area in dedicated centers, were severely compromised, since only 33.3% had been able to resume/reschedule.
Discussion/Conclusion
This study provides a detailed picture of the impact and consequences of the first wave of the COVID-19 pandemic across Portuguese hospitals.
In the beginning, the pandemic took the whole world by surprise, and the health services were no exception. In one of the earliest reports from Wuhan, around 29% of positive cases were healthcare workers [4]. Therefore, the frequency of infected professionals in this study is not surprising, as it has been described that healthcare workers have a 3-fold risk of being infected or hospitalized with COVID-19 in comparison to the general population [5, 6].
Gastroenterologists are at an increased risk for COVID-19 considering the potential of airborne transmission in upper gastrointestinal endoscopy. In fact, endoscopic practice has suffered tremendously, especially in the most severely hit areas. Reports from New York mention an 80-90% procedural volume reduction [7]. In addition to the health hazard, human and logistics resources reallocation in the midst of the pandemic led to this endoscopic “lockdown.” Indeed, both international and national recommendations [8, 9] advised postponement of elective, nonurgent procedures in the beginning of the pandemic due to a high risk of infection for both patients and healthcare professionals. Consequently, almost half of the study’s responders only performed emergent/urgent endoscopies during the emergency state. These necessary restrictions imposed by the new coronavirus are expected to have dire consequences. The reduction in endoscopically detected cancers was reported to be around 58% [10]. Moreover, in a predictive model to estimate the impact of delayed diagnosis on cancer survival, a 15% increase in the 5-year mortality rate was calculated for colorectal cancer and a 6% increase was found for esophageal cancer [11]. Analysis of the recovery period revealed that the majority of hospitals were yet able to achieve a normal procedure volume. On the other hand, almost all of the centers participating in a colorectal cancer screening program had resumed this activity. This delay is likewise expected to have consequences, as it has been determined that performing colonoscopy more than 6 months after a fecal immunochemical test is associated with an increased risk of colorectal cancer diagnosis and in a more advanced stage [12]. Finally, it is important to emphasize that a gastroenterologist was infected only in 1 hospital. This could indicate that endoscopic activity is safe when all of the necessary precautions are taken.
Although it is recommended to screen patients for symptoms and high-risk contacts before endoscopy [13], this was not performed in all hospitals. Remarkably, the large majority of responders confirmed that we are limited not only by endoscopy constraints but also by patients’ concerns, since requests to postpone procedures out of fear are a reality. Even though the risk of getting infected is not zero, all of the efforts put into planning and preventive strategies will drive it down to the very minimum.
Telehealth is defined as the provision of healthcare remotely by means of a variety of telecommunication tools, including telephones, smartphones, and mobile wireless devices, with or without a video connection [14]. Since the start of the pandemic, we have witnessed a remarkable increase in this model of care [15]. It proved to be a valuable tool to keep healthcare providers in contact with their patients while avoiding the risk of infection. Recent studies assessing patients’ perspectives have reported high acceptability and satisfaction rates for this model [16, 17]. However, it might not be appropriate for certain patients and specific situations, which require individual adaptations. Not all elderly patients will adjust to this approach due to sensory or cognitive impediments [18], and remote consultation cannot be an option when physical examination or direct patient contact is required. Thus, 71% of hospitals maintained some face-to-face consultations even in the emergency state. Nevertheless, there is a general feeling, which is mirrored in our study, that telemedicine will persist in the future and have an important role in gastrointestinal practice [19].
Our study confirms the important impact of CO VID-19 in gastroenterology training, i.e., endoscopic activity seems to have been widely affected in the beginning during the emergency state. Fortunately, it has been resumed, even though necessary measures to ensure safety conditions, such as different patient pathways and increased disinfection between patients, will surely reduce the usual procedure volume and prevent the full normalization of endoscopic training. There is general concern regarding gastroenterology training around the world. In a large international survey, comprising more than 700 trainees, 93.8% of respondents reported a reduction in endoscopy case volume [20]. In a US study, 64% of fellows felt that endoscopic restrictions will impact endoscopic skills at the end of training [21]. Alas, external fellowships at different institutions, which are a much expected and valuable experience, were enduringly affected by the pandemic. Lastly, praise is due to the gastroenterology fellows who, as stated in our paper, were frequently deployed to the front line, putting aside their training to contribute to dealing with the public health threat.
This study has a few limitations. Firstly, only district hospitals were surveyed, excluding larger hospitals from Lisbon, Porto, or Coimbra, which may have had different experiences due to their size and characteristics. Nonetheless, the majority of national hospitals and the majority of gastroenterologists is represented in the study sample. Additionally, only the answers of the department head were considered, and these may be different from individual perspectives. On the other hand, the former may constitute a more comprehensive view, as this is the person who oversees all of the activity.
In conclusion, the current pandemic significantly impaired gastroenterology practice and it will take time to return to normal. With the numbers of patients infected with COVID-19 are globally increasing, it is important to understand how the gastroenterology world dealt with the first impact of COVID-19 and what strategies were implemented to face the continuously changing knowledge of this disease in order to better prepare for the waves that might follow.