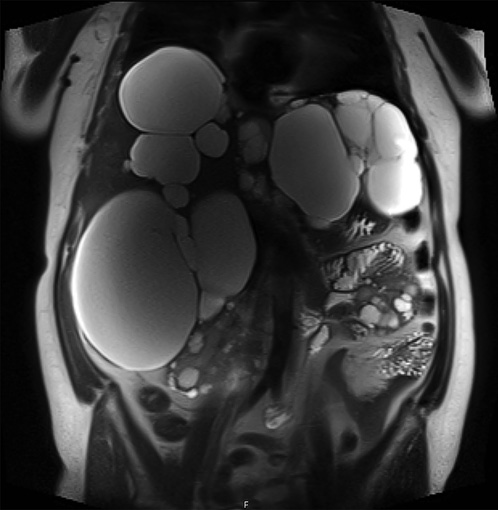
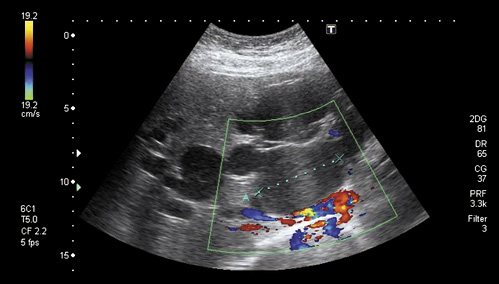
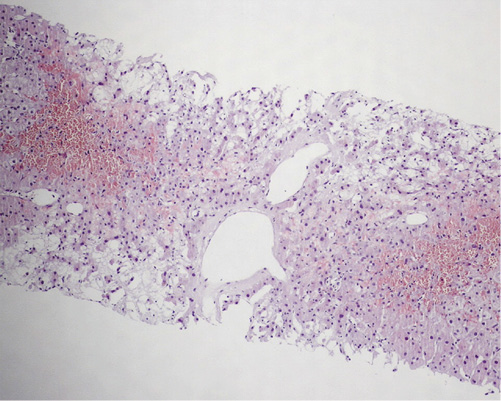
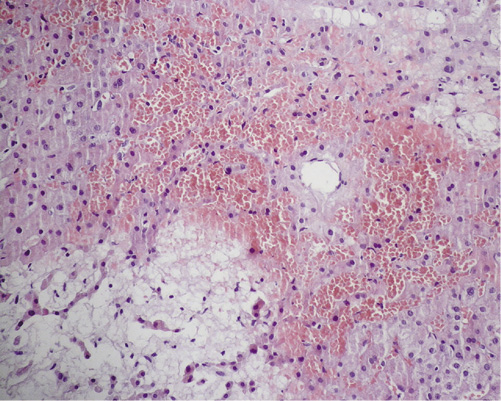
A 52-year-old female with autosomal dominant polycystic kidney disease (ADPKD) associated with polycystic liver disease (PLD) was referred to the gastroenterology clinic due to abnormal liver function tests. Laboratory testing demonstrated increased γ-glutamyltransferase (1,231 vs. normal <40 IU/L) and alkaline phosphatase (218 vs. normal <120 IU/L) levels. The patient was asymptomatic, and there were no clinical manifestations of portal hypertension. The etiological study for liver disease (including viral serologies, autoimmunity, iron kinetics, and ceruloplasmin) was negative. Abdominal magnetic resonance imaging (MRI) showed multiple hepatic cysts (the largest with a 13-cm diameter) (Fig. 1). Abdominal ultrasound with Doppler imaging showed a normal patency of the portal and hepatic veins (Fig. 2). A parenchymal liver biopsy showed marked centrilobular congestion with blood-filled cavities that resembled hepatic peliosis and was associated with findings of mild portal and intralobular inflammation (Fig. 3, 4).
After the diagnostic workup, we concluded that the patient had hepatic venous outflow obstruction secondary to cystic vascular compression. While the liver architecture is affected by PLD, the synthetic function of the polycystic liver remains intact until very late in the course of the disease [1, 2]. Histological features of this functional disease include centrizonal congestion, necrosis, and hemorrhage. Large regenerative nodules, obstructive portal venopathy, and fibrosis/cirrhosis may also be found [3].
It is important to note that in the classical forms of peliosis hepatis, the lesions are randomly distributed in the liver parenchyma. However, in the case of vascular outflow obstruction, the sinusoidal dilation is more evident in the centrilobular area (zone 3) [4].
This case highlights a rare vascular liver disease related to a genetic condition that wouldn’t usually have a significant impact on liver function. Early diagnosis may be helpful, allowing for a strategic cyst intervention that can avoid the consequences of portal hypertension.