Benign strictures of the GI tract can pose a therapeutic challenge. Even though dilation, corticosteroid injection or incisional therapy are among the most used strategies, metal stent placement may be an option in refractory strictures, especially in long strictures (1). However, conventional stents migrate in about 30-40% of the cases, and even using preventive strategies (e.g., over-the-scope clips or endoscopic suture) migration rates of 15% were described (2). Lumen-apposing, fully covered, self-expanding metal stents (LAMS), used to drain pancreatic collections, with its flanges designed to minimize migration, appears to be a safe and effective alternative for the treatment of benign stenosis with less than 10 mm in length (2, 3). In our review of the literature, there is only one systematic review and meta-analysis with 192 patients comparing migration rates, and reported a statistically significant lower migration rate of LAMS compared to covered metal stents (13.7 vs. 31.5%, p < 0.0001) and a clinical success after stent removal of 78.8% for LAMS and 48.4% for SEMS (4).
We present a series of three cases in which LAMS were used in short-segment benign strictures refractory to various attempts of balloon endoscopic dilation.
A 77-year-old man with a history of duodenal ulcer, with a punctiform peptic stenosis at the bulbar apex (Fig. 1); a 62-year-old man, with a previous history of segmental colectomy for the treatment of complicated acute diverticulitis (Hinchey III) with stenosis in the colorectal anastomosis detected in follow-up (Fig. 2); a 64-year-old man with a previous history of sigmoid adenocarcinoma, who underwent sigmoidectomy, developing a colorectal anastomosis stenosis in the follow-up, with no evidence of tumor recurrence (Fig. 3). The patients underwent 4-6 balloon dilation sessions, with intervals ranging from 2 to 3 weeks between sessions, with no clinical success.
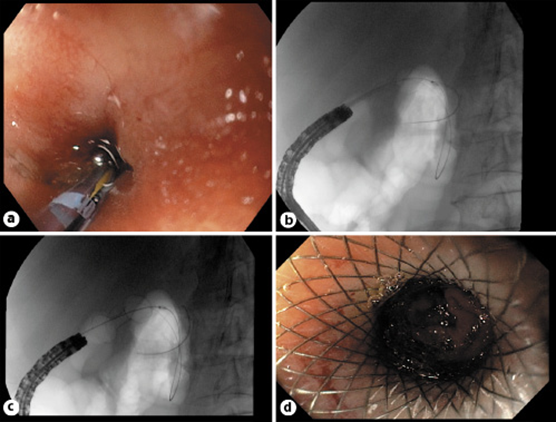
Fig. 1: Duodenal peptic stricture. a Endoscopic view with guidewire passing through the stenosis. b Fluoroscopic view with LAMS distal flange opened. c Fluoroscopic view with LAMS fully opened. d Final result with LAMS positioned in the stenosis allowing view of the duodenal lumen.
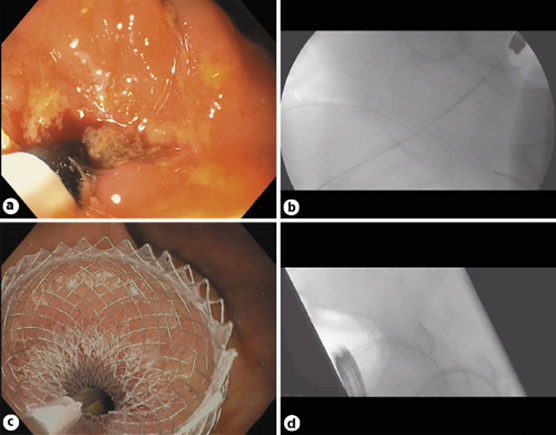
Fig. 2: Colorectal anastomosis stricture, case of sigmoid adenocarcinoma submitted to sigmoidectomy. a LAMS catheter passing through the stenosis. b Fluoroscopic view with LAMS distal flange opened. c Final result with LAMS positioned in the stenosis allowing passage of fecal content. d Fluoroscopic view with LAMS fully opened.
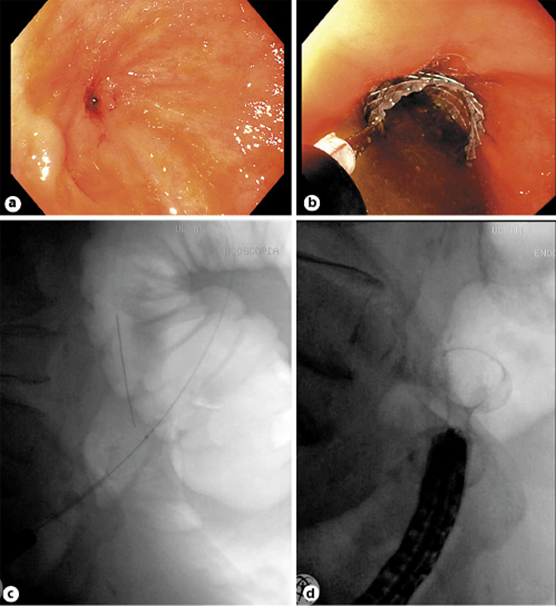
Fig. 3: Colorectal anastomosis stricture, case of Hinchey III acute diverticulitis submitted to shunt colostomy and colorectal anastomosis performed 6 months later. a Endoscopic view of the stenosis. b LAMS catheter passing through the stenosis. c Fluoroscopic view with LAMS distal flange opened. d Fluoroscopic view with LAMS fully opened.
LAMS Hot Axios (Boston Scientific®) with 15 × 10 mm were placed under endoscopic and fluoroscopic control. Technical success and rapid clinical improvement were achieved in all cases, without complications during the procedure. During a 4-month stent indwelling time, patients remain asymptomatic with no reported adverse events. LAMS removal is planned at 6 months of follow-up.
This case series highlights the safety and efficacy of LAMS in the management of such challenging GI stenosis. Despite being designed for other clinical purposes, the literature and our experience shows that LAMS design suits perfectly in this type of strictures (3).















