Introduction
Solid pseudopapillary neoplasms (SPN) are rare and represent approximately 3-4% of all cystic pancreatic tumors [1]. Symptoms, if present, are unspecific and include abdominal pain, nausea, vomiting, weight loss, and, less frequently, jaundice, a palpable mass, and pancreatitis [2]. However, at least one third of all SPN are found incidentally by imaging for other indications [2, 3]. To the best of our knowledge, upper gastrointestinal bleeding is extremely uncommon as the initial presentation of SPN. Here, we report a patient who presented with epigastric pain and melena unmasking an SPN of the pancreas.
Case Presentation
A 31-year-old woman with no prior medical history presented to our gastroenterology clinic with a 3-week history of epigastric pain associated with progressive asthenia, fatigue, and exertional dyspnea. The pain was reported as persistent and it was exacerbated by eating. One month prior, she had experienced 2 episodes of melena. A review of her systems was otherwise unremarkable, and her vital signs were stable. Upon physical examination, she was pale and nonjaundiced, with a temperature of 36.5°C and a blood pressure of 110/70 mm Hg. Her heart and respiratory rates were 92 beats/min and 14 breaths/min, respectively. Her abdomen was soft and nontender. There was no palpable mass, and bowel sounds were unremarkable.
Laboratory tests showed her hemoglobin at 8.6 g/dL and thrombocytosis (502 × 109/L), with the remainder of the complete blood count normal. Her erythrocyte sedimentation rate was 120 mm in the first hour, while her serum urea, blood sugar, electrolytes, alkaline phosphatase, bilirubin, aminotransferases, amylase, lipase, and CA 19-9 levels were within the normal ranges.
An esophagogastroduodenoscopy showed a giant ulcer in the duodenal bulb 5 cm in diameter, which presented a tightly adherent blood clot, a necrotic base, and a suspect fistulous orifice localized on the posterior wall of the duodenal bulb. In addition, a bulge on the duodenal bulb, suggestive of an extrinsic compression, was noticed (Fig. 1). There was mild diffuse oozing of blood from the lesion. The clot was removed with cold snaring, and bipolar diathermy was applied to the lesion to achieve adequate hemostasis. Biopsy samples from the ulcer edge showed inflammatory slough without fibrosis. A regimen of intravenous omeprazole (80-mg boluses), followed by a continuous infusion of 8 mg/h for 72 h, was initiated, and transfusions of 2 units of packed red blood cells were ordered.
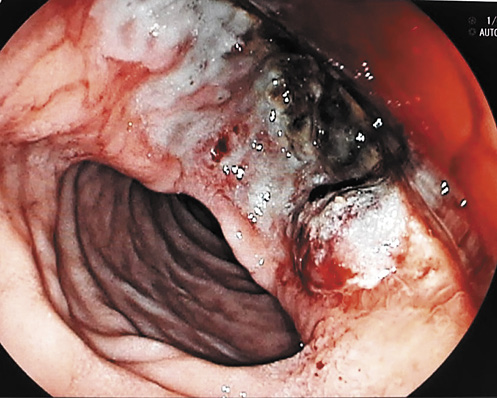
Fig. 1 Esophagogastroduodenoscopy showing a giant ulcer in the duodenal bulb 5 cm in diameter, which presented a tightly adherent blood clot and a necrotic base. There was mild diffuse oozing of blood from the lesion.
An abdominal computed tomography scan and magnetic resonance imaging showed a mixed solid and cystic lesion in the head of the pancreas approximately 12 × 10 cm in diameter. This mass was well delimited by a capsule that presented enhancement on the arterial phase. The tumor was in direct proximity to the duodenum and contained an air cavity within it that was filled by oral contrast, which was compatible with a fistulous tract (Fig. 2, 3). There was no dilation of the bile or pancreatic ducts on the magnetic resonance cholangiopancreatography.

Fig. 2 Computed tomography scan displaying a mixed solid and cystic lesion in the head of the pancreas approximately 12 × 10 cm in diameter. The tumor was in direct proximity to the duodenum and contained an air cavity within it that was filled by oral contrast, which was compatible with a fistulous tract (arrows).

Fig. 3 Abdominal magnetic resonance image showing a mixed solid and cystic well-defined lesion in the head of the pancreas. This mass was well delimited by an enhancing thick fibrous capsule (arrows).
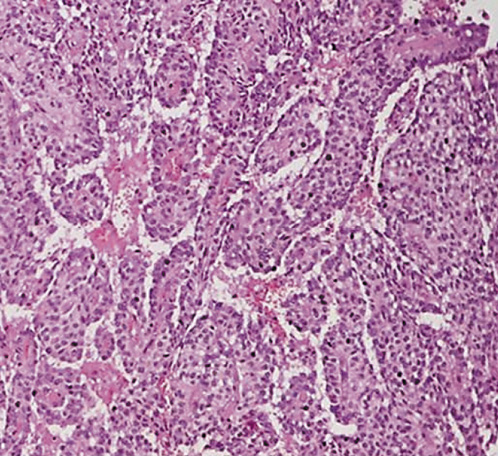
The patient successfully underwent pancreaticoduodenectomy. The histopathology of the surgical specimen revealed a tumor presenting a central ulceration, with hemorrhagic and necrotic areas mixed with solid areas extending to the duodenum and causing mucosal ulceration and fistulization to the duodenum (Fig. 4). None of the 7 lymph nodes evaluated were positive for malignancy. Microscopic analysis revealed sheets of uniform polygonal cells with pseudopapillary features (Fig. 5), with no margin involvement or perineural and angiolymphatic invasion. Immunohistochemistry was reactive for β-catenin, α1-antitrypsin, CD10, and Ki-67, which was consistent with an SPN of the pancreas.
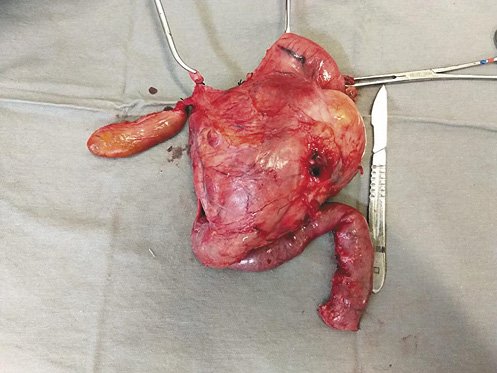
Fig. 4 Surgical specimen exhibiting a well-encapsulated tumor presenting a large central ulceration.
Discussion and Conclusion
SPN are rare pancreatic cystic neoplasms that occur most frequently in the second and third decades of life, and they predominantly (90%) affect young women. The most common clinical presentation includes incidental findings, abdominal pain, or mass effects [1, 2]. The typical imaging characteristic is a mass composed of both cystic and solid components surrounded by a well-defined capsule without involvement of the main pancreatic duct [3, 4]. However, the radiologic appearance of an SPN can also have a completely cystic or purely solid appearance; thus, it can be misdiagnosed as pancreatic ductal adenocarcinoma, pancreatic neuroendocrine tumors, or undefined cystic tumors of the pancreas [3].
Upper gastrointestinal bleeding is extremely unusual as the first presentation of an SPN [2]. In our patient, the tumor invaded the adjacent duodenum and caused a giant ulcer with gastrointestinal hemorrhage. SPN present a low malignancy potential and often cause few symptoms, with abdominal pain being the most common [1]. Notably, SPN may be incidentally found by imaging performed for nonpancreatic indications in up to one third of cases [2]. Most patients have localized disease with benign behavior; however, up to 10% of tumors have the potential for local invasion and metastases [2, 4]. Unfortunately, there are no clear factors for predicting poor outcomes.
In contrast to other pancreatic cystic neoplasms, for which periodic surveillance might be considered, the primary treatment for SPN is surgical resection at the time of diagnosis. Unlike pancreatic adenocarcinoma, the reported 5-year survival rate is over 98% after pancreatectomy [4]. Patients with a surgically resected SPN should have yearly surveillance via imaging for at least 5 years, although recurrence is uncommon [2, 4].
The patient in this case remained asymptomatic with no disease recurrence at her 18-month follow-up. Clinicians must be aware that the evaluation of patients presenting with upper gastrointestinal bleeding due to a giant duodenal ulcer and an extrinsic mass effect noted on the duodenum should include cross-sectional images of the abdomen. In this case, the finding of a large well-encapsulated pancreatic solid and cystic mass on abdominal imaging was suggestive of a pancreatic neoplasm diagnosis, including an SPN.
In this setting, surgical resection must be performed, and an excellent prognosis with minimal recurrence after resection may be expected.