We report a case of a 72-year-old female referred to a gastroenterology consultation for a finding of main pancreatic duct (MPD) dilation. The patient was a nonsmoker and had a mean daily alcohol intake of 5 g/day. Her medical history was positive for several episodes of pancreatitis 15 years previously, with biliary lithiasis, for which she underwent laparoscopic cholecystectomy. Subsequently, she had 2 other episodes of pancreatitis, including an infected pancreatic fluid collection (PFC), that underwent conventional endoscopy-guided transgastric drainage at another institution. The patient remained asymptomatic for 14 years.
A computed tomography (CT) scan and magnetic resonance cholangiopancreatography (MRCP) revealed irregularity and dilation of the MPD (8 mm in the tail and 26 mm in the body) and a communication with the gastric antrum, with no communication with the cephalic segment or ampulla of Vater. Blood tests were normal, including CEA and CA19.9 levels.
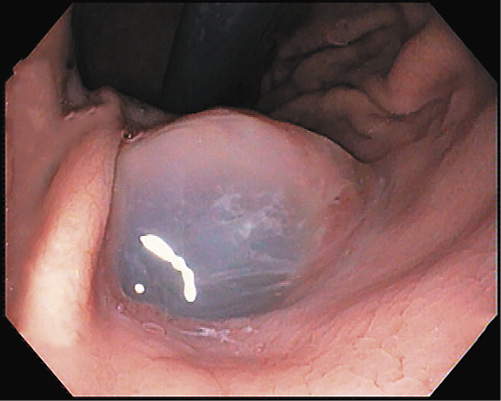
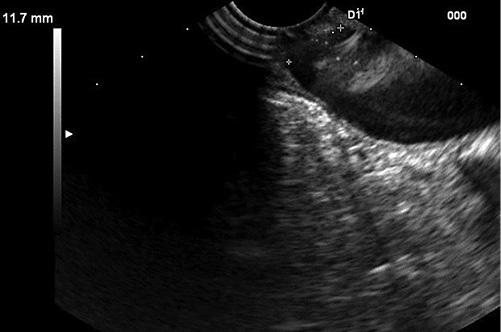
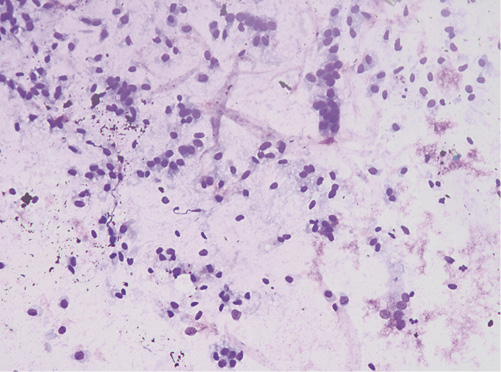
A presumptive diagnosis of disconnected MPD with a gastric fistula due to previous cystic drainage was made, but endoscopic ultrasound (EUS) was performed to exclude a main-duct intraductal papillary mucinous neoplasm (MD-IPMN). Endoscopically, a fistulous orifice 10 mm wide in the gastric antrum was apparent (Fig. 1), with a gelatinous, high-viscosity content which could not be removed despite vigorous lavage. A gastroscope was used to intubate the fistulous tract, but progression was not possible due to the viscous content. The EUS showed a globally dilated MPD (40 mm in the body) with a loss of interface with the gastric wall in the isthmus, 10 mm in diameter (Fig. 2). Fine-needle aspiration (FNA) of the MPD with a 19-gauge needle was performed, revealing a very thick mucinous content. Cytologic analysis confirmed high-grade IPMN, and the patient was referred to surgery (Fig. 3).
Although IPMN can spontaneously fistulize to adjacent organs [1, 2], in this patient, it most likely resulted from a prior drainage procedure. This case underlines the importance of a correct workup prior to endoscopic transmural drainage of PFCs to safely exclude cyst neoplasm, especially in the setting of repeated episodes of pancreatitis. Although the best approach to IPMN fistulization is yet to be defined, a MD-IPMN is a high-risk condition and should be referred to surgery [3].