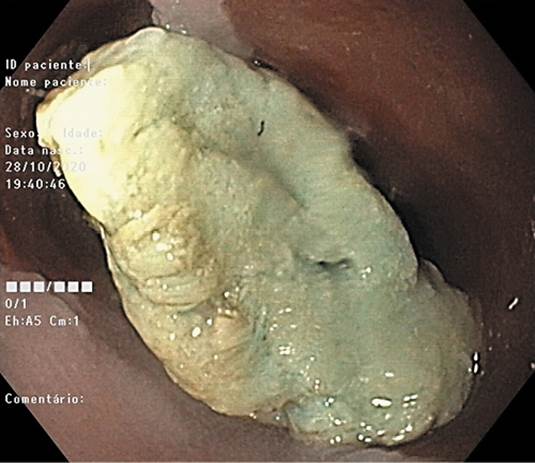
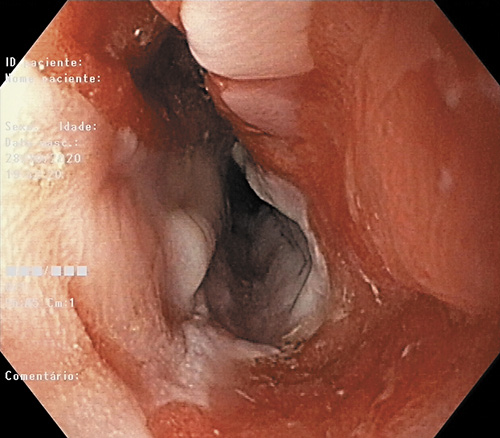
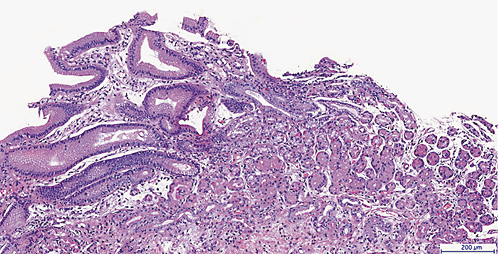
A 22-year-old healthy male was referred to the Endoscopy Unit due to food impaction. He was having difficulty swallowing solid food for the last 2 years. Esophagogastroduodenoscopy (EGD) revealed impacted meat in the cervical esophagus at 18 cm from the incisors, which was removed with a Roth net (Fig. 1). After endoscopic resolution, EGD revealed an almost circular and columnar inlet patch between 17 and 19 cm from the incisors involving more than 75% of the esophageal circumference. The lower margin of the inlet had mucosal injury and a ring stricture allowing passage for the endoscope with some difficulty (Fig. 2). The biopsies of the inlet showed gastric columnar mucosa with fundic type glands (Fig. 3), and biopsies of the remaining esophageal mucosa were unremarkable excluding eosinophilic esophagitis. After 3 months on esomeprazole 20 mg once daily, the patient had clinically improved with resolution of the ring stricture on EGD. Using narrow band imaging, the columnar inlet revealed regular circular/oval mucosa surrounded by regular vessels (Fig. 4), suggestive of oxyntic type mucosa. These findings are consistent with heterotopic gastric mucosa in the cervical esophagus with stenosis. Due to the risk of symptoms relapse with proton-pump inhibitor (PPI) withdrawal, therapeutic options, namely argon plasma coagulation (APC) and long-term PPI, were discussed with the patient. Long-term treatment with esomeprazole 20 mg with 6-12 months clinical follow-up was decided. Ablation of the inlet patch with APC or radiofrequency (RFA) was reserved for refractory symptoms.
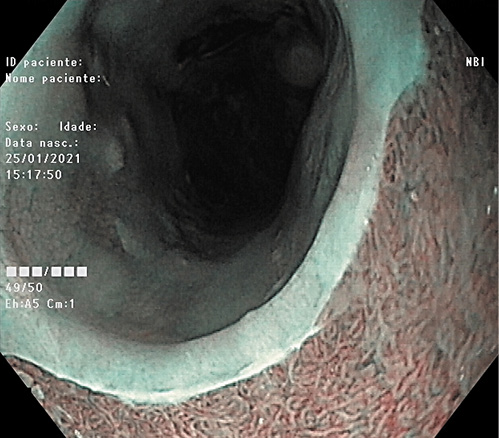
Fig. 4 Endoscopy image: circular and columnar inlet patch on the upper third of the esophagus with NBI after proton-pump inhibitor.
Heterotopic gastric mucosa is an island of ectopic gastric mucosa located in the cervical esophagus below the upper esophageal sphincter. Its prevalence has been reported to range between 0.1 and 11% in various studies [1]. Although it is accepted as being a congenital anomaly, a theory postulates that heterotopic gastric mucosa results from metaplastic transformation of the squamous epithelium due to chronic acid injury like in Barrett’s esophagus [1]. Generally, these lesions present as an asymptomatic incidental finding. However, few case reports have indicated that heterotopic gastric mucosa can produce laryngopharyngeal symptoms and complications like stenosis or malignant transformation [1, 2]. Symptomatic or complicated heterotopic gastric mucosa has to be managed either medically and/or endoscopically. While PPI is recommended as the first-line treatment since it is more widely available and safer [2], endoscopic ablation techniques are considered for symptoms unresponsive to PPI. However, APC and RFA have the potential risk of stenosis when the inlet patch occupies more than a third of the esophageal circumference [2-4]. In case of extensive ring formation, esophageal dilation with acid suppression is also an effective treatment [5]. Endoscopic mucosal resection or submucosal dissection have been used for inlet patches with malignant transformation [2].
Heterotopic gastric mucosa is generally ignored by endoscopists because it is considered benign and asymptomatic. Nevertheless, gastroenterologists should take this entity into account during dysphagia workup since it can rarely cause symptoms.