Introduction
Amyotrophic lateral sclerosis (ALS) is a neurodegenerative disease with progressive loss of the upper and lower motor neurons at the spinal or bulbar levels.
It is known that the course of this disorder is heterogeneous and the survival relies on several factors: clinical presentation (limb onset vs. bulbar onset), age of symptom onset, rate of disease progression, development of respiratory muscle weakness with consequent respiratory failure and nutritional status [1-4]. Since there is no therapy that offers a substantial clinical benefit for patients with ALS, it presents a very poor prognosis. Generally, death occurs due to respiratory failure, aspiration pneumonia, malnutrition, and dehydration [1, 5, 6].
The clinical presentation of ALS is heterogeneous but typically begins with muscle weakness, twitching, and cramping in the limbs. The disease can eventually progress to bulbar involvement, presenting with dysphagia and dysarthria [3, 7].
Nutritional assessment is a major issue to address in patients with ALS, as it has been clearly demonstrated that weight loss is an independent poor prognostic factor. Malnutrition in ALS patients can be explained in part by poor food intake, which might be due to dysphagia, severe upper-limb disability and high ventilatory dependence in patients under continuous non-invasive positive-pressure ventilation (NIV). Dysphagia develops in the majority of ALS patients during the course of the disease and, besides being inevitably associated with weight loss and malnutrition, it also entails an increased risk of respiratory infections due to aspiration, features that are associated with a poor prognosis [2, 3, 8].
Dietary changes are of paramount importance to preserve nutrition and can postpone the need for percutane-ous endoscopic gastrostomy (PEG). However, with the progression of the disease, oral feeding will become insufficient and nutrition can only be guaranteed through PEG placement [2, 8, 9].
Respiratory dysfunction is an established indicator of ALS severity and progression. Furthermore, vital capacity (VC) is a good indicator of respiratory function, and its decline is associated with a poor prognosis in ALS patients, especially when VC decreases to less than 50% of predicted. Thus, this parameter is most commonly used as a criterion for initiating ventilatory support. Respiratory complications are common in ALS, and NIV and, less frequently, invasive mechanical ventilation are used to alleviate symptoms of respiratory insufficiency. In fact, NIV significantly prolongs survival, preserves respiratory unction and improves or maintains quality of life in ALS patients [10].
The American Academy of Neurological Societies and the European Federation of Neurological Societies guidelines for the management of ALS recommend PEG placement before the occurrence of respiratory insufficiency
(FVC ≤50%) as it reduces procedure risks and improves survival and quality of life [10, 11].
PEG placement is an invasive and high-risk endoscopic procedure especially in very vulnerable patients, such as ALS patients. The procedure usually requires mild sedation and is more dangerous in patients with ventilatory impairment, particularly severe respiratory impairment, and/or at an advanced stage of the disease. In this subset of patients, NIV during the PEG procedure may be feasible [10].
Our department has a dedicated team of gastroenterologists working in cooperation with the Pneumology Department that permits the insertion of a PEG tube under NIV in these high-risk patients with ALS and severe ventilatory impairment.
The aim of this study was to evaluate the PEG tube in-sertion under NIV in patients with ALS and severe ventilatory impairment.
Methods
Study Design, Inclusion and Exclusion Criteria
A retrospective study including all consecutive PEGs under NIV placed in the Gastroenterology Department from May 2011 to January 2018 in patients with ALS under pneumology support was performed in a tertiary centre in Porto.
All patients were actively followed at the neuromuscular out-patient clinic of the Pulmonology Department, with nutritional status and swallowing status always evaluated. Severe ventilatory dysfunction was characterized by a VC below 50% of predicted.
The criteria considered to placement of PEG were: insufficient oral feeding due to dysphagia or inability of having an entire meal without the use of NIV, weight loss >10% and suspicion of aspiration pneumonia.
At the time of referral, all patients were evaluated by a pulmonologist and a specialized respiratory physiotherapist, as well as by the gastroenterologist in charge of patients who were candidates for PEG placement. The procedure was explained to the patient and the family, and all the periprocedure risks and implications to the future of the patient were considered. A patient or family in-formed consent was obtained before the procedure.
Procedure
A 12-h fasting prior to the examination was recommended to the patient and anticoagulation therapy stopped for 1 week (war-farin was substituted by enoxaparin that was stopped 24 h before the procedure).
ll patients received prophylactic antibiotic treatment with 1 g cephazolin 1 h before PEG placement.
The procedure was done with an upper endoscope (Olympus ® GIF-Q160, GIF-Q165 and GIF-Q180 models), and a PEG kit was used (PEG US Endoscopy® Pull Silicone (20-24 Fr).
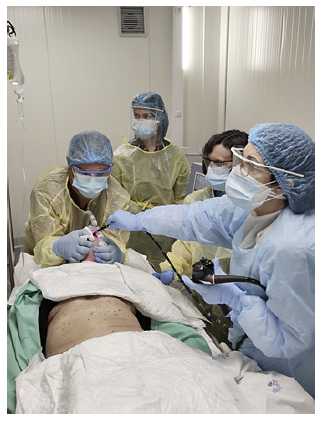
PEG placement was performed by three operators in strict collaboration: one experienced endoscopist, one gastroenterologist responsible for the percutaneous component of the procedure and a specialized respiratory physiotherapist responsible for adjusting NIV parameters whenever it was necessary. This team was also responsible for sedation and its control (with midazolam).
An upper endoscopy was performed to exclude malignancy or gastric outlet obstruction and determine the optimal site for PEG placement. After lidocaine injection, a 2-cm-deep horizontal incision was made and the PEG placed by the through pull method. This procedure was performed without general anaesthesia or profound sedation and under nasal NIV (Fig. 1) in spontaneous timed bilevel mode. When needed, a conscious sedation with midazolam was applied. Those patients who had not been using NIV, were adapted and trained in nasal NIV usage previously by the specialized respiratory physiotherapist to prepare them for the procedure. Estimated tidal volumes, airleaks through the mouth, SpO2, heart rate and respiratory rate were monitored continuously. Due to the increase in mouth air leaks during the PEG placement, home ventilator parameters were readjusted to achieve patient comfort. Low flow oxygen was only employed with NIV to obtain an SpO2 ≥92%, despite NIV optimization. If SpO2 ≤≥92% could not be reached with nasal NIV plus low flow O2 ( 2 L/min), then PEGplacement was cancelled. All patients maintained NIV with their home interface for at least 3 h after the procedure.
Data Collection
Patient data were collected from electronic medical records. Age, gender, presence of dysphagia, previous episodes of aspiration pneumonias, date of established diagnosis of ALS and time of the beginning of bulbar symptoms and presence of comorbidities (diabetes mellitus, liver disease, malignancy, AIDS, moderate to severe chronic kidney disease, heart failure, previous myocardial infarction, chronic obstructive pulmonary disease, peripheral vascular disease, previous cerebral vascular accident or transitory ischaemic accident, dementia, hemiplegia, connective tissue disease and peptic ulcer disease) were obtained, and the Charlson comorbidity index was calculated.
Data regarding the procedure such as type of PEG, need of sedation and dose of midazolam and periprocedure complications were also obtained, as well as postmortality and postprocedure complications (more than 1 month after PEG tube placement). We used our non-ALS PEG patient database to compare the rate of complications of PEG tube insertion in ALS patients.
Results
We included 59 patients, 34 females (58%) and 25 males (42%), with a mean age of 67.2 ± 10.1 years, and the median follow-up was 6 [range 2-15] months.
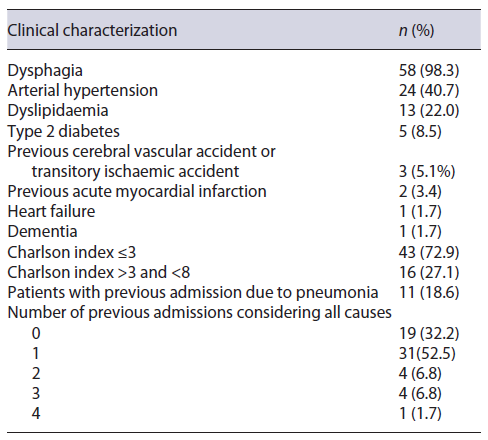
The median Charlson index was 3 [2-4], and 24 patients had arterial hypertension, 13 had dyslipidaemia, 5 patients had type 2 diabetes, 3 previous episodes of cerebral vascular accident or transitory ischaemic accident and 2 previous episodes of acute myocardial infarction.
Nine patients had suspicion of previous episodes of aspiration (15.3%), and 11 patients had previous admissions for pneumonia (10 patients 1 single episode and 1 patient with 2 admissions due to pneumonia).
The main reason for referral for PEG placement was dysphagia with associated weight loss (98.3%).
The clinical characterization is listed in Table 1. The median time for PEG tube insertion since the established diagnosis of ALS was 12 [6-25] months and 4 [2-18] months since the beginning of bulbar symptoms. The majority of the patients had placed a 20-Fr PEG tube (62.7%) and 47 needed midazolam sedation (92% up to 2 mg of midazolam). There were no immediate complications during and after the procedure (no episodes of aspiration or orotracheal intubation), need for admission or mortality. In addition, regarding minor complications, there were no episodes of apnoea/hypoventilation, aspiration pneumonia or peristomal infection in the postpro-cedure period.
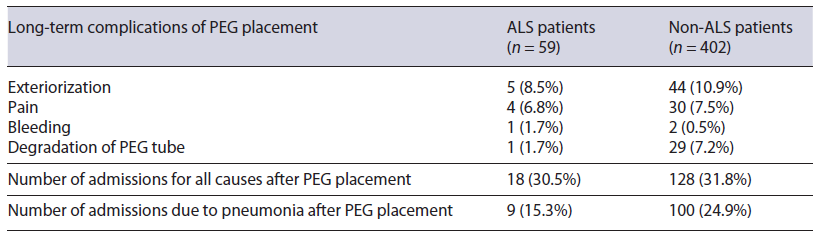
Eleven patients developed long-term complications after PEG tube placement. Six patients needed to substitute the PEG because of 5 accidental exteriorizations and 1 PEG tube degradation, 4 patients developed pain at the site of the PEG tube due to skin erythema (these cases were totally solved after topic fusidic acid use) and 1 patient had self-limited bleeding for the site of the PEG.
In the period of follow-up, there were 18 admissions after PEG placement, with 9 admissions due to pneumonia.
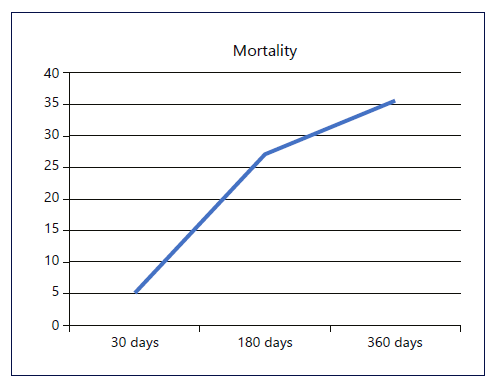
The 30-day mortality after PEG placement was 5.1%, the 180-day mortality was 27.1% and the 360-day mortality was 35.6% (Fig. 2).
Discussion
In this study, we showed that placement of PEG under NIV in ALS patients with severe ventilatory impairment through a strict cooperation between the Gastroenterology and Pneumology Departments is a safe and effective procedure. No respiratory distress or infection, or any other pulmonary complication, was observed in this cohort of patients. No death after the procedure could be imputable to PEG placement.
Malnutrition is undoubtedly one of the main prognostic factors with some studies showing a linear decline in muscle strength. In addition, severe malnutrition is associated with muscle atrophy, muscle weakness, increase in fatigue and decrease in respiratory capacity, leading to the development of depression and decreasing quality of life [1, 8, 12]. Therefore, it is essential to provide effective nutritional care to ALS patients. Several studies have evalu-ated the efficacy of gastrostomies to solve this problem and linked PEG placement to decreased morbidity and improved survival rates (mainly by decreasing pneumonia and cachexia), being a successful and safe procedure in highly disabled ALS patients with respiratory compromise and advanced neurological disease [9, 13, 14]. In our opinion, it should be noted that the proposal of this procedure should not be conditioned by the severity of the respiratory functional impairment of the patient. Otherwise, many patients would have to undergo PEG placement too early in the course of the disease and would have been unnecessarily exposed to the constraints that PEG implies. In fact, a patient with a functional and preserved deglutition and capable of autonomous breathing should not undergo PEG placement uniquely because VC is decreasing and reaching the threshold of 50% of predicted. Thus, we think that the recommendation of the American Academy of Neurology - that, for optimal management of ALS, PEG should be placed when VC is above 50% of predicted [10] - might be exaggerated and contribute to needlessly diminishing the quality of life of ALS patients. This recommendation is mainly based on the argument that it would minimize the risk of respiratory complications [10, 15, 16]. However, in a centre with an experienced and multidisciplinary team, ALS patients with severe ventilatory impairment can be addressed safely and undergo PEG placement under nasal NIV support, as we show with our results. Accordingly, an individualized approach should be undertaken to each patient, taking into account the overall condition of the patient, as well as the severity of dysphagia symptoms and the degree of malnutrition. Recently, an interesting risk-stratifying tool for the approach of PEG placement in late-stage ALS patients was proposed, considering also the NIV support during the procedure in high-risk patients [17-24].
Conscious sedation is another point of discussion in ALS patients, being carefully considered by the European guidelines, as there are only scarce data. In our study, almost 80% received conscious sedation with midazolam with simultaneous NIV and there were no changes in blood pressure, anaesthetic or respiratory complications [3, 10]. We did not find any disadvantage of conscious sedation (in the majority of cases with 2 mg of midazolam) compared with general anaesthesia with propofol, and the procedure with conscious sedation was performed without affecting technical success.
Another interesting fact is that we found fewer long-term complications of PEG placement when we compared our cohorts of PEG in our department (18.6% in ALS patients vs. 33.8% in general patients; Table 2). This difference is even higher if we look to exteriorization and degradation of PEG. This fact might be explained because ALS patients are a population that maintain their cognitive functions preserved till very advanced phases of the disease, which will lead to careful management of the PEG tube. When we also compared the number of admissions due to pneumonia during the period of follow-up, it was also reduced even with the progressive character of the disease.
The impact of PEG on survival cannot be directly extrapolated in our group of patients, since no control group without PEG placement was enrolled. However, it is difficult to evaluate the real impact of PEG on survival, since other factors such as NIV usage, bulbar muscle impairment, timing of PEG placement and patient comorbidities might have also a significant impact on mortality. Besides that, we can assume that PEG placement is mainly a symptomatic treatment, deemed to be a quality of life measure. By reducing the risk of weight loss, malnourishment and respiratory infections due to aspiration, PEG placement might have a positive impact on the survival of ALS patients. As an additional remark, in our study population, there was a high proportion of patients under NIV. It is well known that NIV improves survival in ALS patients, a fact that was also demonstrated in our analyses, since patients under continuous non-invasive ventilatory support, despite the severity of respiratory function impairment, had a tendency for a higher median survival.