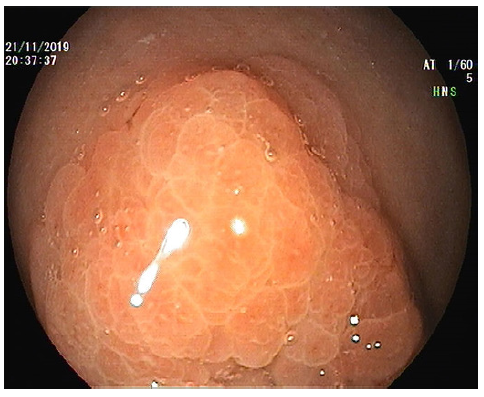
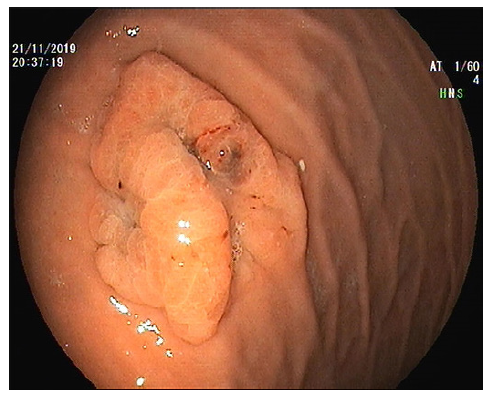
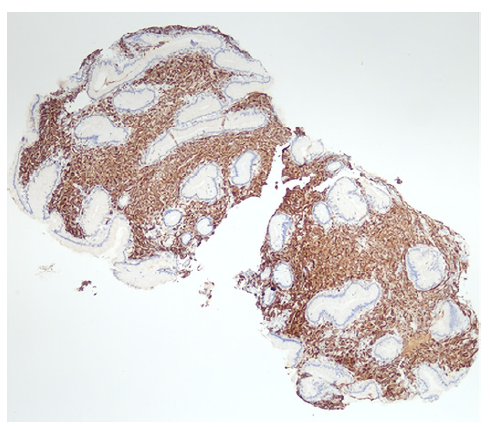
A 56-year-old woman was submitted to an upper gastrointestinal endoscopy due to a recent history of epigastric pain. Endoscopic examination revealed a 20-mm 0-IIa type lesion in the great curvature of the proximal corpus with a hyperplastic appearance and a dark coloration area in one of the edges (Fig. 1, 2). Biopsy of the lesion was suggestive of mesenchymal proliferation and some cells with moderate cytologic atypia. The patient was then referred to our Endoscopy Department to undergo endoscopic resection. Due to the previous histological result, we decided to perform an endoscopic ultra-sonography that showed thickening of the superficial layers of the mucosa. Endoscopic biopsies were repeated, and pathological evaluation revealed diffuse involvement of the lamina propria by a malignant neoplasm, composed of cells with nuclear pleomorphism and high mitotic rate, entrapping benign gastric glands. Immunohistochemistry showed diffuse positivity for melanocytic markers (PS100, SOX10 and MelanA) and negativity for cytokeratins, DOG-1 and CD45 (Fig. 3, 4). Given the clinical history of a malignant melanoma of the third left hand finger submitted to amputation 5 years before, a diagnosis of gastric metastasis of malignant melanoma was made. Thoraco-abdomino-pelvic computed tomography and PET scan showed no other metastasis. After multidisciplinary discussion, total gastrectomy was proposed to the patient given the location of the lesion (proximal corpus). During surgery, it was decided to perform an atypical gastrectomy following endoscopic tattoo. The histological specimen confirmed the diagnosis of malig-nant melanoma with free surgical margins. The patient is currently under clinical and imagiological (PET scan) surveillance.

Fig. 3 Gastric body mucosa with normal epithelial cells and a diffuse infiltration of the lamina propria by sheets of malignant neo-plastic cells. HE staining, ×40.
Malignant melanoma is a frequent source of metastases in the gastrointestinal tract [1]. The most frequent location is the small bowel followed by the colon and rectum; gastric metastases are rare [1, 2]. Metastatic disease is usually diagnosed within the first 3 years, but metastases after 15 years have also been reported [3]. Lesions mimicking submucosal or primary gastric ulcerated tumours are the most frequent presentation, although endoscopic findings are variable [2, 4].
It is important to keep in mind the different possible endoscopic appearances of metastatic lesions to avoid further delay in diagnosis and treatment. Immunohisto-chemistry is an imperative tool for making a correct diagnosis in these circumstances.