A 77-year-old woman was admitted to the hospital because of abdominal distension and vomiting. Laboratory workup showed acute kidney injury with serum creatinine of 3.5 mg/dL and potassium of 5.7 mmol/L. Intravenous hydration, antibiotics, and symptomatic medication were started. Sodium polystyrene sulfonate (SPS) 15 g twice daily was used to treat hyperkalemia. After 48 h, serum potassium decreased to 3.7 mmol/L, and creatinine to 1.8 md/dL. On day 4 of admission she developed watery diarrhea, initially managed with probiotics and dietary modification. Infectious workup was negative for Clostridioides difficile, parasites, and Cytomegalovirus.
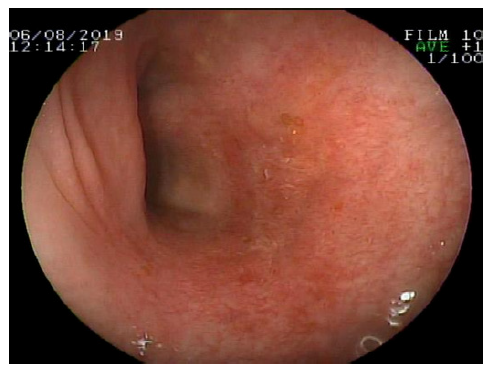
Colonoscopy revealed edema, enanthema, and erosion into the sigmoid colon (Fig. 1). Biopsy showed typical fish scale-like SPS crystals (Fig. 2). SPS administration was discontinued, and the patient’s condition progressively improved until resolution.
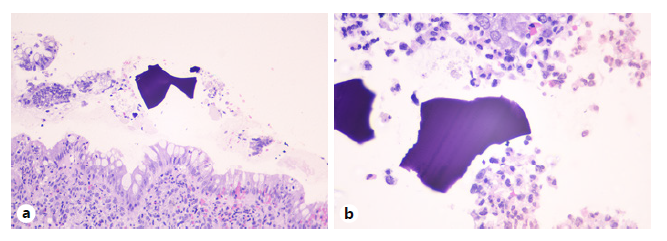
Fig. 2 Sigmoid colon, biopsy. a Mucosal injury with intraepithelial neutrophils (HE ×200). b Polystyrene crystals displaying a fish-scale appearance (HE ×600).
The use of SPS (or Kayexalate) to treat hyperkalemia dates back to the 1960s. Common side effects include constipation, bloating, nausea, and vomiting. Patients with previous kidney damage account for more than 70% of those who develop side effects, which often occur after 2 days of SPS administration. SPS-induced colitis is rarely detected by colonoscopy. Biopsy shows necrosis, ulceration, and SPS crystal deposition in more than 90% of samples. These features can distinguish SPS-induced necrosis from ischemic necrosis. A definitive diagnosis requires excluding conditions that mimic SPS-induced colitis, such as neoplasms, inflammatory bowel disease, microscopic colitis, C. difficile infection, and infectious colitis.
The first cases of SPS-associated ulceration and colonic necrosis were reported by Lillemoe et al. [1] in 1987. In 2013, a systematic review identified 58 cases of serious adverse reactions to SPS use. Colonic necrosis was the most severe complication, resulting in a mortality rate of 33% [2]. Nevertheless, a recent systematic review and meta-analysis showed that, although there was a statistically significantly increased risk for the composite outcome of severe gastrointestinal side effects based on 2 studies, there was no definite association of SPS use with intestinal necrosis [3]. In rats, SPS enema was associated with colonic necrosis and a high mortality rate [4]. Because intestinal necrosis is a life-threatening condition, caution should be exercised before prescribing SPS in patients at risk for complications [5]. Currently, there is no specific treatment for SPS-induced colitis, and medication withdrawal often results in symptom improvement.
In conclusion, SPS-induced colitis is a rare cause of diarrhea in the hospital setting. It should be suspected especially in patients with previous kidney damage who have received treatment for hyperkalemia.