Endoscopic resection of supra-anal lesions is challenging due to marked fibrosis and generous venous plexus [1]. Furthermore, abundance of sensory nerve fibres in the anal canal calls for an adequate local anaesthesia otherwise not warranted in endoscopy [2]. This is the case of a 54-year-old male patient with a 2-year history of debilitating diarrhoea including inability to work (sic!), passing up to 25 watery stools with urgency. Prior gastroenterology consultations elsewhere including previous ileocolonoscopy did not indicate the cause of diarrhoea.
Currently, the patient was scheduled for endoscopic resection of an estimated 15-mm, biopsy-confirmed mucosal prolapse polyp in the supra-anal rectum involving the dentate line. The retroflexed endoscopic visualization revealed a reddened polypoid lesion with an eroded surface, consistent with mucosal prolapse syndrome (Fig. 1a). For resection, a capfitted, antegrade endoscopic approach was chosen to first isolate the lesion from the squamous epithelium of the anal canal, which indeed was cut into in its proximal aspects after injection of an indigocarmine saline mixture without adrenaline and a local anaesthetic (Fig. 1b). To this end, limited endoscopic sub-mucosal dissection using a Dual Knife J (Olympus, Hamburg, Germany) was performed under deep sedation using propofol and midazolam to ensure wide-margin resection at the anal side with diarrhoea most likely attributable to chronic sphincter irritation (Fig. 1c; note marked fibrosis and prominent vessels). Only after progression to the more oral rectum did the submucosal space begin to open up adequately (Fig. 1d). To accelerate the procedure and with a view to the benign histology, we subsequently opted for a hybrid approach ensnaring the lesion (30-mm snare; Medwork, Höchstadt, Germany) after adequate trimming of the anal parts of the lesion (Fig. 1e). The final resection bed was without bleeding;
note the broad cauterization zone related to marked fibrosis (Fig. 1f). The postinterventional course under a 3-day ibuprofen regimen was uncomplicated without pain and/or bleeding complications. The final histology of the 30 × 20 mm specimen described a mucosal prolapse polyp with formation of an inflammatory cloacogenic polyp with a serrated architecture. Dysplasia and/or (anal) intraepithelial neoplasia was excluded.
Of note, diarrhoea ceased immediately and persistent-ly with complete normalization of stool habits, and the patient was able to resume work. An endoscopic control 12 months later revealed an unremarkable resection scar without evidence for recurrence (Fig. 1g).
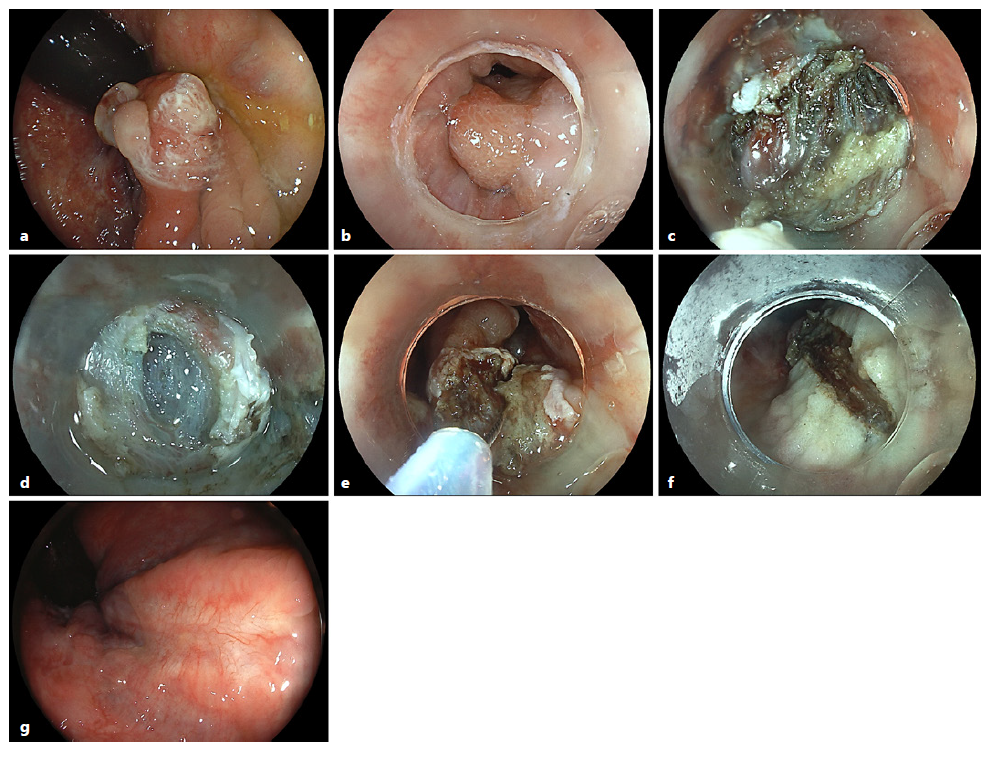
Fig. 1 a Retroflexed vision of an estimated 15-mm reddened supra-anal polypoid lesion with an eroded surface. b Capfitted, prograde representation with continuity to the squamous epithelium of the anal canal. c Limited endoscopic submucosal dissection using a Dual Knife J (Olympus) to ensure wide-margin resection at the anal side; note marked fibrosis and vessel abundance. d Only after lateral progression to the more oral rectum did the submucosal space begin to open. e After adequate trimming and isolation of the lesion from the anal canal, a hybrid approach was opted for to accelerate the procedure, involving snare resection of the lesion. f Final resection bed without bleeding; note the broad cauterization zone related to marked fibrosis. g Endoscopic control 12 months later revealing an unremarkable scar without recurrence.
Mucosal prolapse syndrome as a rare category of colorectal polyps, oftentimes presenting as polypoid supra-anal lesions, if symptomatic warranting endoscopic resection [3, 4]. Indeed, some reports have been pub-lished in which such lesions proved difficult to distinguish from malignancy [5]. Of clinical note, endoscopic resection resulted in rapid and complete normalization of stool habits in this patient with chronic debilitating diarrhoea, which has only occasionally been reported in the literature [6, 7]. Apart from endoscopic submucosal dissection in this technically demanding anatomical region, recent data suggest a similar clinical effectiveness of endoscopic mucosal resection techniques in this setting [8].














