A 41-year-old male with a history of Crohn’s disease (CD) with penetrating phenotype (A2L2B3p, Montreal Classification), who was diagnosed aged 17 years and had started treatment with infliximab monotherapy at 30 years old, had been on clinical, imagiological, and endoscopic remission for the previous 2 years. On follow-up ileocolonoscopy with the purpose of considering stopping biological treatment (per the patient’s wishes), only 2 superficial ulcers in the sigmoid colon and 3 small erosions in the terminal ileum (shown in Fig. 1) were detected. Histological examination of the ileum erosions demonstrated an infiltrate of atypical lymphoepithelial cells, CD20 positive and CD5, CD23, CD10, and cyclinD1 negative, compatible with a marginal zone B-cell lymphoma of the mucosal-associated lymphoid tissue (MALT; shown in Fig. 2). Immunoglobulin deposition was not identified in this tissue. Cervico-thoraco-abdominopelvic computed tomography and magnetic resonance bowel enterography were unremarkable. The histological specimens were analyzed by two different pathologists with expertise in hematopathology. Serum lactate dehydrogenase, β2-microglobulin, and immunoglobulin levels were normal. Hepatitis C virus antibodies and DNA of Campylobacter jejuni on ileum tissue were negative. Staging was complete as a MALT-lymphoma Galian stage A and Lugano stage I. A 6-month course of antibiotic therapy with combined metronidazole and ampicillin was proposed after consultation with Hematology. As the patient was in clinical remission and the endoscopic activity was residual, biologic therapy was suspended due to an unfavorable risk/benefit. Unfortunately, CD recurred clinically and endoscopically so vedolizumab was started after endoscopic and histologic documentation of MALT remission (1 year after diagnosis, 6 months after antibiotics). Due to a primary non-response, the patient was swapped to ustekinumab and is currently in clinical remission, with a further endoscopic evaluation at 6-9 months.
Immunoproliferative small intestinal disease (IPSID) is a subtype of MALT lymphoma, with only sporadic cases in Western countries. IPSID may result from chronic immune stimulation by either autoimmune disorders (such as CD) or infectious agents (such as C. jejuni) [1, 2]. B-symptoms are rare in this disorder, creating another barrier to the final diagnosis [3]. While there is a slightly elevated risk of lymphoma development with thiopurine/combination therapy, there is little convincing evidence to date associating anti-TNF monotherapy and lymphoma development in IBD patients and the benefits of CD control clearly out-weigh the risk of malignancy [4]. MALT lymphoma generally shows an indolent course, but non-gastric MALT lymphomas have a poorer prognosis compared to the gastric type [5]. Despite controversy, in a localized early-stage disease, IPSID could be treated with antibiotics, since it is associated with durable remissions in the majority of patients [6]. Although current evidence is still lacking, vedolizumab/ustekinumab appears to have an acceptable safety profile in this setting, while anti-TNF and thiopurines probably should not be used unless strictly necessary [7]. In conclusion, this case represents the difficulties in managing IBD patients and immunosuppressive medications, requiring constant risk/benefit analysis and careful follow-up.
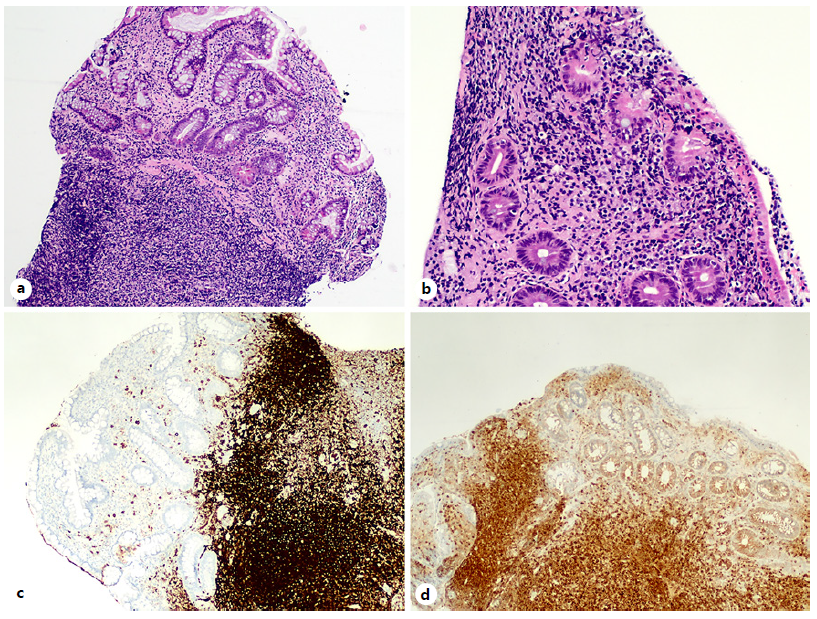
Fig. 2 Histopathological findings of small bowel biopsy. a Villous atrophy and focal decrease of mucus secretion. HE. Original magnification ×20. b Atypical and prominent lymphoplasmocytic infiltrate within the lamina propria, exhibiting a roughly nodular architecture, predominantly comprised by small lymphocytes with centrocytoid and monocytoid morphology. There were occasional immunoblasts and lymphoepithelial lesions. HE. Original magnification ×40. The small lymphocytes expressed both CD20 (c) and Bcl-2 (d).
















