Introduction
The liver allocation policy based on the Model for End-Stage Liver Disease (MELD) score, more recently with the added component of serum sodium (MELDNa), prioritizes the sicker patients for liver transplant (LT) [1]. That approach has reduced patients’ overall mortality on the LT waitlist for more than a decade [2].
The donor risk index (DRI) was developed more than a decade ago to quantify donor-related characteristics that could be associated with increased risk of 1-year graft failure [3]. DRI has offered the possibility to classify organs as high or low risk and has enabled comparisons of transplant practices with such different organs [4, 5]. However, DRI and the several similar models that have been developed afterwards have generally yielded low discriminative or predictive values for post LT outcomes [6].
Perioperative related factors have also been associated with post LT outcomes [7, 8]. However, while recipient- or donor-related factors may be known in advance to allow clinicians to better match LT recipients and donors, perioperative factors are not. Therefore, perioperative factors remain a distinct and difficult to account for component of complex rules intended to predict post LT outcomes.
Accordingly, the objectives of this study were as follows: (1) to assess the impact of DRI on post LT outcomes in a recent cohort of patients; (2) to evaluate the differential impact of recipient, donor, and perioperative factors on post LT outcomes.
Materials and Methods
This study was approved by the Central Lisbon University Hospital Center (CLUHC) ethics committee (reference number INV_185) and informed consent was waived. The study protocol and conduct abided by the principles of the Declaration of Helsinki [9]. The study reporting followed the STROBE guideline [10].
Design, Setting, and Participants
This was a single-center retrospective cohort study including all adult (≥18 years) patients who underwent LT from January 2019 to December 2019 at Curry Cabral Hospital (CCH), CLUHC. Patients who underwent living-donor LT were excluded from the final analysis (online suppl Fig. S1; for all online suppl. material, see https://www.karger.com/doi/10.1159/000524421).
Operational Definitions and Endpoints
The CCH has performed 2,257 adult LT procedures from January 1992 to December 2019. Listing criteria and peri-LT management, including immunosuppression (online suppl. Table S1), have been in accordance with specific international guidelines [1, 11]. Following LT, all patients are admitted to an intensive care unit (ICU) specialized in LT care and when deemed clinically stable transferred to a specialized ward.
The following data were collected about LT recipients: age, sex, etiology of liver disease, presence of hepatocellular carcinoma (HCC), cause of LT, LT priority, patient location prior to LT, laboratory-based MELDNa prior to LT, and sequential organ failure assessment (SOFA) score and laboratory parameters on ICU admission post LT. The following data were collected about LT procedures: retransplantation status, time of operation (hours), vena cava and biliary anastomosis surgical technique, type and number of blood components transfused, result of blood cultures, and the type of immunosuppression used for induction.
Under Portuguese law, all individuals are potential donors of organs unless they specifically opt out in a mandatory and private national registry. Donation procedures are controlled nationally by the Portuguese Institute of Blood and Transplantation.
The DRI was calculated based on the 8 donor-related components derived in the original study: age (years), height (cm), race (white, African descendent, or other), cause of death (trauma, stroke, anoxia, or other), donor following cardiac death, partial or split graft, location of organ sharing (local, regional, or national), and cold ischemia time (CIT; hours) [3]. Additionally, sex, warm ischemia time (WIT), and the type of organ preservation fluid were also retrieved for donors. According to the original study, 1-year graft survival rates varied substantially with the DRI, for example: 85.0% for a DRI of 1.0-1.1, 79.7% for a DRI of 1.4-1.5, or 75.6% for a DRI of 1.8-2.0 [3]. The balance of risk score was also computed, as previously described, for comparative analysis with the DRI [12].
The primary endpoint was graft failure at 1 year following in-dex LT as described elsewhere [3]. The secondary endpoint was index hospital length of stay (LOS).
Statistical Analysis
Continuous variables were described as median and interquartile range (IQR) and categorical variables were described as frequency (n) and proportion (%). Univariate comparisons were done using Mann-Whitney or Kruskal-Wallis tests for continuous variables or χ2 test for categorical variables. Survival was plotted using Kaplan-Meier curves. Multivariable analysis was performed using logistic or linear regression following automated multiple imputation (5 iterations) due to the level of missing data (7.8% across all values in the dataset). Clinical and statistical (p < 0.10 on univariate analysis) covariates were included, and final models were obtained following a stepwise backward selection of covariables. The significance level considered was α = 0.05 (2-tailed).
Statistical analysis was performed using IBM SPSS Statistics version 25.0 (IBM Corp., Armonk, NY, USA).
Results
Characteristics of LT Recipients
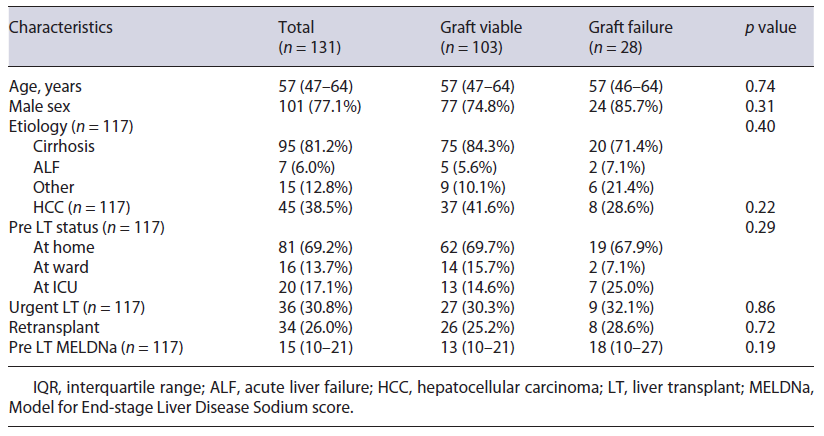
A total of 131 cadaveric donor LT procedures were performed in 116 recipients in 2019 (online suppl. Fig. S1). Recipients’ median (IQR) age was 57 (47-64) years and 101/131 (77.1%) were males. Cirrhosis (and its complications) was the underlying liver disease in 95/131 (81.2%) transplants. HCC was the cause for LT in 45 (38.5%) cases. Urgent (patient acutely decompensated in the ward or ICU pre transplant) LT was performed in 36/117 (30.8%) patients. The index LT considered was for retransplantation in 34/131 (26.0%) procedures. Median (IQR) MELDNa score pre LT was 15 (10-21). All characteristics of LT recipients are depicted in Table 1.
Table 1 Characteristics (n (%) or median (IQR)) of recipients stratified by graft survival status at 1 year post LT (n = 131)
Characteristics of LT Donors
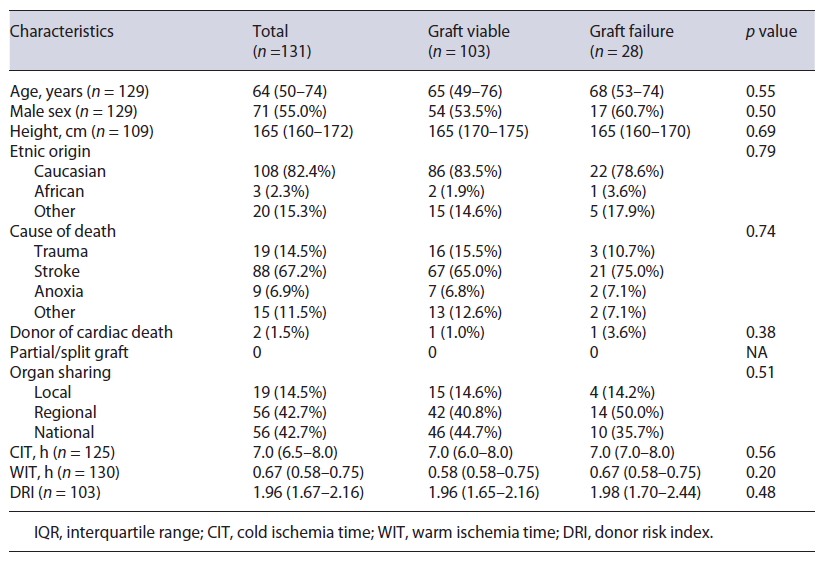
Median (IQR) age of donors was 64 (50-74) years (61/129 [47.3%] aged ≥65 years), and 71/129 (55.0%) were males. Stroke was the cause of death in 88/131 (67.2%) donors. Only 2/131 (1.5%) donors had primarily cardiac death. No partial or split grafts were used. Organs from a region outside of Lisbon were used in 56/131 (42.7%) transplants, with only one coming from outside of Portugal (Spain). Median (IQR) CIT and WIT were 7.0 (6.5-8.0) and 0.67 (0.58-0.75) hours, respectively. Celsior® fluid was used for organ preservation in 130/131 (99.2%) organs (the other used was Belzer® fluid). No organs were subjected to normo- or hypothermic automatic perfusion before implantation.
Taking into account the 8 donors’ characteristics defined previously, median (IQR) overall DRI was 1.96 (1.67-2.16). Median DRI was similar between patients with a viable graft over 1 year following index LT and others (1.96 vs. 1.98; p = 0.48). Furthermore, median DRI was also similar between patients retransplanted over 1 year and others (1.96 vs. 1.96; p = 0.83). All characteristics of LT donors are depicted in Table 2.
Table 2 Characteristics (n (%) or median (IQR)) of donors stratified by graft survival status at 1 year post LT (n = 131).
Perioperative Characteristics
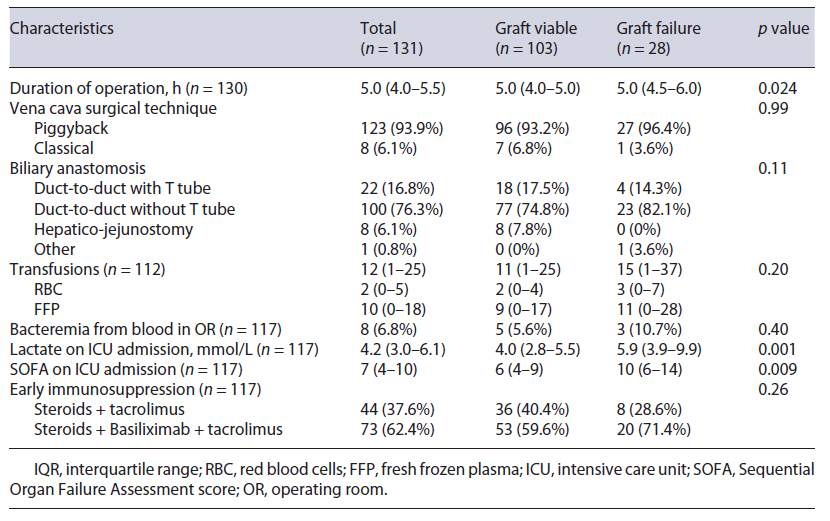
Median (IQR) time of LT procedure was 5.0 (4.0-5.5) hours. Vena cava piggyback technique was performed in 123/131 (93.9%) patients. A duct-to-duct biliary anastomosis was used in 122/131 (93.1%) cases. A median (IQR) of 2 (0-5) units of red blood cells and 10 (0-18) units of fresh frozen plasma were required in the operating room. Bacteremia was identified in the blood collected in the operating room in 8 (6.8%) patients. Upon ICU admission following surgery, median (IQR) lactate and SOFA score were 4.2 (3.0-6.1) mmol/L and 7 (4-10), respectively. Early immunosuppression regimen included induction with basiliximab in 73/117 (62.4%) patients. All perioperative characteristics are depicted in Table 3.
Table 3 Perioperative characteristics (n (%) or median (IQR)) stratified by graft survival status at 1 year post LT (n = 131)
Clinical Outcomes
Among 116 patients who underwent LT during 2019 at CCH, 15 (12.9%) required retransplantation and 103 (88.8%) were alive within 1 year of index LT (online suppl Fig. S2). None of these patients who underwent retransplantation died up to year following index LT. Therefore, graft survival at 1 year following index LT was 78.6% (103/131). The causes of retransplantation within 1 year of index LT were as follows: hepatic artery thrombosis in 8 patients, stenosis of the biliary anastomosis in 4, intrahepatic abscesses in 1, primary non-function in 1, and piggyback syndrome in another one. The causes of mortality within 1 year of index LT were as follows: hemorrhagic shock in 6 patients, liver-related multiorgan failure in 3, septic shock in 2, and stroke in 2. Overall, median (IQR) hospital LOS was 22 (13-37) days.
The Adjusted Association of DRI with Endpoints
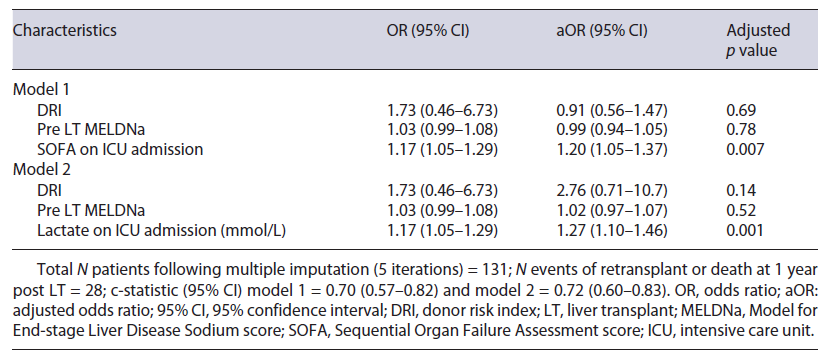
Using logistic regression, following adjustment for pre LT (MELDNa score) and perioperative (SOFA score or lactate on ICU admission) characteristics, DRI was not associated with 1-year graft failure (Table 4: adjusted odds ratio [aOR] and 95% confidence interval [CI] = 0.91 [0.56-1.47] for model one [p = 0.69] or 2.76 [0.71-10.7] for model 2 [p = 0.14]). In fact, only higher SOFA score (aOR [95% CI] = 1.20 [1.05-1.37]; p = 0.007) or lactate (aOR [95% CI] = 1.27 [1.10-1.46]; p = 0.001) on ICU admission were independently associated with higher odds of 1-year graft failure. Furthermore, the discriminative ability of both models was reasonably good (c-statistic [95% CI] = 0.70 [0.57-0.82] for model one and 0.72 [0.60-0.83] for model 2).
Table 4 Study of associations of covariates with graft failure at 1 year post index LT by multivariate logistic regression
Using logistic regression, both on unadjusted (OR [95% CI] = 1.08 [1.00-1.17]; p = 0.005) and adjusted (for SOFA score: aOR [95% CI] = 0.99 [0.89-1.10]; p = 0.88) analyses, the balance of risk score (includes donor and recipient’s characteristics) was also not associated with 1-year graft failure.
Using linear regression, both on unadjusted (regression coefficient [95% CI] = 2.18 [-8.49 to 12.84]) and adjusted (for MELDNa and SOFA scores: regression coefficient [95% CI] = 1.82 [-9.10 to 12.74]) analyses, DRI was not associated with hospital LOS.
Discussion
Key Results and Comparisons with Previous Literature
In a recent Portuguese cohort of patients who underwent cadaveric donor LT, median DRI was as high as 1.96, but it was not associated with graft failure at 1 year post index LT. In fact, only perioperative characteristics, such as SOFA score or lactate on ICU admission post index LT, were independently associated with 1-year graft failure.
Over the past few decades, reports have documented that given the scarcity of organs and the increasing competence in performing LT internationally, centers have been accepting more frequently extended criteria donors with good post LT outcomes [1, 13, 14]. In our cohort, 47.3% of all donors were ≥65 years old, a unique criterium often used to define marginal donors [1]. Therefore, we were expecting to find a high median DRI (1.96). Fortunately, this did not apparently translate into poorer post LT outcomes, namely the 1-year graft survival. The fact that our LT program has been running for >25 years and currently with >100 procedures performed annually may help to explain the increasing competence in using and taking advantage of such marginal donors at CCH [13]. However, we still observed a retransplantation rate of 12.9% within 1 year post index LT, which signals a window of opportunity for potential improving graft’s longevity, especially in terms of prevention and treatment of the hepatic artery thrombosis.
Several studies have tried to evaluate the impact of recipient or perioperative factors on post LT outcomes besides donor characteristics [7, 8, 15-19]. In our cohort, among pre LT, operative, or early post LT characteristics, only higher SOFA score or lactate on ICU admission following index LT were independently associated with higher odds of 1-year graft failure.
SOFA score has been widely used to quantify organ failure severity in general critically ill patients [20]. Therefore, we would expect SOFA score to capture the severity of illness in patients who underwent a complex transplant procedure, often with aggressive ongoing organ support measures. This complexity may result from preoperative clinical instability, surgical complications, or even post reperfusion graft malfunctioning. Much in the same way, lactate is a known good marker of ongoing physiological stress, whether caused by transient hypovolemia or shock [21]. Furthermore, a poorly working liver will not clear lactate appropriately. In fact, worse post LT lactate clearance has been associated with poorer post LT outcomes [18, 19].
Taking into account all of our findings, we should make the following remarks. Firstly, while DRI may be useful to compare specific donors’ characteristics, especially for high-risk donors, in our cohort, its prognostic value was poor. However, DRI may be potentially improved by including other relevant donor factors, for example the degree of liver steatosis [6]. Secondly, the overall severity of illness immediately following LT effectively impacted 1-year graft failure. Therefore, understanding, preventing, and timely treating organ failures during and following transplant surgery could be important to improve patients’ outcomes.
Limitations
The interpretation of our results should take into account the following limitations. Firstly, this was a single-center retrospective study, therefore it may have been prone to selection bias. Certainly, there are specific features of every LT center. However, the high volume of transplant procedures at CCH and the extensive characterization of both recipients and donors may have helped to mitigate that risk. Secondly, the overall rate of missing values may have interfered with the final modeling performed. However, we think that the multiple imputation strategy used, as per suggested recommendations, may have helped to mitigate that effect [22]. Thirdly, other donors’ characteristics may have an impact on the graft quality, for example the degree of liver steatosis or retrieval techniques. Unfortunately, we were unable to collect data on further features that could help to better characterize accepted grafts. Fourthly, based on previous literature, we only analyzed clinical outcomes up to 1 year following index LT. However, it may be of interest to understand if donors’ features may impact long-term results, for example at 5 years post LT (criterion of futility of transplant).
Despite these limitations, we think our study adds to the literature dedicated to study the factors that may influence post LT outcomes. In fact, it tries to recognize the multiple factors possibly involved in a complex interconnected way, while highlighting the relevance of the overall severity of illness immediately upon LT. In future studies, to further characterize what happens in the operating room during LT, for example the number and severity of ensuing organ failures, may shed some additional light on the prognosis of LT recipients.
Conclusions
In a recent Portuguese cohort of patients who under-went LT, DRI was high. While DRI was not associated with 1-year graft failure, SOFA score or lactate on ICU admission post LT were.
Acknowledgments
The authors acknowledge the Portuguese Institute of Blood and Transplantation, and the Liver Failure Study Group of the Portuguese Society of Intensive Care Medicine.















